The 20- -Minute Medicare Visit
Physicians struggle to provide high-quality care for older patients in busy primary care practices. The presentation discusses the barriers, such as insufficient time and cognitive capacity, and offers practical changes for immediate implementation and long-term practice redesign. Insights from the ACOVE project highlight the need for better geriatric care standards to address the vulnerable elderly population.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
The 20 The 20- -Minute Medicare Visit Minute Medicare Visit David B. Reuben, MD Archstone Foundation Chair and Professor David Geffen School of Medicine at UCLA
DISCLOSURES DISCLOSURES None of the faculty, planners, speakers, providers nor CME committee has any relevant financial relationships with commercial interest There is no commercial support for this CME activity
Overview of Talk Overview of Talk What s the problem here? Fixing the problem Changes you can make on Monday Longer term practice redesign changes An example of practice redesign Does practice redesign work? Learning more
The Problem The Problem Physicians are unable to provide high quality of care for conditions affecting older persons within the context of busy primary care practices.
Health care quality for vulnerable Health care quality for vulnerable elderly elderly Assessing Care of the Vulnerable Elderly (ACOVE) project identified elders at increased risk for death or functional decline, created quality indicators based on literature review and expert panel for 22 conditions
ACOVE results ACOVE results Overall, 55% of Quality Indicators passed Compliance for geriatric conditions was worse than for general medical conditions (31% versus 52%) Care for specific conditions varies greatly Stroke 82%; end-of-life care 9% Wenger NS et al. Ann Int Med 2003
Barriers to good health care Barriers to good health care Insufficient cognitive capacity Not enough time The health care system isn t a system Rewards are wrong Competing agendas
Insufficient cognitive capacity Insufficient cognitive capacity Too much to know During 2001, the US National Library of Medicine added more than 12,000 new articles per week to its on-line archives To maintain current knowledge, a general internist would need to read 20 articles per day 365 days per year Shaneyfelt TM. JAMA 2001; 286:2000-2601
Too much to know Too much to know The rise in non-systematic reviews, case reports, trials, and systematic reviews, 1950 to 2007 Bastian H, Glasziou P, Chalmers I. Seventy-five trials and 11 systematic reviews a day: how will we ever keep up? PloS Med 2010; 7(9).
Insufficient cognitive capacity Insufficient cognitive capacity Too much to know Too much to remember Heart failure management 10 ACEIs 7 ARBs 3 Beta-blockers 2 aldosterone antagonists All with different starting and target doses
Not Enough Time Not Enough Time Assuming practice size 2500 patients age and chronic disease distribution of US population following guidelines for 10 chronic diseases Would take 10.6 hours per day! Plus time for management of other problems. Ostbye, Ann Fam Med 2005; 3:209-214.
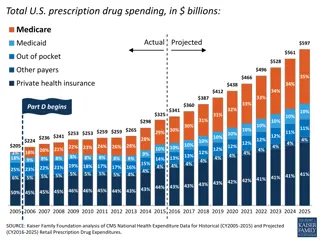
The Health Care System isnt The Health Care System isn t a System a System Duplication Reordering tests rather than looking for results 34% sometimes or often Unavailability of needed clinical info 72% sometimes or often Source: The Commonwealth Fund National Survey of Physicians and Quality of Care. 2005
The Wrong Reward System Productivity is most important factor in determining income Having more time to spend with patients is best method for improving quality Over half believe that providing higher quality of care often/sometimes means less income Source: The Commonwealth Fund National Survey of Physicians and Quality of Care. 2005
Competing Competing agendas agendas Patient Physician Addressing patient concerns Payer Alleviation of symptoms Live a long life Managing the Cost of care Technical quality of care Patient Satisfaction patient s care Managing diseases Administrative (documentation) Social issues Advice/Social interaction
Practice Redesign Practice Redesign Aims to improve quality and/or increase efficiency by: Fixing a problem or inefficiency in patient care Using different people or people differently Exploiting technology
Fixing an inefficiency Fixing an inefficiency Delegate data collection
Out-of-Office Preparation Office Visit Physician-Patient Encounter $$$$ $$ $ 1. Reduce time but increase effectiveness/efficiency of the inner circle 2. Always push to outermost possible circle whenever possible
Delegation to Patients Delegation to Patients Pre-visit questionnaires Initial Follow-up
Pre Pre- -visit Questionnaire visit Questionnaire 1. Past medical history - Current medications - Drug allergies - Surgical & medical hospitalization - Social history (habits, sociodemographics) - Preventive services, including lifestyle 2. Home safety checklist 3. Advance Directives
Pre Pre- -Visit Questionnaire Visit Questionnaire Specific questions on: Vision Hearing Dentition Falls Urinary incontinence Nutrition Depressive symptoms Functional status
Delegation to Patients Delegation to Patients Pre-visit questionnaire Initial Follow-up Lists Diaries
Delegation to Office Staff Delegation to Office Staff Screening/Case identification History gathering Following up on triggers Medications/allergies Enhanced vital signs/physical exam Orthostatic blood pressure readings Visual acuity testing Patient education
Run a More Efficient Practice Run a More Efficient Practice ) Delegate data collection ) Minimize data recording time Dictation Templates Computerized medical records increase documentation time http://www.cdc.gov/nchs/data/databrief s/db129.htm 2013
Strategies for Savings Time in Strategies for Savings Time in Clinical Practice Clinical Practice 3) Keep information needed for decision- making readily available Pocket guides PDA programs Useful books Computer retrieval system 4) Delegate plan execution Network of health professionals Health educators
Structuring Visits and Work Flow Structuring Visits and Work Flow ACOVE -2 Practice Redesign Case finding Delegation of data collection Structured visit notes to guide appropriate care processes Physician and patient education Linkage to community resources -Reuben et al. J Am Geriatr Soc. 2003;51:1787-93.
