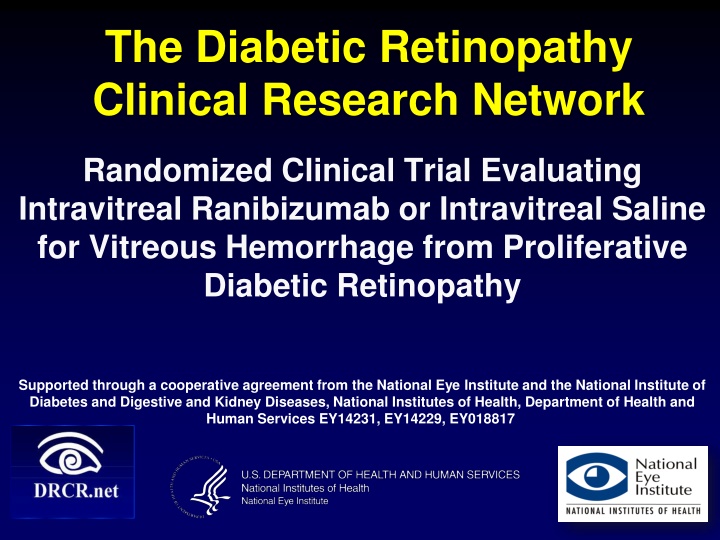
Study on Intravitreal Ranibizumab for Diabetic Retinopathy
This clinical trial conducted by The Diabetic Retinopathy Clinical Research Network evaluated the effectiveness of intravitreal ranibizumab injections compared to saline injections for vitreous hemorrhage in proliferative diabetic retinopathy cases. The study aimed to assess the impact on the need for vitrectomy and safety of the anti-VEGF therapy. A total of 261 eyes were randomized, with follow-up injections performed based on predetermined criteria. Baseline characteristics and outcomes were analyzed to determine the optimal treatment approach for this condition.
Uploaded on | 0 Views
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
The Diabetic Retinopathy Clinical Research Network Randomized Clinical Trial Evaluating Intravitreal Ranibizumab or Intravitreal Saline for Vitreous Hemorrhage from Proliferative Diabetic Retinopathy Supported through a cooperative agreement from the National Eye Institute and the National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health, Department of Health and Human Services EY14231, EY14229, EY018817 1
Study Objectives To determine if intravitreal injections of ranibizumab decrease the proportion of eyes in which vitrectomy is performed compared with saline injections in eyes presenting with vitreous hemorrhage from PDR. Note: This trial was not a comparison of anti-VEGF with observation or sham injection; rather the trial was a comparison of intravitreal anti-VEGF with intravitreal saline injection To assess the efficacy and safety of anti-VEGF therapy as treatment for vitreous hemorrhage due to PDR. 2
Study Enrollment 261 Eyes Randomized (61 Sites) Intravitreal Injection of 0.5 ranibizumab N = 125 Intravitreal Injection 0.9% sodium chloride N = 136 12 Week Visit Completion 95% Overall* (96% Ranibizumab Injection; 95% Saline Injection) * One death occurred prior to the 12 week visit. 4
Follow-Up Treatment Follow-up injections performed at 4 and 8 weeks unless: Vitreous hemorrhage had cleared enough to complete PRP or Vitrectomy had been performed. All eyes were to be treated with complete PRP as soon as possible. The decision to perform vitrectomy was based on study guidelines. 6
Baseline Study Eye Characteristics Ranibizumab N=125 50% 42% 8% Saline N=136 57% 42% 13% Prior PRP Prior Treatment for DME Prior treatment with anti- VEGF for DME E-ETDRS Visual Acuity Median (25th, 75th Percentile); Snellen Equivalent OCT Signal Strength = 0 > 0 34 (0,61) 20/200 28 (0, 59) 20/320 59% 40% 71% 28% 10
Baseline Study Eye Characteristics Ranibizumab N=125 Saline N=136 Duration of Vitreous Hemorrhage <1 Month 1-3 Months 4-6 Months >6 Months IOP - mmHg Median (25th, 75th percentile) 53% 33% 6% 9% 55% 29% 8% 8% 15 (12, 17) 14 (12,17) 11
Total Number of Intravitreal Injections In Eyes without vitrectomy or complete PRP prior to 8 weeks Number of Injections Ranibizumab Injection N = 86 0 1 4 81 0 Saline Injection N = 98 0 5 10 82 1 0 1 2 3 4 One subject was given masked intravitreal study drug at the 12-week follow-up visit when a study injection was not scheduled per protocol. Since an injection was not scheduled, a drug number according to the randomized treatment was not obtained, and it is possible that the wrong randomized treatment was performed. The investigator did believe that an injection was medically indicated for the study participant. 12
