Summary of Non-Alcoholic Fatty Liver Disease (NAFLD) Knowledge
Non-Alcoholic Fatty Liver Disease (NAFLD) is a common condition characterized by liver fat accumulation in individuals without alcohol abuse. Risk factors, disease progression, histology, screening, and non-invasive scoring methods are discussed. Visual aids illustrate the natural history, disease progression, liver histology, and screening process for NAFLD diagnosis.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Non Alcoholic Fatty Liver Disease NAFLD Summary of current knowledge January 2018 NAFLD
Natural History of Nonalcoholic Fatty Liver Disease (NAFLD) RISK FACTORS Overweight Obesity Metabolic syndrome Dyslipidemia Type 2 diabetes Polycystic ovary syndrome ? HCC ? > 1-2%/year 25% F3 F1 NASH F4 NAFLD F0 F2 25%, with progression of one stage fibrosis per decade Regression ? Decompensation Isolated liver steatosis Adapted from Diehl AM. NEJM 2017;377:2063-72 NAFLD
NAFLD: progression of disease Healthy Liver NAFLD NASH Cirrhosis Reversible Reversible Irreversible Large droplets of fat Collagen fibers Bloated hepatocyte Scarring Hepatocyte Nucleus Inflamed dying hepatocyte Remnant of dead cells Small droplets of fat Displaced nucleus
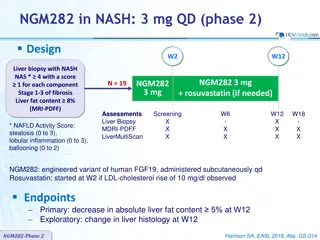
Liver histology in NAFLD NAFLD NASH Cirrhosis Hepatic steatosis 5% 5% Current or previous Lobular and portal inflammation Yes Yes Hepatocellular injury (ballooning) No Yes Yes Fibrosis No F0 to F3 F4 Histology scoring NAS (NAFLD Activity Score), reflects disease activity: unweighted composite of Steatosis (0 to 3) Lobular inflammation (0 to 3) Ballooning (0 to 2) SAF Score: semi-quantitative score of Steatosis (0 to 3) Activity (lobular inflammation + ballooning) = NAS (0 to 8) Fibrosis (0 to 4) Adapted from Chalasani N. Practice Guidance from the AASLD;Hepatology 2018;67:328-357 NAFLD
Screening for NAFLD Incidentally discovered Hepatic Steatosis (Imaging) Type 2 diabetes Liver-related symptoms or signs ? or Abnormal liver biochemistries ? YES NO Evaluation for potential NAFLD Alternate causes Significant alcoholism (> 21 standard drinks/week in men, > 14 in women) Medications Assess for metabolic risk factors Obesity Diabetes Dyslipidemia Exclude other etiologies for steatosis, chronic liver diseases NAFLD Fibrosis Score (NFS) FIB-4 index Elastography Adapted from Chalasani N. Practice Guidance from the AASLD; Hepatology 2018;67:328-357 NAFLD
Non-invasive Scores of NAFLD NAFLD Fibrosis Score (NFS) * FIB-4 ** Age + + AST + + ALT + + Platelet count + + BMI + Albumin + Impaired fasting glucose or diabetes + * NFS: www.mdcalc.com/nafld-non-alcoholic-fatty-liver-disease-fibrosis-score or gihep.com/calculators/hepatology/nafld-fibrosis-score ** FIB-4: www.mdcalc.com/fibrosis-4-fib-4-index-liver-fibrosis or gihep.com/calculators/hepatology/fibrosis-4-score NAFLD
Assessment of NAFLD Non invasive evaluation Presence of metabolic syndrome: predictive of steatosis LIVER BIOPSY NFS*, FIB-4, vibration controlled transient elastography, magnetic resonance elastography: predictive of advanced fibrosis LIVER BIOPSY Serum ferritin and iron saturation: if , marker of possible hepatic injury and/or hemochromatosis (homozygote or heterozygote C282Y HFE mutation) LIVER BIOPSY High serum titers of autoantibodies in association with other features suggestive of autoimmune liver disease (> 5 ULN aminotransferases, high globulins, or high total protein to albumin ratio) work-up for autoimmune liver disease Consider presence of commonly associated comorbidities (central obesity, hypertension, dyslipidemia, diabetes or insulin resistance, hypothyroidism, polycystic ovary syndrome, obstructive sleep apnea) * NFS is based on 6 variables (age, BMI, hyperglycemia, platelet count, albumin, and AST/ALT ratio) and is calculated using the published formula http://gihep.com/calculators/hepatology/nafld-fibrosis-score/ Adapted from Chalasani N. Practice Guidance from the AASLD ; Hepatology 2018;67:328-357 NAFLD
