Reproductive Endocrinology and Infertility
Amenorrhea is classified into primary and secondary types with different causes like physiological and pathological factors affecting the hypothalamus, pituitary, ovaries, and uterus. Understanding the reasons behind amenorrhea is crucial due to its implications on fertility, estrogen deficiency-related health risks, and potential link to endometrial cancer.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Reproductive Endocrinology and Infertility Reproductive Endocrinology and Infertility Mihretu Molla (Bsc, Msc)
Presentation outline Amenorrhea Menopause Infertility
Amenorrhea Definition and classification Amenorrhea is defined as the absence of menstruation at any time between the usual ages of puberty and menopause. Primary amenorrhea is the absence of spontaneous menses by age 16 regardless of the presence of secondary sexual characteristics or absence of both by age 14. Secondary amenorrhea:- is the absence of menses for more than or equal to 6 months in a woman with regular cycles or for a period of more than 3 cycles length in women with irregular cycle. 3
Causes of amenorrhea 1.Physiological amenorrhea:- result from pregnancy, lactation, prior or directly after menopause. (90-95%). 2.Pathological amenorrhea:- result from pathologic conditions affecting the hypothalamus, pituitary, ovaries, uterus and the outflow tract. (5-10%). It is sub divided into:- Hypogonadotropic, Hypergonadotropic Eungonadotropic. 4
Cont-- Hypogonadotropic:- amenorrhea:- Hypothalamic causes like stress, acute weight loss, anorexia nervosa and strenuous exercise. Drugs like psychotropic drug, drug addiction , post pill amenorrhea and absences of GnRH. 5
cont- Pituitary causes:- include hyper prolactinemia, damage to the pituitary, postpartum ischemic and necrosis. Hypergonadotrophic amenorrhea:- -This results from congenital (primary) or acquired (secondary) ovarian failure. 6
Eungonadotrophic amenorrhea:- Uterovaginal causes include congenital absence or acquired distruction of the endometrium. Conditions that are associated with obstruction of menstrual blood flow like:- - Cervical and vaginal atresia. - Transverse vaginal septum . - Imperforate hymen and others. 7
Importance:- Amenorrhea is important for several reasons:- Failure to ovulate causes infertility Prolonged estrogen deficiency result in health hazards Amenorrhea with some estrogen production can predispose to endometrial cancer. Primary amenorrhea in a girl who has not already developed secondary sexual characteristics may give rise to major social and psycho sexual problems. 8
Diagnosis:- In the majority of the cases, diagnosis is reached by history, physical examination and simple laboratory investigation. Few need sophisticated and expensive investigation. Investigation:- Initially pregnancy must be ruled out, then depending on the type of amenorrhea and the clinical findings the following can be done:- 9
Cont-- - Hormone assays:- prolactin, LH,FSH, thyroid hormones - Ultrasound, skull X-ray and other imaging techniques - Buccal smear for sex chromosomal analysis 10
Work up of secondary amenorrhea 1 .Rule out pregnancy by history, physical examination and urine HCG. 2. Perform progestin challenge test let medroxy progestrone acetate 10mg for 5 days Presence of withdrawal bleeding (positive test) after 2-7 days signifies normal estrogen primed endometrium, normal outflow tract and absence of endogenous progesterone (anovulation) 11
Cont-- Absence of withdrawal bleeding (negative test) signifies absence of estrogen primed endometrium which may result from either faults in the Hypothalamus or Pituitary or Ovary or Endometrium or Outflow tract. Further test is needed to differentiate 12
3. Perform combined estrogen-progesterone challenge test by giving drugs like combined oral contraceptives. Presence of withdrawal bleeding (positive test) indicates absence of endogenous estrogen and progesterone arising either from ovarian failure or hypothalamus or pituitary failure. To determine LH/FSH levels. Low FSH/LH levels diagnose hypothalamus -pituitary failure and high levels diagnose ovarian failure. 13
Cont-- Absence of withdrawal bleeding (negative test) indicates either obliteration of the endometrium (Ashermans syndrome) or destruction/atrophy of endometrium. To differentiate these hysterosalpingography is needed. 14