Non-Protocol Study Eye Treatment for DME Prior to 16 weeks Ranibizumab Injection N = 4 4 Saline Injection N = 4 4 Number of Eyes with Non-Protocol Study Eye Treatment for DME Intravitreal Bevacizumab (Avastin) Intravitreal Triamcinolone Acetonide Focal/Grid Laser Photocoagulation 1* 2* 2 1** 0 3 Note: only focal/grid laser was permitted per protocol prior to 16 weeks *One eye received both bevacizumab and triamcinolone for DME after vitreous hemorrhage cleared and PRP was considered complete **DME treatment performed 1 week post-vitrectomy 13
Vitrectomy Primary Outcome 14
Cumulative Probability of Vitrectomy by 16 Weeks
Complete Panretinal Photocoagulation Secondary Outcome 16
Cumulative Probability of Complete PRP (in absence of vitrectomy) by 16 Weeks
Visual Acuity at Follow-up Visits Secondary Outcome 18
Mean Change in Visual Acuity from Baseline 25 Mean Change in Letter Score P=0.04 Ranibizumab Placebo 20 15 10 5 0 Baseline 4-weeks 8-weeks 12-weeks Treatment comparison for the mean change in visual acuity at the 12 week visit was performed using a longitudinal mixed model adjusting for baseline visual acuity. 19
Ocular Adverse Events of Interest Prior to 16 weeks Ranibizumab Injection N=125 0 1 ( <1%) Saline Injection N=136 1 (< 1%) 4 (3%) Ocular Events Endophthalmitis Angle or iris neovascularization Neovascular glaucoma Cataract Surgery Recurrent vitreous hemorrhage 1 (<1%) 1 (<1%) 8 (6%) 1 (<1%) 2 (1%) 23 (17%) Treatment comparison for recurrent vitreous hemorrhage was performed using Fisher Exact test (P-value = 0.01) 21
Retinal Detachments Prior to 16 weeks Ranibizumab Injection N=125 8 (6%) Saline Injection N=136 9 (7%) Traction retinal detachment only Rhegmatogenous retinal detachment only Combined retinal detachment Any Retinal Detachment 1(<1%) 2(2%) 1(<1%) 0 10 (8%) 11(8%) 22
Elevated Intraocular Pressure Prior to 16 weeks Ranibizumab Injection N=125 6% Saline Injection N=136 8% Increase of IOP 10 mm Hg from baseline IOP 30 mmHg Currently on IOP-lowering medication, but not at baseline Glaucoma surgery at anytime Elevated IOP/Glaucoma 3% 10% 3% 10% 0 0 13% 14% Percentages represent the number of eyes with at least 1 occurrence.
Systemic Adverse Events of Interest Prior to 16 weeks Ranibizumab Injection N = 125 Saline Injection N = 136 Hypertension-related event 3 7 Cardiovascular or cerebrovascular event 1 6
Discussion 25
Conclusions From Primary Outcome As a result of having substantially overestimated the control group rate when estimating sample size, the study may not have been sufficiently powered to detect a treatment group difference. This study suggests little likelihood of a clinically important difference between ranibizumab and saline on the rate of vitrectomy by 16 weeks in eyes with VH from PDR 26
Conclusions from Secondary Outcomes Short term secondary outcomes including visual acuity improvement, increased PRP completion rates, and reduced recurrent VH rates suggest biologic activity of ranibizumab Intravitreal ranibizumab does not appear to increase the risk of retinal detachment in the short term 27
Other Considerations Whether vitrectomy rates after saline or ranibizumab are different than observation alone cannot be determined from this study 28