Strengthening Supports Through Complex Technical Assistance
Learn about complex technical assistance provided by KEPRO HCQU in September 2016 to improve health care quality. Discover strategies and insights to enhance support systems effectively.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Strengthening Supports Through Complex Technical Assistance Presented by: KEPRO SW PA Health Care Quality Unit (KEPRO HCQU) September 2016 RB/AT 1
Disclaimer Information or education provided by the HCQU is not intended to replace medical advice from the individual s personal care physician, existing facility policy, or federal, state, and local regulations/codes within the agency jurisdiction. The information provided is not all inclusive of the topic presented. 2
Objectives List the benefits of the Complex Technical Assistance (CTA) process Promote the concept of person-centered approaches with care teams as a standard in their work areas 3
Health Care Quality Units From PA Dept. of Human Services (PA DHS): Health Care Quality Units (HCQUs) serve as the entity responsible to county I/DD programs for the overall health status of individuals receiving services in the county programs. HCQUs work to support and improve the state I/DD community system by building capacity and competency to meet the physical and behavioral health care needs of people with developmental disabilities living in Pennsylvania. From PA DHS Office of Developmental Programs Consulting: The HCQUs work to support and improve the health information and knowledge for the intellectual disabilities community service system by building capacity and competency within the physical and behavioral health care systems as well as the stakeholders of the I/DD system. HCQUs are unique to Pennsylvania 4
HCQU Service Delivery Model Not a provider of direct care services Resource people for care teams Best practices Standards of care Information specific to people with intellectual and developmental disabilities 5
HCQU Staff Complement & Oversight Administrative team and field staff team Field staff consists of 7 nurses and 3 behavioral health staff; 4 nurses are certified developmental disabilities nurses Activities directed by administrative entities (counties) served They are known as the Management Oversight Committee (MOC) 6
HCQU Core Functions Training Instructor-led or online training, self-learning packets for caregivers, families, people with I/DD, and healthcare professionals Capacity Building Technical Assistance General Complex 7
Creation of the CTA Process Management Oversight Committee (MOC) identified the need to work with teams who support individuals with challenging behaviors Reasons Improve the individual s quality of life Provide caregivers with tools and best practices to support people with I/DD and those who have a dual diagnosis Cost containment 8
Skills Required of Staff Facilitation skills Verbal and written communication skills Emotional self regulation Empathy 9
CTA Process Referral of Case and Assignment of Team Completed referral form received County Gatekeeper approves CTA Approved CTA is provided to HCQU HCQU team is then assigned 10
CTA Process: Before the First Meeting Supports Coordinator assembles care team Identifies key team members and coordinates meetings Record review by HCQU nurse 11
CTA Process: Meetings and Documentation of Suggestions The team meets Team develops goal for CTA HCQU offers suggestions Determine next meeting date Summary and suggestion letter to the team 12
CTA Process: Closing a CTA The team agrees that the CTA will close Required paperwork completed Communication to the gatekeeper about the CTA 13
Evaluation of a CTA: Team Members Nurse sends CTA evaluation form within 25-40 calendar days after the close of the CTA If no response, the request is made again in 10 days 14
Evaluation of a CTA: Administrative Entity (AE) AE Evaluation form sent to county at 6-9 months Provides feedback several months after the close of the CTA 15
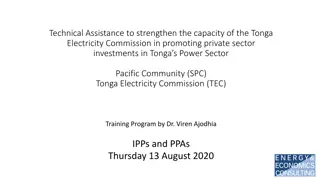
Current Data Related to CTA Effectiveness Number of Complex TAs Active within Fiscal Year and Number with BH/Restraint Component 120 100 80 60 40 20 0 FY2011-12 FY2012-13 FY2013-14 FY2014-15 FY2015-16 Overall Satisfaction with Complex Technical Assistance 100.0 95.0 % Overall Satisfaction 90.0 85.0 80.0 75.0 FY2011-12 FY2012-13 FY2013-14 FY2014-15 FY2015-16 17
Case Studies 18