ACOVE ACOVE- -2 2 practice redesign practice redesign Case finding Delegation of data collection Structured visit notes to guide appropriate care processes Physician and patient education Linkage to community resources -Reuben et al. J Am Geriatr Soc. 2003;51:1787-93.
Case Finding Case Finding Brief questions to identify bothersome incontinence, memory loss, and falls or fear of falling Responses are given to provider at clinic appointment along
Structured Visit Note Structured Visit Note History items and simple procedures (completed by office staff) More detailed H & P, ordering tests (completed by physician) Impression and plan (completed by physician)
VISIT FORM: FALLS/MOBILITY PROBLEMS Reason for Visit: History of Present Illness: 1. If patient fell, date of last fall: __________________ 2. Circumstances of fall: Loss of consciousness . Tripped/stumbled over something .. Lightheadedness/palpitations . Unable to get up within 5 minutes .. Needed assistance to get up .. 3. Psychotropic medications (specify): Neuroleptics: ____________________ Benzodiazepines: ________________ Antidepressants: _________________ 4. 2 or more drinks alcohol each day .. Examination: 1. Lying: BP: _____/_____ Pulse: _____ Standing: BP: _____/_____ Pulse: _____ 3. Cognition: 3-Item recall: Fall since last visit (or in last year, if new patient) Fear of falling, balance/trouble walking 5. Uses device for mobility: Cane .. Walker .... Wheelchair Other, specify: ____________________ 6. Other conditions (e.g., Parkinson s, CVA, cardiac, neuropathy, severe OA), specify: ________________________________ 7. Vision: Noticed recent vision change . Eye exam in past year . NO YES NO YES 2. If NO eye exam in past year, Visual Acuity: OS: 20/_____ FAIL If FAIL Cognitive status: OD: 20/_____ OU: 20/_____ PASS 4. Gait: Abnormal if: -Hesitant start NORMAL ABNORMAL -Heels do not clear toes of other foot -Heels do not clear floor -Path deviates NO If indicated: Can pick up penny off floor .. Resistance to nudge . -Broad-based gait -Extended arms 5. Balance: Side-by-side, stable 10 sec . Semi-tandem,stable 10 sec .. Full tandem,stable 10 sec .. YES NO YES 6. Neuromuscular: Quad strength: Can rise from chair w/o using arms If indicated, hip ROM and knee exam: YES NO Rigidity (e.g., cogwheeling). Bradykinesia .. Tremor NO YES Impression: Diagnosis/Treatment Plan: Lab/Tests: EKG Holter monitoring Other: _________________ Strength problem Balance problem Parkinsonism Severe hip/knee OA Other: ______________ Treatment: Patient education handout: Falls Home safety checklist Strength/balance exercises: Referral for PT Assistive device: __________________________________ Referral for home safety inspection/modifications Change in medication(s): ___________________________ Referral for eye exam Cardiology consult Neurology consult Upper body Lower body Community resources Community exercise program Other: _________________________________________ Provider s Signature_________________________________________ Date of Visit______________ Patient Name: ____________________________ Med. Rec. # ______________________________ (Medical Group logo here) Date of Birth: _____________________________ PCP: ____________________________________
Patient educational materials Patient educational materials Assembled for each condition Readily available to the clinician to facilitate treatment Community resources Follow-up visit sheet
Decision Support Decision Support- -Physician Education Education Physician Small group educational sessions aimed at practical approaches Written briefs that describe management of the condition
Flexibility Flexibility Must address all conditions using all components of the intervention Flexibility in administration and content Decide how much of the intervention is performed by staff rather than physicians Can modify content and supporting materials
Practice Practice redesign redesign i interventions based on the ACOVE based on the ACOVE- -2 Model nterventions 2 Model Study Conditions Falls, UI, Dem Groups Delegation 2 PCP Minimal ACOVE-2 ACOVEprime Falls, UI 5 PCP Minimal- Moderate Moderate High Alz Assoc JAHF NP Dem Falls, UI, Dem, Dep, HF 2 PCP 1 Ger UniHealth NP Falls, UI, Dem, Dep 2 PCP High
