The Evolution of type 2 Diabetes Prof. Abbas Orabi
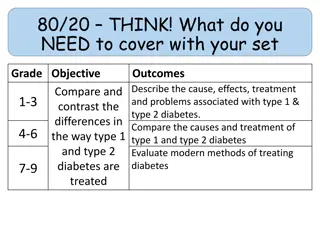
The evolution and pathophysiology of type 2 diabetes, discussing the genetic susceptibility and interacting gene sets contributing to insulin resistance, beta-cell failure, and diabetic complications. Insights into the genes associated with diabetes, insulin secretion, and insulin action. Natural history, diagnosis, and treatment of type 2 diabetes, along with the ominous octet concept outlining multiple defects in disease progression.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
The Evolution of type 2 Diabetes Prof. Abbas Orabi Prof. of Diabetes and Endocrinology Zagazig University
Developing diabetes needs: Genetic susceptibility Acquired (environmental factors)
Genetic susceptibility is determined by complexed heterogenic, polygenic gene sets.
Interacting gene sets for: Insulin resistance -cell failure Diabetic complications
Genes Genes Insulin resistance- lipotoxicity Environment b-cell dysfunction/ Failure; dec. mass Abn. First phase 1st & 2nd peripheral Environment hepatic IFG IGT Glucose Toxicity Glucose Toxicity Type 2 diabetes DM will NOT occur if B-cells not genetically predisposed Reaven GM. Physiol Rev. 1995;75:473-486 Reaven GM. Diabetes/Metabol Rev. 1993;9(Suppl 1):5S-12S; Polonsky KS. Exp Clin Endocrinol Diabetes. 1999;107 Suppl 4:S124-S127.
Genes that Cause or are Associated with Diabetes Insulin Secretion Neonatal KCNJ11/Kir6.2 ABCC8/Sur1 Insulin MODY HNF-1 ,1 , 4 Glucokinase PDX1/IPF1 Neurod1/Beta2 KLF11 CEL Mitochondrial diabetes Type 2 CDKAL1 TCF7L2 HHEX/IDE SLC30A8/ZNT8 WFS1 NOTCH2-ADAM30 Insulin action Insulin receptor PPARG PHENOTYPE- eg: age of presentation, IFG/ IGT/Both/ severity depends on number of which kind of genes a person inherits GENOTYPE Modified from McCarthy, NEJM 363:24,2339. Obesity FTO MCR4 Unknown IGFBP2 CDKN2A/B KIF11 JAZF1 CDC123-CAMK1D TSPAN8-LGR5 THADA ADAMTS9 NOTCH-ADAM30
Natural History Macrovascular complications Microvascular complications b-cell function Insulin resistance Blood glucose Treatment Prevention 0 Years 10 10+ Diagnosis Type 2 diabetes IFG/IG T IFG: impaired fasting glucose IGT: impaired glucose tolerance
The Ominous Octet Multiple defects contribute to the progression of T2D Decreased Incretin Effect Increased Lipolysis Decreased Insulin Secretion Increased Glucagon Secretion Increased Glucose Reabsorption Hyperglycaemia Islet-a cell Increased Decreased Glucose Uptake HGP Neurotransmitter Dysfunction Adapted from De Fronzo RA. Diabetes. 2009;58:773-95.
What is -cell dysfunction? Major defect in individuals with type 2 diabetes Reduced ability of -cells to secrete insulin in response to hyperglycemia DeFronzo RA, et al. Diabetes Care 1992; 15:318 354.
Now In the depth of -cell failure
Why does the -cell fail? Oversecretion of insulin to compensate for insulin resistance1,2 Glucotoxicity2 Lipotoxicity3 Chronic hyperglycemia High circulating free fatty acids Pancreas -cell dysfunction 1Boden G & Shulman GI. Eur J Clin Invest 2002; 32:14 23. 2Kaiser N, et al. J Pediatr Endocrinol Metab 2003; 16:5 22. 3Finegood DT & Topp B. Diabetes Obes Metab 2001; 3 (Suppl. 1):S20 S27.
Poor Sensing (Glucose insensitivity of beta-cells) Glucose Resistance !!
