The Female Reproductive System and its Functions
Explore the intricacies of the female reproductive system, including the ovary, oviduct, uterus, and vagina. Learn about the role of hormones, follicle development, and the menstrual cycle. Delve into the structure and functions of the different components, from the ovaries to the mammary glands.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
The female reproductive system consists of the ovary, oviduct, uterus and vagina. The oviduct, uterus and vagina have a common structure which is adapted for their particular functions. The breast or mammary glands are also considered here, as they are important during pregnancy.
The Ovary The ovary by gonadotrophin from the anterior pituitary. Ovaries also have an endocrine function - they release oestrogen and progesterone. The genital tract makes up the rest of the female reproductive system: fallopian tubestake the ova to the uterus. The uterus is a muscular organ, and its mucosal lining undergoes hormone dependent changes. The vagina is a muscular tube that leads to the outside. The ovaries are small almond shaped structures, covered by a thick connective tissue capsule - the tunica albuginea. This is covered by a simple squamous mesothelium called the germinal epithelium. The ovary has a cortex, which is where the ovarian follicles can be found, and a highly vascular medulla, with coiled arteries called arteries. The oocytes are surrounded by epithelial cells and form follicles. The ovary contains many primordial follicles, which are mostly found around the edges of the cortex. There are fewer follicles in different stages of development. ovary is where oogenesis occurs Ovaries are stimulated
Primordial germ cells multiply during fetal development. At birth, the ovary contains around 400 000 primordial follicles which contain primary oocytes. These primary oocytes do not undergo further mitotic division, and they remain arrested in the prophase I I, sexual maturity -At sexual maturity, two hormones, produced by the pituitary gland: follicle stimulating hormone (FSH) and lutenising hormone (LH) cause these primordial follicles to develop. In each ovarian cycle, about 20 primordial follicles are activated to begin maturation. however, normally only one follicle fully matures, and the rest contribute to the endocrine function of the ovary. -When activated, the first meiotic division is completed. When this happens, the primary follicle has matured into a secondary follicle Graafian follicle is formed. This contains a secondary oocyte. This second division is not completed, unless the ovum is fertilised. prophase stage of meiotic division meiotic division until secondary follicle. The second division then starts, and a
-The uterus is made up of an external layer of smooth muscle called the myometrium internal layer called the endometrium -The endometrium compactum the stratum -The Stratum spongialis during the first half of the menstrual cycle (proliferative phase) The wall of the uterus changes during the menstrual cycle, as shown diagramatically here. myometrium, and an endometrium. endometrium has three layers: stratum compactum, stratum stratum functionalis Stratum compactum spongialis develop into the stratum functionalis stratum stratum spongiosum functionalis) and stratum compactum and stratum spongiosum(which make up stratum basalis stratum basalis. -
In the proliferative phase the endometrium thickens, connective tissue is renewed, along with glandular structures and ehlicrine arteries. Oestrogen causes the endometrial stroma to become deep and richly vascularised. Simple tubular glands in the stratum functionalis the endometrium proliferative phase, facilitated by FSH, stratum functionalis open out onto the surface, and endometrium thickens.
-The vagina epithelium is stratified -Underneath the epithelium is a layer of lamina propria does not have any glands. -Under the lamina propria layer is a layer of smooth muscle and outer longitudinal layer. -Finally, there is an adventitial layer, which merges with that of the bladder (anteriorly) and rectum (posteriorly). vagina is a muscular tube. The lining stratified squamous squamous lamina propria, , which is rich in elastic fibres, and smooth muscle, which has an inner circular
The vagina which is derived from the rich vascular network, and mucus from glands in the labia minora. The smooth muscle contracts during/after coitus to keep the pool of semen close to the cervix. vagina is lubricated by cervical mucus,
The main functions of the male reproductive system, are to produce spermatozoa, androgens (sex hormones - principally testosterone) and to facilitate fertilisation, by introducing spermatozoa into the femal genital tract (copulation). The male reproductive system includes the testis, genital ducts, accessory sex glands and penis.
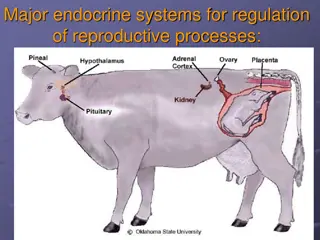
The pair of testes produces spermatozoa Several accessory glands constituents of semen. Long ducts store the sperm and transport them to the penis. The male reproductive system consists of paired testes glands are shown in this diagram. spermatozoa and androgens accessory glands produce the fluid androgens. testes and genital ducts glands and the penis genital ducts, accessory sex penis. The testes and ducts accessory sex
The genital ducts -The looped seminiferous the testes system fluid component of the semen to the outside. -This duct recti seminiferous tubules), the rete found in the mediastinum testis lead into the ductus -The ductus deferens duct to the outside. seminiferous tubules testes are connected to the genital duct system which transports the spermatozoa and tubules in genital duct duct system is made up of the tubuli recti (short straight tubules connected to the tubuli rete testis testis. The rete ductuli efferentes epididymus. . epididymus empties into the vas deferens, which empties into the ejaculatory duct, which empties into the urethra testis - which is rete efferentes that mediastinum testis testis empties into the ductuli ductus epididymus ductus epididymus vas ejaculatory urethra and passes
The epididymis -The ductulis epididymus are highly coiled, and make up a single tube in the epididymis that can be up to 6 metres long. This means that several sections of it can be found on a single slide. -The ductus spermatozoa that become matured here, and competent to fertilise ova. Fluid is absorbed here, and the epithlium is also secretory. -The epithelium is pseudostratified, with long immotile 'sterocilia' which are in fact very long microvilli. These are thought to be involved in absorption of fluid. The cells are also thought to be secretory, but the nature of the secretions is unknown. ductulis efferentes epididymus make up the epididymis efferentes and the ductus epididymis. These ducts ductus ductus epidymis epidymis is a storage reservoir for
-The production of sperm and eggs/ova (gametes) is a procedure called gametogenesis (spermatogenesis and oogenesis). Gametogenesis involves two rounds of meiotic cell division. -The germinal (seminiferous epithelium) of the seminiferous tubules contains spermatogenic cells -The spermatogenic then meiosis into sperm by the process of spermiogenesis spermatogenic cells and Sertoli spermatogenic cells divide by mitosis meiosis to form gametes Sertoli cells cells. mitosis, gametes, which mature spermiogenesis.