STEMI: Diagnosis and Management
Acute coronary syndromes, specifically ST-elevation myocardial infarction (STEMI), present with chest pain, nausea, and other symptoms. Diagnosis involves history, ECG, and biochemical markers. Different techniques like pathology, biochemistry, ECG, and imaging aid in confirming myocardial infarction. Revised criteria outline the diagnosis of acute, evolving, or recent MI based on specific markers and symptoms.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Acute coronary syndromes ST elevation myocardial infarction (STEMI)
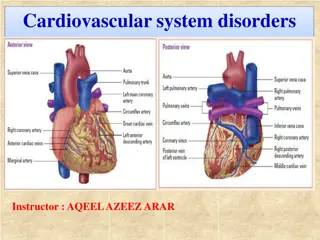
ST elevation myocardial infarction (STEMI) Patients with ACS who have ST-segment elevation or new left bundle branch block (LBBB) on their presenting ECG benefit significantly from immediate reperfusion and are treated as one group under the term ST- elevation myocardial infarction (STEMI).
ANT.WALL STEMI LEFT BANDLE BRANCH BLOCK
Presentation Chest pain is usually similar in nature to angina, but of greater severity and longer duration and is not relieved by sublingual (SL) nitroglycerin. Associated features are nausea and vomiting, sweating, breathlessness, and extreme distress. The pain may be atypical (e.g., epigastric) or radiate to the back. Diabetics, elderly, women, or hypertensive patients may suffer painless ( silent infarcts) and/or atypical infarction. Presenting features include breathlessness from acute pulmonary edema, syncope or coma from arrhythmias, acute confusional states (mania/psychosis), diabetic hyperglycemic crises, hypotension or cardiogenic shock, central nervous system (CNS) manifestations resembling stroke secondary to sudden reduction in cardiac output, and peripheral embolization.
STEMI: diagnosis STEMI diagnosis is based on a combination of history, ECG, and biochemical markers of cardiac injury. In practice, history and ECG changes are diagnostic. Biochemical markers of cardiac injury usually become available later and help reconfirm the diagnosis and provide prognostic information (magnitude of rise).
-- Aspects of Diagnosis of Myocardial Infarction by Different Techniques Pathology Myocardial cell death Biochemistry Markers of myocardial cell death recovered from blood samples Electrocardiography Evidence of myocardial ischemia (ST and T wave abnormalities) Evidence of loss of electrically functioning cardiac tissue (Q waves) Imaging Reduction or loss of tissue perfusion Cardiac wall motion abnormalities
Revised Definition of Myocardial Infarction (MI) Criteria for Acute, Evolving, or Recent MI Either of the following criteria satisfies the diagnosis for acute, evolving, or recent MI: 1. Typical rise and/or fall of biochemical markers of myocardial necrosis with at least one of the following: a) Ischemic symptoms b) Development of pathological Q waves in the ECG c) ECG changes indicative of ischemia (ST segment elevation or depression) d) Imaging evidence of new loss of viable myocardium or new regional wall motion abnormality 2. Pathological findings of an acute myocardial infarction
Criteria for Healing or Healed Myocardial Infarction Any one of the following criteria satisfies the diagnosis for healing or healed myocardial infarction: 1. Development of new pathological Q waves in serial ECGs. The patient may or may not remember previous symptoms. Biochemical markers of myocardial necrosis may have normalized depending on the length of time that has passed since the infarction developed. 2. Pathological findings of a healed or healing infarction
ECG changes ST-segment elevation occurs within minutes and may last for up to 2 weeks. ST elevation of 2 mm in adjacent chest leads and 1 mm in adjacent limb leads is necessary to fulfill thrombolysis criteria. Persisting ST elevation after 1 month suggests formation of LV aneurysm. Pathological Q waves indicate significant abnormal electrical conduction but are not synonymous with irreversible myocardial damage. In the context of a transmural infarction the Q waves may take hours or days to develop and usually remain indefinitely. In the standard leads, the Q wave should be 25% of the R wave, 0.04 s in duration, with negative T waves. In the precordial leads, Q waves in V4 should be >0.4 mV (4 small sq) and in V6 >0.2 mV (2 small sq), in the absence of LBBB (QRS width <0.1 s or 3 small sq). ST-segment depression in a second territory (in patients with ST-segment elevation) is secondary to ischemia in a territory other than the area of infarction (often indicative of multivessel disease) or reciprocal electrical phenomena. Overall, it implies a poorer prognosis. T-wave inversion may be immediate or delayed and generally persists after the ST elevation has resolved.
