Spirochetes and Borrelia: Characteristics, Classification, and Syphilis
Explore the world of spirochetes and Borrelia in this lecture, focusing on their genus identification, chemical tests, special procedures for viewing, classification, and the causative agent for syphilis. Learn about the general characteristics of spirochetes, differentiating between pathogenic and non-pathogenic species, and the stages of venereal syphilis.
Uploaded on | 1 Views
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
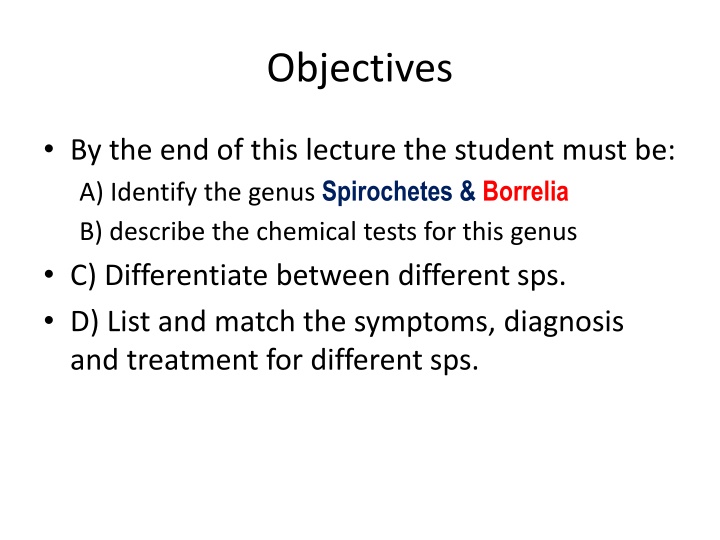
Objectives By the end of this lecture the student must be: A) Identify the genus Spirochetes & Borrelia B) describe the chemical tests for this genus C) Differentiate between different sps. D) List and match the symptoms, diagnosis and treatment for different sps.
General characteristics Spirochetes Tiny (0.2 W x 6-20 m L), thin walled, flexible, spirals (helical) that like corkscrew They are coiled into regular helices (6-14/cell) Move in a unique spinning fashion via 6 thin endoflagella called axial filaments Flagella lie between outer membrane & PDG layer Gram negative Too small to be seen using the light microscope 2
Special procedures are required to view spirochetes Dark field microscopy Immunofluorescence Silver stain (Fontana s silver or Giemsa s stain) Pathogenic species do not grow on artificial media While non-pathogenic species can be grow Can be propagate some strains of spirochetes by inoculating it into the testes of the living rabbit 3
Classification of Spirochetes Human pathogens belong to following 3 genera: 1. Treponema 2. Leptospira 3. Borrelia Others (saprophytes) are found in water, sewage & in mouth & genital tracts of humans 4
Treponema pallidium The causative agent for STD syphilis Syphilis is either 1. Acquired (STD, Venereal) Transmitted from infected skin or mucous membrane (genitalia, mouth, rectum) to other person by intimate contact 2. Congenital Transmitted from pregnant women to their fetus 3. Blood transfusion Rarely reported Men are more susceptible to contract syphilis than women Marked increase in syphilus in homosexual men 5
Stages of venereal syphilis A. Primary syphilis Primary lesion is Hard chancre Develop on genitals in 10-90 day Chancre heals spontaneously in 3-12 week without scar Enlargement of lymph nodes on genital organs Firm, painless, indurated & ulcerated lesion; covered with a thick exudate rich in spirochetes Highly infectious Spirochetes spread widely in tissue leading to 2ry syphilis 6
Stages of venereal syphilis Secondary syphilis Most infectious stage Untreated patient enters bacteremic or 2ry syphilis 1-3 months later, secondary lesions may appear T. pallidium multiply and spread via blood This stage is systematic and characterized by Generalized lymphadenopathy Maculopapular skin rashes on the body & condylom latum (wart) at mucocutaneous junctions Lesions heal spontaneously over 6 week and yet the disease may progress latency & then to tertiary stage B. 7
Stages of venereal syphilis Latent Syphilis Most patients are asymptomatic during this period Early latent period Last for 1-2 years after the 2nd stage 25% of patient develop symptoms of 2ry syphilis Patient can infect other Late latent period Last for many years No symptoms occur and patients are not infectious 30% of untreated patients slowly progress to 3ry syphilis The rest will remain asymptomatic 8
Stages of venereal syphilis C. Tertiary syphilis Develops over 6-40 year with slow inflammatory damage to organs, blood vessels & nerve cells It can be grouped into 3 general categories 1. Gummatous syphilis Occurs 10 year after 1ry stage in 10% of untreated May show localized granulomatous lesions (gumma) which eventually necrosis and become fibrotic Noninfection lesion are found mainly in skin & bones 9