AL-108 Case Study 23-year-old female Diagnoses: autism, bipolar disorder, seizure disorder, seasonal allergies, constipation, may have Cornelia de Lange syndrome, severe ID Opened 11/14/13; Closed 8/13/14 Open for 9 months 19
AL-108: Reason for Referral Injuries to staff Night time behaviors and rituals Sensory concerns 20
AL-108: Desired Outcomes Assist individual with night routine Decrease number of injuries to caregivers Address sensory issues CTA Goal: Assist team with supporting individual in exploring methods for communication 21
AL-108: Pertinent Information Scratching and biting staff on a daily basis Urinating in bedroom Stripping off clothing Sleeping on the floor Known to have sensory issues 22
AL-108: Pertinent Information, (continued) May have Cornelia de Lange Syndrome Pre-occupied with self stimulation Inability to verbally communicate needs Sensory- likes to snuggle tightly, sit on hard surfaces Has 1:1 staffing 23
AL-108: Areas Addressed Through the CTA Process Medical Sensory Communication Night time routine Unidentified syndrome 24
AL-108: Status at Close of CTA Communicating more often using her own signs Increased participation in social activities/less self isolation Appears to be much happier Staff no longer needed to wear arm guards for hygiene and assisting with activities of daily living 25
AL-108: Evaluations: Residential HCQU Team brought education and knowledge Increased communication between client and care team Team s injuries went from daily occurrence to almost none to report Helped care team be more confident and safe 26
AL-108: Contributing Factors to Success Dedicated care team Team across all environments participated in CTA Changes were made in all environments 27
AL-114 Case Study 27-year-old male Diagnoses- glaucoma, psychiatric disorder, NOS, mood disorder, ICD, IED, anxiety disorder, mild ID Opened 5/13/14; Closed 10/30/14 Open for 5 months 28
AL-114: Reason for Referral Property destruction Physical harm to staff Multiple personalities Two involuntary psychiatric hospitalizations in three weeks and another hospitalization two months later Unlawful restraint 29
AL-114: Desired outcomes Decrease hospitalizations Decrease law enforcement involvement Support, information and training for staff CTA Goal: Reduce incidences of hospitalization and police involvement 30
AL-114: Pertinent Information History of severe and prolonged trauma at a very early age Identifies as a woman Hearing and vision impairment Has three distinct personalities/voices that he uses Staff and housemates afraid of him. Staff states they are walking on eggshells around him 31
AL-114: Pertinent Information, (Continued) Frequent episodes of involuntary hospitalizations after throwing dishes and furniture at others in his home Stated he has no family and staff do not care about him Had another psych hospitalization while CTA was open; after that he was on 1:1 staffing 32
AL-114: Areas Addressed Through the CTA Process Medical Safety Sensory Communication Trauma 33
AL-114: Status at Close of CTA Doing very well with no hospitalizations or police involvement in three months Staff reports that they and the individual feel more confident, safe, and less anxious Note: This team chose to implement every suggestion offered by the HCQU team 34
AL-114: Evaluations: Residential Team met the goal Staff more responsive to the individual Rates of aggression have decreased greatly 35
AL-114: Evaluations: AE CTA effective in providing the care team tools needed to support him Staff knows how to consistently redirect him to de- escalate to prevent hospitalization No hospitalizations and only one law enforcement involvement since the close of the CTA 36
AL-114: Contributing Factors to Success Dedicated team who implemented all suggestions from the CTA Management team that valued staff; complimented and supported them Consistency in communication techniques, using a respectful approach Team s understanding of the effects of trauma and how to work with someone who has experienced trauma 37
WE-29 Case Study 27-year-old male Diagnoses: autism, anxiety disorder, seasonal allergies, bipolar disorder, hypertension, bowel irregularity, Lennox-Gastaut syndrome, moderate ID Closed within two months of opening, since there was no care team to work with 38