Localization of infarcts from ECG changes Anterior Anterseptal Lateral inversion/ST elevation/Q waves in I and aVL Inferoseptal ST elevation and/or Q waves in II, III, aVF, and 5 V6 (sometimes I and aVL) True posterior Tall R waves in V1 V2 with ST depression in V1 V3. T waves remain upright in V1 V2. This can be confirmed with an esophageal lead if available (method similar to an NG tube). This usually occurs in conjunction with an inferior or lateral infarct RV infarction ST-segment elevation in the right precordial leads (V3R V4R). Usually found in conjunction with inferior infarction. This may only be present in the early hours of infarction ST elevation and/or Q waves in V1 V4/V5 ST elevation and/or Q waves in V1 V3 ST elevation and/or Q waves in V5 V6 and T-wave
Conditions that may mimic ECG changes of a STEMI Left or right ventricular hypertrophy LBBB or left anterior fascicular block Wolff Parkinson White syndrome Pericarditis or myocarditis Cardiomyopathy (hypertrophic or dilated) Trauma to myocardium Cardiac tumors (primary and metastatic) Pulmonary embolus Pneumothorax Intracranial hemorrhage Hyperkalemia Cardiac sarcoid or amyloid Pancreatitis
Biochemical markers of cardiac injury CK (creatine kinase) Levels twice the upper limit of normal are considered abnormal. Serum levels rise within 4 8 hours post-STEMI and fall to normal within 3 4 days. The peak level occurs at about 24 hours but may be earlier (12 hours) and higher in patients who have had reperfusion (thrombolysis or percutaneous coronary intervention [PCI]). False-positive rates of ~15% occur in patients with alcohol intoxication, muscle disease or trauma, vigorous exercise, convulsions, IM injections, hypothyroidism, pulmonary embolism (PE), and thoracic outlet syndrome. CK-MB isoenzyme is more specific for myocardial disease. Levels may be elevated despite a normal total CK. However, CK-MB is also present in small quantities in other tissues (skeletal muscle, tongue, diaphragm, uterus, and prostate) and trauma or surgery may lead to false-positive results. If there is doubt about myocardial injury with CK-MB levels obtained, a cardiac troponin must be measured.
Cardiac troponins ( Tn T ,Tn I ) Both TnT and TnI are highly sensitive and specific markers of cardiac injury. Serum levels start to rise by 3 hours post-MI and elevation may persist up to 7 14 days. This is advantageous for diagnosis of late MI. In most STEMI cases, the diagnosis can be made using a combination of the clinical picture and serial CK/CK-MB levels. In the event of normal CK-MB levels and suspected noncardiac sources of CK, troponins can be used. Troponins can also be elevated in non ischemic myocyte damage, such as myocarditis, cardiomyopathy, and pericarditis. Other markers There are multiple other markers, but with increasing clinical availability of Troponin, measurements of these markers are not recommended. These include aspartamine transferase (AST) (rise 18 36 hours post-MI) and lactate dehydrogenase (LDH) (rise 24 36 hours post-MI).
Biomarker Begins to rise Peak value Returns to normal Myoglobin 1-2 hours 6-8 hours 1-2 days CK-MB 2-6 hours 16-20 hours 1-2 days CK 4-8 hours 16-24 hours 3-4 days Trop T 4-6 hours 12-24 hours 7-10 days AST 12-24 hours 36-48 hours 3-4 days LDH 24-48 hours 72 hours 8-10 days
Factors associated with a poor prognosis Age >70 years Previous MI or chronic stable angina Anterior MI or right ventricular infarction Left ventricular failure at presentation Hypotension (and sinus tachycardia) at presentation Diabetes mellitus Mitral regurgitation (acute) Ventricular septal defect
Treatment of STEMI Diagnosis is normally made on presentation (history and ECG changes of ST elevation /new LBBBB )followed by rapid stabilizing measures to ensure institution of reperfusion therapy without delay. This is in contrast to NSTEMI/UA, where diagnosis may evolve over a period of 24 72 hours. (Reperfusion must not be delayed to wait for biochemical markers.) All patients with STEMI should be admitted to an intensive care unit (ICU), e.g., coronary ICU (CICU). Stabilizing measures are generally similar for all ACS patients. All patients with suspected STEMI should have continuous ECG monitoring in an area with full resuscitation facilities. Patients should receive immediate aspirin 325 mg po plus one of thyenopyridine antiplatlets (if no contraindications) , analgesia, and oxygen. Secure IV access. Conduct rapid examination to exclude hypotension, note the presence of murmurs, and identify and treat acute pulmonary edema. Right ventricular failure (RVF) out of proportion to left ventricular failure (LVF) suggests RV infarction.
