The Reproductive System Functions
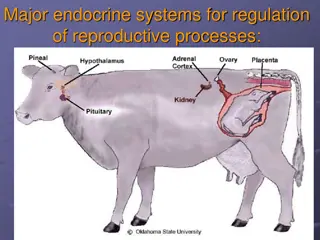
The male and female reproductive systems function differently, involving hormone regulation for testosterone, spermatogenesis, ovulation, and menstrual cycles. Delayed puberty can result from genetic factors or hormonal abnormalities in the body.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
THE REPRODUCTIVE SYSTEM
In the male, the testis has two principal functions: Synthesis of testosterone by the interstitial Leydig cells controlled by luteinising hormone (LH) 1 Spermatogenesis by Sertoli cells under the control of follicle- stimulating hormone (FSH). 2 Negative feedback suppression of LH is mediated principally by testosterone, while inhibin suppresses FSH.
In the female, sex hormones vary during the menstrual cycle FSH produces growth and development of ovarian follicles during the first 14 days. This leads to a gradual increase in oestradiolproduction which initially suppresses FSH secretion (negative feedback) but then, above a certain level, stimulates an increase in the frequency and amplitude of gonadotrophin- releasing hormone (GnRH) pulses, resulting in a marked increase in LH secretion (positive feedback). This LH surge induces ovulation. The follicle then differentiates into a corpus luteum which secretes progesterone. Withdrawal of progesterone results in menstrual bleeding
The cessation of menstruation (the menopause) occurs in developed countries at a median age of 50.8 yrs. In the 5 yrs before there is an increase in the number of anovulatory cycles, referred to as the climacteric. Oestrogenand inhibin secretion falls, resulting in increased pituitary secretion of LH and FSH.
DELAYED PUBERTY Genetic factors influence the timing of the onset of puberty, although body weight acts as a trigger. Puberty may be considered delayed if it has not begun by a chronological age >2.5 standard deviations (SD) above the national average (>14 in boys, >13 in girls in the UK). The key issue is to determine whether the delay in puberty is because the clock is running slow (constitutional delay) or because of pathology in the hypothalamus/ pituitary (hypogonadotrophic hypogonadism) or the gonads (hypergonadotrophic hypogonadism).
DELAYED PUBERTY The key issue is to determine whether the delay in puberty is because the clock is running slow (constitutional delay) or because of pathology in the hypothalamus/ pituitary (hypogonadotrophic hypogonadism) or the gonads (hypergonadotrophic hypogonadism).
CAUSES OF DELAYED PUBERTY AND HYPOGONADISM Hypogonadotrophic hypogonadism Hypergonadotrophic hypogonadism Constitutional delay Structural hypothalamic/pituitary disease Functional gonadotrophin deficiency Chronic systemic illness (e.g. asthma, coeliac disease, cystic fi brosis) Psychological stress, anorexia nervosa, excessive exercise Endocrine disease: hyperprolactinaemia, Cushing s, hypothyroidism Isolated gonadotrophin deficiency (Kallmann s) Chemotherapy/radiotherapy to gonads Gonadal trauma/surgery, cryptorchidism Autoimmune gonadal failure Mumps, TB, haemochromatosis Klinefelter s/Turner s syndrome
Constitutional delay This should be considered a normal variant and is the most common cause of delayed puberty. Affected children are typically shorter than their peers throughout childhood. There is often a family history and bone age is lower than chronological age. Puberty will start spontaneously, but prolonged delay can have significant psychological consequences
Hypogonadotrophic hypogonadism: This may be due to structural, infl ammatoryor infi ltrative disorders of the pituitary/hypothalamus (p. 373). Other pituitary hormones are likely to be defi cient. Functional gonadotrophin defi ciency is caused by a variety of factors (see Box 10.8). Isolated gonadotrophin defi ciency is due to a genetic abnormality affecting GnRH or gonadotrophin synthesis. The most common form is Kallmann s syndrome which is also associated with olfactory bulb agenesis, resulting in anosmia. If left untreated, the epiphyses fail to fuse, resulting in tall stature with disproportionately long arms and legs (eunuchoid habitus). Cryptorchidism (undescended testes) and gynaecomastia are seen in all forms of hypogonadotrophic hypogonadism
Hypergonadotrophic hypogonadism: Hypergonadotrophichypogonadism associated with delayed puberty is usually due to sex chromosome abnormalities (Klinefelter s/Turner s syndromes, p. 356). Other causes of primary gonadal failure are shown in Box 10.8.