Work of primary amenorrhea 1.Check for secondary sexual characteristics 2.If secondary sexual characteristics of feminizing type are present, check the vagina and for pelvic mass. -If there is bluish membrane which bulges with straining and associated pelvic mass imperforate hymen 15
Cont-- - If there is a blind ending vagina with pelvic mass- transverse vaginal septum - If vaginal canal close not exist and there is pelvic mass- isolated vaginal agenesis - Normal vagina with absent cervical Os and associated pelvic mass- cervical atresia. 16
Cont-- If there is a blind ending vagina without pelvic mass, two possibilities exist which can be differentiated by barr body determination. These are androgen insensitivity syndrome (barr body negative and presence of inguinal mass) and mullerian agenesis (barr body positive) . 17
Climacteric and Related Problems Definitions:- Climacteric is the phase of life for women that marks transition being able to reproduce to being non-reproductive. Menopause is cessation of physiological uterine bleeding. -It is the most visible event marking climacteric. - The average age is 51 years - It is not affected by race, number of pregnancy contraceptive use, age at menarche and physical characteristics 18
Pre-menopause:- is the period before menopause during which the menstrual cycle is irregular. Post menopause:- is the period after menopause. Pathophysiolgy of menopause -As menopause nears, ovarian follicles get depleted and - Become resistant to gonadotrophic hormones. - Estradiol production which in turn FSH and later level of LH - 19
Cont-- - Anovulation or oligoovulatory result menses irregularity - Later, there will not be any follicles to be stimulated by high level of gonadotrophins result in significant drop in estrogen to a level that is not capable of stimulating the endometrium causing menopause. 20
Change in menopause I. Hormonal changes II. Change in reproductive organs:- -Atrophy of the vagina thinning of the epithelium and flattening of rugae. - Atrophy of cervix reduce in size -vaginal dryness - Uterus decreased in size 21
Cont-- - The ovaries decreased in size and not palpable - Supporting strictures lose their tons - The labia lose fat and flatten III. Change in the menstrual cycle IV. Change in other organs 22
Problems of Menopause These is mainly related to estrogen deficiency and rarely to estrogen excess. Hot flush:- vasomotor disturbance consisting of sudden flushing i.e feeling of heat or burning in the face, neck and chest, followed by outbreak of sweating to whole body. -These women suffer from insomnia. - As a treatment for sever cases conjugated estrogen or progestin is recommended. 23
Osteoporosis:- is the most important health hazard of menopause. It affects the trabecular bone. -It may end up in pathologic fracture of the spines and the other bones. - Diagnosis needs special imaging investigation. - Treatment is estrogen replacement. - The prevention is estrogen replacement, exercise and adequate calcium intake. 24
Cont-- Dysparunia:- arises from vaginal dryness and atrophic vaginitis. - Local treatment with estrogen cream relieves the problem. 25
Psychological problems:- May arise from estrogen deficiency or from the effects of other menopausal problems (hot flush and dysparunia). -Symptoms include anxiety, insomnia, irritability, depression and mood changes. Post menopausal bleeding -It is defined as vaginal bleeding after 6 months of menopause. - It is an abnormal condition that always needs proper investigation. - It could arise from benign or malignant conditions. 26
-Postmenopausal bleeding should be considered as a manifestation of malignant condition unless proved . The causes are:- - Atrophic vagina - Atrophic endometritis - Cervical cancer - Endometrial hyperplasia and polyps - Endometrial cancer - Sarcoma of the uterus - Vulval or vaginal cancer N.B All postmenopausal bleeding should be referred. 27
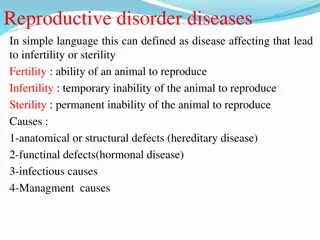
Infertility Infertility: is inability to conceive after 1 year of unprotected intercourse of reasonable frequency. Most couples are more correctly considered to be subfertile, rather than infertile, as they will ultimately conceive if given enough time. This concept of subfertility can be reassuring to couples. Sterility: incapable of becoming pregnant or of inducing pregnancy Infertility is a common condition, affecting 10 to 15 % of reproductive- aged couples.