Control of cardiac pain Morphine 2.5 10 mg IV is the drug of choice and may be repeated to ensure adequate pain relief, unless there is evidence of emerging toxicity (hypotension, respiratory depression). Nausea and vomiting should be treated with metoclopramide (10 mg IV) or a phenothiazine. Oxygen should be administered at 2 5 L/min for at least 2 3 hours. Hypoxemia is frequently seen post-MI due to ventilation perfusion abnormalities secondary to LVF. In patients with refractory pulmonary edema, endotracheal intubation may be necessary. Beware of CO2 retention in patients with COPD. Nitrates may lessen pain and can be given (sublingual or IV) provided that the patient is not hypotensive. These drugs should be used cautiously in inferior STEMI, especially with right ventricular infarction, as venodilation may decrease RV filling and precipitate hypotension. Nitrate therapy has no demonstrated effect on mortality (ISIS-4). Correction of electrolytes Both low potassium and low magnesium may be arrhythmogenic and must be supplemented, especially in the context of arrhythmias.
Strategies to limit infarct size B-Blockade Early B-blockade has been shown to be beneficial by limiting infarct size, reducing mortality, and decreasing early malignant arrhythmias. All patients (including primary PCI and thrombolysis patients) should have early B-blockade. Patients with the following features may benefit most from B-blocker therapy: Hyperdynamic state (sinus tachycardia, hypertensive) Ongoing or recurrent pain or reinfarction Tachyarrhythmias such as AF Use a short-acting agent IV initially (metoprolol 5 mg at a time repeated at 5-minute intervals to a maximum dose of 15 mg) under continuous ECG and BP monitoring. Aim for a HR of 60 beats per minute (bpm) and SBP 100 110 mmHg. If hemodynamic stability continues 15 30 minutes after the last IV dose, start metoprolol 50 mg po bid. Esmolol is an ultra-short acting IV B-blocker, which may be tried if there is concern whether the patient will tolerate B-blockers.
CONTRAINDICATIONS TO THE USE OF B- BLOCKERS Absolute contraindications: heart rate (HR) <50, systolic blood pressure (SBP) <90 mmHg, moderate to severe heart failure, AV conduction defect, severe airways disease. Relative contraindications: asthma, current use of calcium channel blocker and/or B-blocker, severe peripheral vascular disease with critical limb ischemia, large inferior MI involving the right ventricle.
ACE inhibitors After receiving aspirin, B-blockade (if appropriate), and reperfusion, all patients with STEMI/LBBB infarction should receive an ACE inhibitor within the first 24 hours of presentation. Patients with high risk or large infarcts, particularly with an anterior STEMI, a previous MI, heart failure, and impaired LV function on imaging, will benefit most. The effect of ACE inhibitors appears to be a class effect; therefore, one may use the drug that the physician is familiar with.