Stages of venereal syphilis 2. Cardiovascular syphilis 3-10 year after 1ry stage in 15% of untreated patients Characterized by aortic aneurysm & necrosis in aorta 3. Neurosyphilis (Late tertiary or quaternary syphilis) Occurs 10-20 yearin 8% of untreated patients Asymptomatic neurosyphilis, subacute meningitis, brain infarction, mental deteriorations & psychiatric symptoms In 3ry lesion , T. pallidium are rarely seen 10
Congenital syphilis Transplacental spread of T. pallidium after the 1st trimester of pregnancy may result in Fetal death Prematurity or Congenital syphilis The early syndrome may not present at birth, only developing during the subsequent 4 weeks They are characterized by Generalized rash resemble 2nd acquired syphilis Enlargement of the liver, spleen and lymph nodes Congenital syphilis leaves residual characteristic sign Hutchinson s teeth Saddle nose or nose deformity 11
Immunity of syphilis Immunity of T. pallidium is incomplete Antibodies do not stop the progression of the disease Treated syphilitic Patient can contract syphilis again Late syphilitic patient is relatively resistant to reinfection The antigens of T. pallidium induce Specific antibodies (non-treopenemal); detected by immuno-fluorescence or hemagglutination tests Nonspecific antibodies (reagin): detected by the flocculation of cardiolipin extracted from beef heart tissues Both specific and non-specific antitreponemal antibodies are used in serological diagnosis of syphilis 12
Diagnosis of Syphilis Syphilis is confirmed by Finding T. pallidium in exudates from the lesions Or by detection of antibodies in the serum During t 1ry and 2ry stages spirochetes are demonstrated in the early lesions in wet preparation by dark field or immunfluorescense microscopy Stained with either Fontana or Giemsa stain Not seen on a Gram-stained smear During 2ry & 3ry syphilis can be detected serologically 13
Serological Tests of Syphilis Patients develop 3 types of antibodies 1st is known as a lipoidophil antibody called regain Tests depend on the detection of regain Non-specific test/Standard Tests for Syphilis (STS) STS used for routine screening STS involves use of non-treponemal antigens (Cardiolipin) which react with regain in patient s serum Can be demonstrated by CFT (Wassermann test) or by Flocculation Tests such as Venereal Disease Research Laboratory (VDRL) or Rapid Plasma Regain (RPR) test 14
Serological Tests of Syphilis 2nd antibody called Reiter which react with a protein component found in non-pathogenic T.reiter This test called Group specific test Demonstrated by Reiter Protein CFT This test is more specific than the STS but gives fewer false positive results 15
Serological Tests of Syphilis 3rd type of antibody reacts directly with T. pallidium These tests are specific Using Nichol s strain It can be demonstrated by T. pallidium Immobilization (TPI) test, Fluorescent Treponemal Antibody (FTA) test and T. pallidium Haemagglutination (TPHA) test This test is the most specific tests 16
Prevention, Control & Treatment There is no vaccine against syphilis This disease is controlled by Early diagnosis and appropriate treatment Use of condoms Follow-up of infected individuals & their contacts This disease is treated by Penicillin Tetracycline or Erythromycin can be used in allergic patients to Penicillin 17
Non-venereal Treponema There are three subspecies of T. pallidium T. pallidium subspecies endemicum It causes endemic syphilis (Bejel) T. pallidium subspecies pertenue It causes yaws T. pallidium subspecies carateum It causes pinta 18
Borrelia causing diseases Borellia Causing Relapsing Fever Lyme B. burgdorferei Endemic (Africa) Shorter febrile period More relapses Endemic (European) Longer febrile period Fewer relapses B. duttoni B. recurrentis Transmitted by Ticks Transmitted by Lice 19
Main differences between the two types of relapsing fever European or louse-borne type West African or Tick-borne type Caused by B. recurrentis B. duttoni Transmitted by body louse Tick Often appears in epidemics Endemic Long febrile period and fewer relapses Spirochetes not transmitted to louse progeny Shorter febrile and more relapses Transmitted to tick progeny 20