Management of hyperglycemia in type 2 diabetes -cell decline - Genetically predisposed (Genes set other than that predisposing for IR). - Overworking -cells in response to IR may lead to -cell exhaustion with endoplasmic reticulum stress ending in - cell failure - Glucotoxicity and lipotoxicity may have a role in -cell failure
Management of hyperglycemia in type 2 diabetes -cell exhaustion - A physiological depletion of B-cell insulin stores secondary to prolonged chronic stimulation with glucose on non- glucose secretagogues. - No defect in insulin synthesis. - The -cell function fully recovers as it rests. Exhaustion is reversible
Management of hyperglycemia in type 2 diabetes Glucotoxicity irreversible B-cell damage caused by chronic exposure to supra-physiological concentration with characteristic decreases in insulin synthesis and secretion caused by decreases insulin gene expression. Glucotoxicity is irreversible Nonphysiological and potentially glucose
Management of hyperglycemia in type 2 diabetes Depletion of insulin stores Pool-hypothesis I. Defective mobilisation II. insulin requirements Reserve-Pool RR-Pool ATP ADP Modified from Rorsman P, et al. News Physiol Sci 2000;15:72 7.
Interplay between -cell exhaustion & glucotoxicity Hyperglycemia Excess insulin secreation Prolonged hyperglycemia Beta-cell Rest Insulin depletion from -cell (Exhausion) More, prolonged hyperglycemia ER Stress Cytokines ROS Ca++ Irreversible -cell damge & apoptosis (Glucotoxicity)
Pancreatic islet morphology: structural defects are evident in type 2 diabetes Adapted from Rhodes. Science 2005;307:380 4
Management of hyperglycemia in type 2 diabetes Incretin concept response to the orally taken foods enhances the response of -cells to rising blood glucose. The physiologically released GLP-1 in DPP4 (very short half life, 1-2 min.) GLP-1 is readily degraded by the enzyme
Management of hyperglycemia in type 2 diabetes In type 2 Diabetes Small amounts of GLP-1 are released from the L-cells of the ileum, but -cells are still responding physiologically to the GLP-1. It is no yet settled, is GLP-1 reduction a cause or only an association with type 2 diabetes?!
L-Cell (ileum) ProGIP Proglucagon GLP-1 [7-37] GIP [1-42] K-Cell (jejunum) GLP-1 [7-36NH2] GLP-1=Glucagon-Like Peptide-1; GIP=Glucose-dependent Insulinotropic Peptide Adapted from Drucker DJ. Diabetes Care. 26:2929-2940.
Mechanisms of GLP-1 action: Role of incretins in plasma glucose regulation -cell stress Meal-induced secretion of GLP-1 Increased satiety Decreased appetite -cell response -cells: postprandial glucagon secretion Liver: glucagon decreases hepatic glucose production -cells: Stimulation of glucose dependent insulin secretion Stomach: slowing of gastric emptying Modified from Flint A, et al. J Clin Invest. 1998;101:515-520.; Larsson H, et al. Acta Physiol Scand. 1997;160:413-422.; Nauck MA, et al. Diabetologia. 1996;39:1546-1553.; Drucker DJ. Diabetes. 1998;47:159-169.
Insulin release : It involves 3 main steps : 1.Translocation of insulin granules. 2.Docking of insulin granules. 3.Fusion of insulin granules.
Translocation of insulin granules : Two essential components of the cytoskeletal elements : 1.Microtubules (formed of tubulin subunits). 2.Microfilaments (Actin + Myosin).
Microtubules form a network radiating from the perinuclear region outwords. The framework provides the mechanical pathway along which secretory granules move toward the exocytic sites close to the plasma membrane. It gives the way but not the force
The motive force to propel granules along the microtubules is provided by the interaction between : Filamentous actin Phosphorylated myosin + ATP Ca+ Granule transport It gives the force but not the way
Ca+ is essential for almost all steps involved in insulin release, thus factors increasing intracellular Ca+ will augment insulin release. Mechanisms involved in increasing intra- cytoplasmic Ca+ : Ca-influx from outside. Inhibition of Ca-reuptake by intracellulas stores. Increased Ca-sensitivity. Ca++Store x
Increased intracellular Ca+ is essential for granules translocation and fusion hence release of insulin. ATP-sensitive K+ channel Voltage-gate Ca channel Glucose 6 GLUT2 X Fusion 4 K retention Depolarization 3 Glucose Ca+ 2 5 Glucokinase 1 G-6-P ATP Translocation Each B-cell contains up to 500 Ca channels
The potentiating effect of GLP-1 is mediated through activation of adenyl cyclase : GLP-1 Adenyl cyclase ATP C-AMP Ca2+ uptake into stores PKA Cyclosolic Ca2+ Ca2+ sensitivity Insulin Release
Insulinotropic Effect of GLP-1 RA Ca2+ Voltage- dependent Ca2+ Channel K/ATP Chan nel ATP/A DP GKB Ca2+ Glucose transpor ter Insulin secretion cAMP Insulin vesikel GLP-1 Recep tor ATP Beta Cell Modified according to Gromada J, et al. Pflugers Arch Eur J Physiol. 1998;435:583-594; MacDonald PE, et al. Diabetes. 2002;51:S434-S442.