WE-29: Creation of CTA Other Category HCQU involvement is requested by the state or the county on cases that are particularly challenging HCQU is a participating member of the team, rather than the facilitator of the process Meetings attended by HCQU management staff 39
WE-29: Pertinent Information Physical assault on staff and peers Property destruction Breaking windows and throwing things out Ripping commodes out of the floor Breaking all the way through drywall Breaking the TV in 1/2 Self injurious behaviors/yelling profanities/stripping clothes Elopement Prolonged hospitalizations 40
WE-29: Strategy of Transition Team Open new home specifically to support this person Environmental changes to protect individual and staff Train staff immediately Support agency as they support him 41
WE-29: HCQU Does Not Collect Data From CTA Other Cases We note that our staff participated in this process, but do not ask for evaluations of the process or the outcomes We learn of the outcomes via our participation on the AE Risk Management Team 42
WE-29: Status Today No hospitalizations in four years No longer trying to elope 43
WE-29: Contributing Factors to Success Interdisciplinary approach where decision makers sat at the table and influenced outcomes Consistent staff who truly understand how to work with this individual Residential management strongly supports care team and debriefs them if there is an incident; offers extra days off or other compensation Care team feels extremely valued Case was presented statewide as a model of care 44
Limitations to Effectiveness of the Process Agency staff turnover Suggestions not implemented Individual experiences new life event/medication side effects HCQU does not continue to follow the individual or the team 45
Data Related to CTAs Westmoreland County Developmental Services HCQU CTA/Dual Diagnosis/Risk Management Data 2013 CTA s were done for 15 people identified as at risk: 6 physical health, 8 behavioral, 1 Abuse/neglect. 4 of the 6 physical health were resolved*. 5 of the 8 behavioral were resolved. The abuse/neglect was resolved. * By resolved I am meaning that the person has not appeared on Risk Management again for the same reason/issue and/or the DD/Psych review. For 2015 especially this will not be accurate since we need to reassess at the close of this calendar year. 2014 16 CTA s were done: 8 physical health and 8 behavioral. 7 of the 8 physical health were resolved and 7 of the 8 behavioral were resolved. According to this data CTA s have had an 86% success rate in the physical health cases and a 71% success rate in the behavioral cases. 2015 14 CTA s were done. 7 physical health 5 behavioral, 1 restraint and 1 I to I abuse. 6 of the 7 physical were resolved. 4 of the 5 behavioral were resolved, 1 restraint was resolved and the I to I Abuse is resolved. 46
Improved Quality of Life He now talks with the therapist about how he feels. He never would talk to anyone about his experience before. He is engaged in new activities that he enjoys such as his garden and walking the neighbor s dog. 47
References Kepro HCQU Job Aid for CTAs Kepro HCQU database for CTAs Westmoreland County Risk Management Committee Goreczny, A.J., Hobbs, E.R., Peterson, L.M. et al. Improving Quality of Care for Individuals with Intellectual and Developmental Disabilities via Consultation: Process Improvement and Support of Interprofessional Teams Rev J Autism Dev Disord (2015) 2: 19. doi:10.1007/s40489-014- 0031-8 48
References Office of Developmental Programs Consulting System. (2016). HCQU. Retrieved on July 29, 2016 from http://www.odpconsulting.net/hcqu/#.V9Fjok0rLIU PA Department of Human Services, (2016). Healthcare Quality Units. Retrieved on July 29, 2016 from http://www.dhs.pa.gov/provider/intellectualdisabilit ies/healthcarequalityunits/ 49
References Philadelphia Mental Health Care Corporation. Philadelphia Coordinated Healthcare. (2010).Accessed on 9/7/16 from https://www.pmhcc.org/index.php/programs/philadelphia- coordinated-health-care Morrow, J. Emerging Priorities in Health Promotion Programs. Chapter 7: Health Promotion in People with Disabilities. (n.d.). Accessed on 9/7/16 from http://samples.jbpub.com/9780763753771/53771_CH07_FINAL.p df National Institute of Health. 8/17/2006. Appendix A: Surgeon General s Conference on Health Disparities and Mental Retardation, December 5, 2001. Jill Morrow, MD: Creative Program Presentation discussing HCQUs. Retrieved on 9/7/16 from https://www.nichd.nih.gov/publications/pubs/closingthegap/Pages /sub12.aspx 50