Investigations Height should be plotted on centile charts. Key measurements are LH/ FSH, testosterone, oestradiol, FBC, renal, liver and thyroid function, and coeliac disease autoantibodies. Chromosome analysis is performed if gonadotrophin concentrations are elevated. If gonadotrophin concentrations are low, the differential diagnosis lies between constitutional delay and hypogonadotrophichypogonadism. A wrist X-ray allows estimation of bone age Neuroimaging is required in hypogonadotrophichypogonadism.
Management Puberty can be induced using low doses of oestrogen or testosterone Higher doses carry a risk of early fusion of epiphyses and therefore therapy should be administered and monitored by a specialist. In constitutional delay, therapy is withdrawn once puberty is established. In other cases, hormone doses are gradually increased during puberty and full adult replacement doses given when development is complete.
MALE HYPOGONADISM The clinical features of both hypo- and hypergonadotrophic hypogonadism in men include: Decreased frequency of shaving Muscle weakness Loss of libido Lethargy Delayed puberty Erectile dysfunction Gynecomastia Infertility
Management Testosterone replacement is indicated to prevent osteoporosis and to restore muscle power and libido. Testosterone administration should be avoided in prostatic carcinoma. In men over 50, prostate-specifi c antigen (PSA) should be monitored Men with hypogonadotrophic hypogonadism who wish fertility are usually given injections of hCG. Extraction of sperm from the epididymis, in vitro fertilisation and intracytoplasmic sperm injection (ICSI) are used in primary testicular disease
GYNAECOMASTIA Gynaecomastia is the presence of glandular breast tissue in males, resulting from an imbalance between androgen and oestrogen activity (androgen defi ciencyor oestrogen excess). Causes are listed in the next slide. The most common are physiological, i.e. in the newborn baby (maternal oestrogens), in pubertal boys (oestradiol concentrations reach adult levels before testosterone) and in elderly men ( testosterone concentrations). Gynaecomastia is often asymmetrical.
CAUSES OF GYNAECOMASTIA Drug-induced: cimetidine, digoxin, anti-androgens (cyproterone acetate, spironolactone) Idiopathic Physiological Oestrogenexcess: liver failure (impaired steroid metabolism), oestrogen secreting tumor (e.g. testis), hCG-secreting tumor (e.g. testis, lung) Androgen resistance syndromes Hypogonadism
Palpation may allow breast tissue to be distinguished from adipose tissue observed in obesity. If a clinical distinction between gynaecomastiaand adipose tissue cannot be made, then USS or mammography is required. The testes should be examined for cryptorchidism, atrophy or a tumour. Testosterone, LH, FSH, oestradiol, prolactin and hCGshould be measured. Elevated oestrogenconcentrations are found in testicular tumours and hCG- producing neoplasms. The underlying cause should be addressed, e.g. changing drug treatments, excision of tumour In physiological gynaecomastia, reassurance is usually sufficient but if the condition is associated with significant psychological distress, surgical excision may be justified. Androgen replacement improves gynaecomastiain hypogonadal males.
HIRSUTISM Hirsutism refers to the excessive growth of thick terminal hair in an androgen- dependent distribution in women (upper lip, chin, chest, back, lower abdomen, thigh, forearm). It should be distinguished from hypertrichosis, which is generalised excessive growth of vellus hair.
Important observations are a drug and menstrual history, BMI, BP, examination for virilisation (clitoromegaly, deep voice, male-pattern balding, breast atrophy) and associated features, e.g. Cushing s syndrome. Recent hirsutism associated with virilisation is suggestive of an androgen- secreting tumour. Testosterone, prolactin, LH and FSH should be measured. If testosterone levels are over twice the upper limit of the normal female range, especially with LH and FSH, then causes other than idiopathic hirsutism and PCOS are more likely.