Infertility contd. Two types of infertility Primary infertility: no prior pregnancies Secondary infertility: infertility following at least one prior conception. Fecundability Is the ability to conceive in a single cycle , the monthly probability of conceiving is 20 to 25 %. In people attempting conception, approximately 50 % of women will be pregnant at 3 months, 75 % will be pregnant at 6 months, and > 85 % will be pregnant by 1 year. Fecundity is the ability to achieve alive birth within one menstrual cycle (0.15-0.18)
Etiology of Infertility Successful pregnancy requires a complex sequence of events including: Patent out flow tract Ovulation Sperm of adequate number & quality Ovum pick-up by a fallopian tube Fertilization Transport of a fertilized ovum into the uterus Receptive endometrial cavity. Infertility can be seen as male & female infertility
Etiology contd. Female infertility Male factors Ovulatory Dysfunction Tubal /Peritoneal Factor Uterine Factor Cervical Factors Vaginal Factors Chronic systemic diseases Social personal habit(illicit drugs) Unexplained Pre-testicular Testicular Post-testicular Idiopathic
Etiology contd. Etiology of Infertility Ovulatory dysfunction 27% Male factor 25% Tubal/uterine factors 22% Unexplained infertility 17% Other 9%
Ovulatory Dysfunction Ovulation may be perturbed by abnormalities within the hypothalamus, anterior pituitary, or ovaries. Hypothalamic disorders may be due to lifestyle, for example, excessive exercise, eating disorders, or stress. Alternatively, idiopathic hypothalamic hypogonadism (IHH) or Kallman syndrome may be the cause. Thyroid disease and hyperprolactinemia may also contribute to menstrual disturbances
Ovulatory contd. Treatment of ovulatory dysfunction is ovulation induction Drugs used for ovulation induction Clomiphene citrate hMG FSH hcG GnRH GnRH analogs
Tubal/Peritoneal Factor Damage or obstruction of fallopian tube Previous PID Previous tubal surgery Ectopic pregnancy Benign polyps Tubal endometriosis Mucus debris Tubal damage of unknown cause-sub clinical infection Peritubal/periovarian adhesions PID Pelvic Surgery Endometriosis
Tubal/ peritoneal contd. Symptoms such as chronic pelvic pain or dysmenorrhea may suggest the presence of tubal obstruction or pelvic adhesions or both. Adhesions can prevent normal tubal movement, ovum pick-up, and transport of the fertilized egg into the uterus. Tubal infertility has been estimated to follow in 12 percent, 23 percent, and 54 percent of women following one, two, or three cases of PID, respectively Testing for tubal patency can be performed by Rubin test hysterosalpingography (HSG), Falloposcopy , Salpingoscopy or by chromotubation during laparoscopy.
Tubal/ peritoneal Contd. Treatment of tubal and peritoneal factors is done via tuboplasty which includes 1. Adhesiolysis 2. Fimbrioplasty 3. Sapingostomy 4. Tubal anastmosis 5. Tubo-cornual anastmosis
Tubal/ peritoneal contd. Possible mechanisms of endometriosis to cause infertility are: a. Pelvic adhesions altered tubal motility - dysparunea b. Increased macrophage activity Sperm phagocytosis c. Altered immune response - interfere uterine nidation - early fetal wastage d. Prostaglandin secretion ovulatory dysfunction - altered tubal motility
Uterine Factor Uterine causes of infertility include Congenital malformation didelphys, unicornute, septate Luteal phase defect Endometritis Tuberculosis Endometrial polyps Leiomyoma large, solitary, submucous, distorting cavity Asherman s syndrome In utero exposure to DES
Uterine Factor contd. There are five major approaches for evaluating pelvic anatomy: 1. Hysterosalpingography 2. Transvaginal sonography with or without saline instillation 3. Hysteroscopy 4. Laparoscopy, and 5. MRI
Cervical Factors The cervical glands secrete mucus that is normally thick and impervious to sperm and ascending infections. High estrogen levels at midcycle change the characteristics of this mucus, and it becomes thin and stretchy. Estrogen-primed cervical mucus filters out nonsperm components of semen and forms channels that help direct sperm into the uterus. Midcycle mucus also creates a reservoir for sperm, allowing ongoing release during the next 24 to 72 hours and extending the potential time for fertilization.
Cervical Factors contd. Abnormalities in mucus production are secondary to Cryosurgery, cervical conization, or a loop electrosurgical excision procedure (LEEP) for an abnormal pap smear Cervical infection (Chlamydia trachomatis, Neisseria gonorrhoeae & Ureaplasma urealyticum) Abnormalities of cervical factor can be assessed by postcoital test
Unexplained No obvious cause for infertility following all standard investigations i.e. semen analysis, ovulation detection, tubal &peritoneal factors, endocrinopathy & post-coital test With expectant management, 60 % conceive in three years
Male factor Etiology of Male Infertility Etiology of infertility Site of dysfunction Prevalence % Pre-testicular Hypothalamic / pituitary Testis 1 -2 Testicular 30 - 40 Post-testicular defects Ducts of sperm 10 - 20 transport ----- Idiopathic 40 -50
Etiology of Male Infertility contd. 1. Pre-testicular causes Are hypothalamic & pituitary disease a. Congenital disorders Kallmann's syndrome b. Acquired diseases Tumors Infiltrative diseases Chronic disease Hyperprolactinemia Drugs 47
Etiology of Male Infertility contd. 2. Testicular Causes Congenital disorders Y chromosome defects Cryptorchidism Varicoceles Acquired disorders Infection Drugs Radiation Environmental factors Smoking Systemic disorders 48
Etiology of Male Infertility contd. 3. Post-testicular causes Congenital or acquired disease in the ductal system of a male Absence, dysfunction, or obstruction of the epididymis Bilateral obstruction, ligation, or altered peristalsis of the vas deferens 49
Etiology of Male Infertility contd. 4. Idiopathic male infertility Despite careful assessment of all possible causal mechanisms, a cause of abnormal sperm number, morphology or function cannot be identified in a substantial proportion of infertile men. There are also men who have repeatedly normal semen analyses but cannot impregnate an apparently normal female partner.