GLP-1 mainly and GIP Promote Glucose-Dependent Insulinotropic Activity in Healthy Subjects (n=7) Test Infusion Test Infusion 250 1,000 Glc Glc 200 800 Glucose (mg/dL) Insulin (pmol/L) 150 600 400 100 200 50 0 0 -50 -25 0 Time (min) 25 50 75 100 -50 -25 0 Time (min) 25 50 75 100 Saline GLP-1* GIP Glc = glucose *GLP-1 (7 36 amide) infused at 0.5 pmol/kg/min for 70 min GIP infused at 1.5 pmol/kg/min for 70 min Adapted from Kreymann B, et al. Lancet. 1987;2:1300 1304
GLP-1 acts at many levels to promote insulin secretion Potentiates glucose-dependent insulin secretion Enhances all steps of insulin biosynthesis Up-regulates insulin gene expression Up-regulates expression of genes essential for -cell function Promotes -cell neogenesis and progenitor cell differentiation* Inhibits apoptosis* Clinical Therapeutics/Volume 33, Number 5, 2011 Adapted from Holst JJ. Diabetes Metab Res Rev. 2002;18:430-441. *Observed in animal models
GLP-1 Controls Glucagon Secretion Suppresses glucagon release in glucose- dependent manner Enhances glucagon release in response to hypoglycemia Improves -cell glucose sensing Acts on specific G-protein coupled receptors on alpha-cells Dunning BE et al. Diabetologica. 2005;48:1700-13. Degn KB, et al. Diabetes. 2004; 54:2397-2403. Gromada J and Rorsman P Horm Metab Res 2004; 36:822-9.
In patients with Type 2 diabetes, incretin effect is either greatly impaired or absent, and it is assumed that this could contribute to the inability of these patients to adjust their insulin secretion to their needs Diabetologia (2004) 47:357 366
Control + GLP-1 Day 1 Day 3 Day 5 Farilla et al. Endocrinology. 2003
In genetically susceptible patients, -cell declines due to many factors (e.g.) glucotoxicity, lipotoxicity, IR, GLP1 deterioration . etc.
Correction of the underlying pathogenic factors early and intensively might preserve endogenous pancreatic functions.
RAPID INACTIVATION (DPP-4), SHORT ELIMINATION HALF-LIFE (1-2 MIN) NEED FOR CONTINOUS INFUSION OF GLP-1 NOT PRACTICAL FOR TREATMENT OF TYPE 2 DIABETES Drucker DJ, et al. Diabetes Care. 2003;26:2929-2940
Enzymatic cleavage of GLP-1 by DPP-4 inactivates GLP-1 DPP-4 GLP-1 30 1 2 3 Des-HA-GLP-1 (inactive) 1 2 3 30 Two possible solutions to utilize GLP-1 action therapeutically: 1) Long-acting DPP-4 resistant GLP-1 analogues / incretin mimetics 2) DPP-4 inhibitors / incretin enhancers Mentlein et al. Eur J Biochem. 1993; Gallwitz et al. Eur J Biochem. 1994
GLP-1 secretion is impaired in Type 2 diabetes Natural GLP-1 has extremely short half-life DPP- 4 inhibitors e.g.: Sitagliptin Vildagliptin GLP-1 analogues e.g.: Exenatide Liraglutide Oral agents Injectables Drucker. Curr Pharm Des. 2001; Drucker. Mol Endocrinol. 2003