Likelihood of NASH and fibrosis in patients with NAFLD Low Intermediate High Age < 40 > 40 > 50 Type 2 diabetes No Yes, well-controlled Yes Obesity No Yes Yes Hypertension Yes Yes Fibroscan kPa < 7 > 7 > 8.5 AST < 20 > 20 > 40 and AST/ALT ratio 1 NFS (NAFLD Fibrosis Score) < - 1.455 - > 0.676 FIB-4 < 1.3 - > 2.67 Patients at risk for clinical progression Steatosis 1 Ballooning 1 Inflammation 1 NAS (NAFLD Activity Score) 4 F2 Adapted from Konerman MA. J Hepatol 2018 (Epub ahead of print) NAFLD
Comorbidities of NAFLD Liver complications Cirrhosis End-stage liver disease CV diseases Liver (HCC)* NAFLD GI malignancies Colon (men)** Esophagus Stomach Pancreas Cancer Metabolic comorbidities More frequent More severe Non-GI malignancies Kidney (men) Breast (women)** HR of * 17 ; ** 2 ; *** 1.9 Adapted from Kim GE. J Hepatol 2018;68:140-6 ; Chalasani N. Practice Guidance from the AASLD; Hepatology 2018;67:328-357 NAFLD
Management of patients with NASH and fibrosis Interventions recommended Objective/restrictions Benefit 3-5% 7-10% > 10% Improve steatosis Improve NASH, including fibrosis NASH resolution and fibrosis Weight loss (Hypocaloric Diet [ by 500-1,000 kcal/day]) Moderate-intensity exercise (30 min/day x 3-5 times/week) If isolated Prevent or reduce steatosis Limit alcohol consumption ( 2 drinks/day men, 1 drink women) All patients Inflammation and fibrosis Coffee consumption ( 2 cups/day) Modification of CVD risk factors All patients CV morbidity and mortality Statins Interventions to consider If dyslipidemia In patients with or without type 2 diabetes Pioglitazone Improves liver histology Vitamin E (rrr -tocopherol) In non-diabetic patients Improves liver histology Foregut bariatric surgery In otherwise eligible obese Omega-3 fatty acids If hypertriglyceridemia Improve hypertriglyceridemia Not recommended : Metformin, GLP-1 agonists (liraglutide), Systematic bariatric surgery, Ursodeoxycholid acid Adapted from Chalasani N. Practice Guidance from the AASLD ; Hepatology 2018;67:328-357 ; Diehl AM. NEJM 2017;377:2063-72 NAFLD
Endpoints in clinical trials of NAFLD and NASH Outcomes Hard endpoints Surrogate endpoints All cause mortality Liver-related mortality Child-Pugh and MELD scores Hepatic venous portal gradient Clinical Hepatic decompensation Fibroscan (kPa) and magnetic resonance elastography Biomarkers (pro-C3, FIB-4, NFS, enhanced liver fibrosis) Progression to cirrhosis MRI-derived proton density fraction, Multiparametric MRI, Controlled attenuation parameter in hepatic fat content in insulin resistance HbA1c, fasting glucose, HOMA-IR Metabolic Impact on lipids in weight/BMI in necro-inflammation Multiparametric MRI, Liver enzymes Inflammatory in hepatocyte ballooning Fibroscan (kPa) and magnetic resonance elastography Biomarkers (pro-C3, FIB-4, NFS, enhanced liver fibrosis) in fibrosis stage Fibrosis Adapted from Konerman MA. J Hepatol 2018 (Epub ahead of print) NAFLD
NASH-new serum non-invasive biomarkers Not yet fully validated Could diagnose NASH and its severity Could identify patients likely to respond to therapy Chitinase-3-like protein 1(CHI3L1) YKL-40 Enhanced Liver Fibrosis (ELF) Test Comprised of TIMP-1 (tissue inhibitor of matrix metalloproteinase-1), PIII-NP (mino-terminal peptide of type III procollagen), and hyaluronic acid Pro C3 Derived from synthesis of type III collagen FIB-C3 Score HepQuant STAT Quantitative liver function test 60 min after oral administration of 4 mg tetra-deuterated cholic acid Non-invasive score-4 (NIS4) Detect patients with NAS 4 and F 2 Comprised of Chitinase-3-like protein 1(CHI3L1), alpha2-macroglobulin, microRNA 34a (MIR34a), and HbA1C Adapted from Harrison SA. AASLD 2017 NAFLD