Assessment of Reperfusion Options for STEMI Patients Step 1: Assess time and risk. Time since onset of symptoms Risk of STEMI Risk of fibrinolysis Time required for transport to a skilled PCI laboratory Step 2: Determine if fibrinolysis or invasive strategy is preferred. If presentation is <3 hr and there is no delay to an invasive strateg y, there is no preference for either strategy. Fibrinolysis is generally preferred if: Early presentation ( 3 hr from symptom onset and delay to invasive strategy) Invasive strategy is not an option Catheterization laboratory occupied or not available Vascular access difficulties Lack of access to a skilled PCI laboratory[*][ ] Delay to invasive strategy Prolonged transport (Door-to-Balloon) (Door-to-Needle) more than 1 hr[ ][ ] Medical contact-to-balloon or door-to-balloon more than 90 min
Reperfusion therapy (thrombolysis) Indications for thrombolysis Typical history of cardiac pain within previous 12 hours and ST elevation in two contiguous ECG leads (>1 mm in limb leads or >2 mm in V1 V6). Cardiac pain with newly presumed LBBB on ECG. If ECG is equivocal on arrival, repeat at 15- to 30-minute intervals to monitor progression. Thrombolysis should not be given if the ECG is normal or if there is isolated ST depression (true posterior infarct must be excluded). Timing of thrombolysis Greatest benefit is achieved with early thrombolysis (especially if given within 1 1/2 hours(90min.s) of onset of first pain. Patients presenting between 12 and 24 hours from onset of pain should undergo thrombolysis only with persisting symptoms and ST-segment elevation. Elderly patients (>65 years) presenting within the 12- to 24-hour time period with symptoms are best managed by primary PCI, as thrombolysis has been demonstrated to result in increased incidence of cardiac rupture.
Choice of thrombolytic agent This is partly determined by each center s local thrombolysis strategy. Allergic reactions and episodes of hypotension are greater with streptokinase (SK). Bolus agents are easier and quicker to administer, with a decrease in drug errors in comparison to first-generation infusions. Recombinant tissue-type plasminogen activator (rtPA) has a greater reperfusion capacity and a marginally higher 30-day survival benefit than that of SK, but this agent has been associated with an increased risk of hemorrhage. More recent rtPA derivatives have demonstrated a higher 90-minute TIMI-III (coronary reperfusion scale) flow rate, but have shown similar 30-day mortality benefits to those with rtPA. An rtPA derivative (rather than SK) should be considered for any patient with any of the following: Large anterior MI, especially if within 4 hours of onset Previous SK therapy or recent streptococcal infection (as this has been shown to be a risk factor for allergic reactions to SK) Hypotension (systolic BP <100 mmHg) Low risk of stroke (age <55 years, systolic BP <144 mmHg) Reinfarction during hospitalization where immediate PCI facilities are not available
Doses and administration of thrombolytic agents Streptokinase (SK) Give as 1.5 million units in 100 mL normal saline IV over 1 hour. There is no indication for routine heparinization after SK; there is no clear mortality benefit and there is a small increase in risk of hemorrhage. Recombinant tissue-type plasminogen activator (rtPA, alteplase) The GUSTO trial suggested that the front-loaded or accelerated rtPA is the most effective dosage regimen. Give 15 mg bolus IV then 0.75 mg/kg over 30 minutes (not to exceed 50 mg), then 0.5 mg/kg over 60 minutes (not to exceed 35 mg). This should be followed by IV heparin. Reteplase Give two IV bolus doses of 10 units 10 minutes apart. Tenectaplase Give as injection over 10 seconds at 30 50 mg according to body weight (500 600 g/kg). Maximum dose is 50 mg. APSAC (anistreplase) Give as an IV bolus of 30 mg over 2 5 minutes.
Complications of thrombolysis Bleeding is seen in up to 10% of patients. Most incidents are minor and at sites of vascular puncture. Local pressure is generally sufficient to stop this bleeding but occasionally transfusion may be required. In extreme cases, SK may be reversed by tranexamic acid (10 mg/kg slow IV infusion). Hypotension during the infusion is common with SK. Treatment consists of placing the patient in a supine position and slowing/stopping infusion until the blood pressure rises. Treatment with cautious (100 500 mL) fluid challenges may be required, especially in inferior/ RV infarction. Hypotension is not necessarily evidence of an allergic reaction and may not warrant treatment as such. Allergic reactions are common with SK and include a low-grade fever, rash, nausea, headaches, flushing, and, rarely (0.1%), anaphylaxis. Give hydrocortisone 100 mg IV with chlorpheniramine 10 mg IV. Intracranial hemorrhage is seen in ~0.3% of patients treated with SK and in ~0.6% with rtPA. Reperfusion arrhythmias (most commonly a short, self-limiting run of idioventricular rhythm) may occur. Systemic embolization may occur from lysis of thrombus within the left atrium, LV, or aortic aneurysm.