Effects on Effects on quality in ACOVE in ACOVE- -2 2 intervention quality of of care care by intervention by condition condition Usual Care Usual Care ACOVE ACOVE- -2 2 Overall 22-32% 37-71% Falls 23-40% 44-79% Incontinence 17-37% 37-64% Dementia 38-44% 43-60% Depression 28-61% 51-63% In each, significant differences between UC and ACOVE for overall, falls and UI; variable significance for depression and dementia
Using people differently: Using people differently: Co Co- -management management Two or more health care providers jointly managing the patient s medical care to achieve the best quality and outcomes Many models, most focus on specific conditions (e.g., cancer, dementia) or on multiple conditions and coordination of care (e.g., Guided Care)
Co Co- -management: Who management: Who Physician specialist-physician generalist (e.g., oncologist-general internist) Other health profession-physician generalist (e.g., depression clinical specialist-primary care physician)
Co Co- -management: Process of Care management: Process of Care Assessment Developing care plan Recommendations Orders Monitoring Revising care plan
The UCLA Alzheimers and The UCLA Alzheimer s and Dementia Care Program Dementia Care Program Uses a co-management model with Nurse Practitioner Dementia Care Manager (DCM) Works with physicians to care for patients by Conducting in-person needs assessments Developing and implementing individualized dementia care plans Monitoring response and revising as needed Providing access 24 hours/day, 365 days a year
Co Co- -management: Quality of Care management: Quality of Care Evidence base: general Decreases in HbA1c, systolic and diastolic BP, total and LDL cholesterol (Shaw RJ, 2014) Evidence base: falls and dementia Condition Study Physician alone Co-management with nurse practitioner 44% P- value .002 Falls Ganz, 2010 17% Falls Reuben, 2013 32% 78% <.001 Dementia Reuben 2013 38% 59% <.001 Dementia Jennings, 2016 92%
UniHealth Quality of Care: Falls MD alone 45%* 7%* 34%* 12-22%* 8%* 79%* MD+NP 89%* 79%* 84%* 85%* 82%* 98%* Falls history performed Orthostatic BP checked Visual testing or eye exam Gait/balance/strength exam Home hazard evaluation Exercise/PT *p<0.01 for comparison between MD alone v MD+NP
UniHealth UniHealth Quality of Care: UI Quality of Care: UI MD alone 11%* 31%* 40%* 23%* 3%* 0* MD+NP 70%* 80%* 93%* 75%* 34%* 95%* Incontinence history Incontinence exam Classification of type of UI Discuss treatment options Assess response to treatment Behavioral/lifestyle Rx first *p<0.01 for comparison between MD alone v MD+NP
Overall Dementia Quality of Care Overall Dementia Quality of Care (ACOVE (ACOVE- -3 and PCPI QIs)* 3 and PCPI QIs)* Community-based physicians Community-based physicians & NP UCLA Alzheimer s and Dementia Care 92% 38% 60% * Based on medical record abstraction
UCLA Alzheimers and Dementia UCLA Alzheimer s and Dementia Care Program: Quality Care Program: Quality Check meds as cause Laboratory testing Depression screen Caregiver support Behav & psych sx screen Driving intervention ID surrogate decision-maker 99% 82% 99% 99% 100% 95% 94%
Co Co- -management: Challenges management: Challenges Defining scope of responsibility Range of clinical problems Co-manager versus primary care physician Order writing Acute clinical problems Communication With primary care physician With other health providers (e.g., specialists, therapists)
Exploiting Exploiting technology technology Remote access to medical records Passive and active (e.g., ADT notification) Smart notes and records Patient entry into medical records (e.g., Open notes, Tonic software) Mobile and remote technology
New Practice Redesign Efforts New Practice Redesign Efforts Improving communication Sight lines and co-location Huddles and team meetings Redefining roles of staff Enhanced rooming/prepping the chart Standing orders/prescription renewals Scribes and order entry Inbox management Health coaching and care coordination