Current Status of Pharmacologic Treatments for NASH No approved therapies for NASH Currently available therapeutics with (some) proven efficacy Vitamin E Pioglitazone NAFLD
NASH: targets for therapeutics Insulin resistance Cell stress apoptosis Fibrogenic remodeling Inflammation Insulin resistance modifiers Anti-inflammatory agents Cell stress modifiers Anti-fibrotic agents CCR2-CCR5 antagonist ASK-1 inhibitor PPAR- agonsit FXR agonist Dual PPAR-/ agonist Lysyl oxidase-like 2 inhibitor Galectin 3 FGF-21 FGF-19-like agent CCR2-CCR5 antagonist Vitamin E ASK-1 inhibitor PPAR- agonsit FXR agonist Dual PPAR-/ agonist Galectin 3 FGF-21 FGF-19-like agent PPAR Vitamin E ASK-1 inhibitor (selonsertib) PPAR- agonsit FXR agonist Dual PPAR-/ agonist FGF-21 FGF-19-like agent FXR agonist (obeticholic acid, GS-9674) GLP-1 FABAC FGF-21 (BMS-986036) Thyroxine analog Exemples of drugs in development Endpoints for clinical trials 1. Disease Activity (steatohepatitis) = NAFLD Activity Score (NAS) 2. Disease Progression = Fibrosis Stage 3. Clinical outocmes: Cirrhosis (MELD, Portal hypertension), Liver-related outcome, death Adapted from Konerman MA. J Hepatol 2018 (Epub ahead of print) ; Diehl AM. NEJM 2017;377:2063-72 NAFLD
NASH Pharmacological agents in development Drug Class Mechanism of action Objective liver fat and NAFLD activity score without of fibrosis Synthetic fatty acid/bile acid conjugate Impacts lipogenesis by upregulates the ABCA1 reverse cholesterol transporter and functions Aramchol Blockage of apoptotic and inflammatory caspase activation involved in hepatocyte cell death fibrosis and portal hypertension Phase 2b Pan-caspase inhibitor Emricasan fibrosis and portal hypertension Galectin-3 protein inhibitor GR-MD-02 Anti-fibrogenesis Agonist of the farnesoid X receptor : downregulates hepatic glucose and lipid metabolism. May also portal pressure and have anti- inflammatory and antifibrotic activity Semi-synthetic derivative of acid chenodeoxycholic acid fibrosis without NASH ; NASH resolution without of fibrosis Obeticholic acid NASH resolution without of fibrosis ; Clinical outcomes Regulation of metabolic homeostasis, inflammation, cellular growth, and differentiation Dual PPAR- / agonist Elafibranor Phase 3 NAFLD activity score without of fibrosis ; fibrosis without NASH dual CCR2/CCR5 antagonist Reduction of hepatic inflammation and fibrosis Cenicriviroc Apoptosis signal regulating kinase 1 (ASK1) inhibitor Selonsertib (GS-4997) Reduction in oxidative stress-related cell death, fibrosis and inflammation fibrosis without NASH Adapted from Konerman MA. J Hepatol 2018 (Epub ahead of print) NAFLD
Improvement of NASH with pharmacologic agents Results of trials for individual treatment agents * Placebo Elafibranor Vitamin E Cenicriviroc Pioglitazone Selonsertib Obeticholic acid Simtuzumab % 100 Improvement in hepatic steatosis Resolution of NASH Improvement in fibrosis 80 p < 0.001 p = 0.001 69 p = 0.005 p = 0.001 61 60 54 p = 0.24 p = 0.12 p = 0.05 47 p = ns p = 0.004 44 p = 0.01 p = 0.10 41 38 40 36 37 35 p = 0.08 35 31 31 31 31 p = 0.02 29 22 21 21 20 20 19 18 20 13 10 5 80 72 70 72 102 98 31 39 80 72 70 72 102 98 31 39 80 72 70 72 102 98 145 144 57 10 0 * Enrollment criteria and durations of therapy differed between studies, and the primary endpoint definitions were not identical Adapted from Konerman MA. J Hepatol 2018 (Epub ahead of print) NAFLD
NASH Combination of metabolic damages to the liver Prevention and Lifestyle Modifications are key ! NAFLD