Contraindications to thrombolysis Absolute contraindications to thrombolysis Active internal bleeding Suspected aortic dissection Recent head trauma and/or intracranial neoplasm Previous hemorrhagic stroke at any time Previous ischemic stroke within the past 1 year Previous allergic reaction to fibrinolytic agents Trauma and/or surgery within past 2 weeks at risk of bleeding Relative contraindications to thrombolysis Trauma and/or surgery more than 2 weeks previously Severe uncontrolled hypertension (BP >180/110) Nonhemorrhagic stroke over 1 year ago Known bleeding diathesis or current use of anticoagulation within therapeutic range (INR 2) Prolonged (>10 minutes) cardiopulmonary resuscitation Prior exposure to SK (if planning to give SK, especially previous 6 9 months) Pregnancy or postpartum Lumbar puncture within previous 1 month Menstrual bleeding or lactation History of chronic severe hypertension Non compressible vascular punctures (e.g., subclavian central venous lines)
Reperfusion by primary PCI Primary PCI is the current gold-standard reperfusion strategy for treatment of STEMI. Indication for primary PCI All patients with chest pain and ST-segment elevation or new LBBB fulfill primary PCI criteria (compare with indications for thrombolysis). This includes a group of patients in whom ST-segment elevation may not fulfill all criteria for thrombolysis. In general, patients in whom thrombolysis is contraindicated should be managed by primary PCI.
Outcome in primary PCI A superior outcome in patients with STEMI who are treated with primary PCI in comparison to outcomes with thrombolysis. There is a significant short-term, as well as long-term, reduction in mortality and major adverse cardiac events (MACE) (death, nonfatal reinfarction, and nonfatal stroke) in STEMI patients treated with primary PCI, with better LV function, a higher vessel patency rate, and less recurrent myocardial ischemia. Interhospital transportation for primary PCI (community hospital to invasive center) is safe, and primary PCI remains superior to thrombolysis despite the time delays involved. It is generally accepted that in the acute phase only the culprit lesion(s) and vessel(s) will be treated. The pattern of disease in the remainder of the vessels will determine whether further revascularization should be performed as an inpatient or an elective case in the future. STEMI patients treated with uncomplicated primary PCI can often be discharged safely within 72 hours of admission without the need for further risk stratification. Primary PCI is more cost-effective in the long term than thrombolysis with significant savings from fewer days in the hospital, less need for readmission, and less heart failure. Post-discharge care, secondary prevention, and rehabilitation remain identical to that for other MI cases.
Rescue PCI Rescue PCI may be performed as an adjunct to thrombolysis but should be reserved for patients who remain symptomatic post-thrombolysis failure to reperfuse) or develop cardiogenic shock. We recommend that all patients who continue to have post-thrombolysis symptoms and/or ongoing ST-elevation with or without symptoms be discussed with the local invasive cardiac center for urgent catheterization and revascularization. Surgery for acute STEMI CABG in the context of an acute STEMI is of value in the following situations: High-risk coronary anatomy on catheterization (left main stenosis, left anterior descending [LAD] ostial disease). Complicated STEMI (acute mitral regurgitation, or ventricular rupture) STEMI patients (with or without successful thrombolysis) with additional coronary lesions whose anatomy is best served by CABG on prior or subsequent catheterization
STEMI: additional measures Low-molecular-weight and unfractionated heparin UFH There is no indication for routine IV heparin following SK. IV heparin (4000 U/max IV bolus followed by 1000 U/hr max adjustedf or an aPTT ratio of 1.5 2.0 times control) should be used routinelyfollowing rtPA and its derivatives for 24 48 hours. LMWH There is clinical trial data supporting the use of LMWH andthrombolysis (e.g., enoxaparin 30 mg IV bolus, then 1 mg/kg SC q12h). As an alternative to UFH, LMWH can be used at a prophylactic doseto prevent thromboembolic events in high-risk patients. Clopidogrel and other antiplatlets inhibitors This should be administered to all patients undergoing primary PCI(loading dose 300 600 mg po followed by 75 mg qd). The length of therapy is determined by the type of stent used. Drug eluting stents require longer term use of clopidogrel than bare-metalstents (current guidelines for ACS is 1 year of Plavix). Calcium antagonists These are best avoided, especially in the presence of LV impairment. Diltiazem and verapamil started after day 4 5 in post-MI patients withnormal LV function may have a small beneficial effect. Amlodipine is safe to use in patients with poor LV function post-MI. Nifedipine has been shown to increase mortality and should beavoided.