Thinking outside the [mirror] box
Explore the innovative approach of CRPS rehabilitation presented by Dr. Tara Packham, an occupational therapist with a background in hand rehabilitation and a focus on CRPS. Learn about evidence-based practice and the evolution of EBP in clinical decision-making. Discover clinical practice guidelines and recommended strategies for CRPS rehabilitation, including pain relief, education, physical rehabilitation, and psychological interventions.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
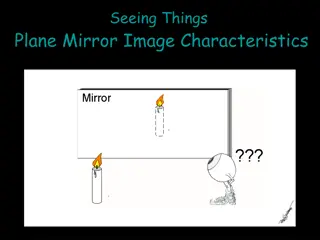
Thinking outside the [mirror] box for CRPS rehabilitation PARC Living with CRPS Meeting October 26, 2019 Dr. Tara Packham, OTReg(Ont), PhD 1
My background (and biases) Occupational therapist Hand rehabilitation Did a PhD focused on CRPS Active member of IASP special interest group on CRPS 2
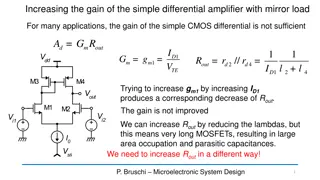
What is Evidence-Based Practice? The use of RESEARCH EVIDENCE RESEARCH EVIDENCE together with CLINICAL KNOWLEDGE CLINICAL KNOWLEDGE and REASONING REASONING to make decisions about interventions that are effective for a specific individual (Sackett, 1998) 3
Evidence Evidence- -based clinical decision making based clinical decision making Clinical Expertise (Haynes et al, (Haynes et al, 1996) 1996) Research Evidence Patient Wishes 4
The Evolution of EBP Clinical State & Person Context (Haynes et al 2002) (Haynes et al 2002) Today Today s talk will be about the best s talk will be about the best evidence with a dose of my evidence with a dose of my clinical experience, but clinical experience, but you will need to weigh that you will need to weigh that against your unique situation against your unique situation and experiences. and experiences. Clinical Clinical Expertise Expertise Best Research Evidence Patient Preference & Actions 5
Clinical practice guidelines for CRPS Most recent: Royal College of Physicians, UK Goebel et al, 2018 6
What is recommended for rehabilitation? Pain relief (medication and procedures) Education to support self- management Physical and vocational rehabilitation Psychological interventions Goebel et al, 2018 7
Pain, perception and plasticity: Pain, perception and plasticity: the 3 Ps the 3 Ps 8
What is pain? Nociception Nociception the detection of danger or threat High perception threshold High perception threshold Early warning system Usually this is acute pain Inflammatory pain Inflammatory pain Decreased perceptual threshold Decreased perceptual threshold (tenderness) Self-immobilization, protective behavior This can happen with both acute and persistent pain Pathological pain Pathological pain altered function of the nervous system Low threshold Low threshold - - Amplified sensory signals Includes nociplastic nociplastic (no actual damage) and neuropathic pain neuropathic pain (lesion in peripheral or central nervous system) (Woolf, 2010) This is what we think of with chronic pain 9
What is sensitization? Simply put: Peripheral sensitization Peripheral sensitization = inflammatory pain (lowered thresholds, evoked pain) Central sensitization Central sensitization = nociplastic pain (low threshold, spontaneous pain) Neuropathic pain may include elements of both (Woolf, 2011) 10
There are multiple sensitization mechanisms in CRPS (Gierthm hlen et al, 2014) TRAUMA TRAUMA Inflammatory responses Neurogenic inflammation Maladaptive neuroplasticity Peripheral Peripheral sensitization sensitization Oxidative stress Central Central sensitization sensitization 11
There are multiple sensitization mechanisms in CRPS TRAUMA TRAUMA Inflammatory responses Neurogenic inflammation Psychological Psychological Maladaptive neuroplasticity Peripheral Peripheral sensitization sensitization Oxidative stress distress distress Central Central sensitization sensitization 12
Mechanistic cascade (Gierthmhlen et al, 2014) Increased circulating stress hormones (cranky systems) Focal osteopenia (bone loss) Consequences of immobilization (muscle loss) Body perception disturbance (limb feels foreign) Dystonia (muscle cramps/spasms) Inflammatory signs (colour, temperature, swelling) Hyperalgesia, allodynia, spontaneous pain (hypersensitivity) Kinesiophobia, guarding, altered movement patterns (fear of movement) 13
Top down Top down Pain mechanisms and management Central sensitization Central sensitization Maladaptive neuroplasticity Neurogenic inflammation Oxidative stress Bottom up Bottom up Inflammatory responses Peripheral sensitization Peripheral sensitization 14
down down down down down down Top Top Top up up Top Top Top Bottom Bottom Bottom Bottom up up Pain relief (medication and procedures) Education to support self- management Physical and vocational rehabilitation Psychological interventions Goebel et al, 2018 15
Perception Body (periphery) Spinal cord Brain Stimulus Transmission Modulation Perception 16
Perception Modulation Modulation Perception Perception Response Response Stimulus Stimulus Transmission Transmission Bottom up Bottom up Top Down Top Down 17
CRPS is NOT Chronic Regional Pain Syndrome because of PLASTICITY If maladaptive plasticity are core to our understanding of the symptom mechanisms plasticity and altered perception perception then adaptive plasticity graded stimuli and response training) should reduce symptoms by normalizing the perceptions plasticity (including (Moseley & Flor, 2012; Mansour et al, 2014) 18
Bottom-up strategies Key principles: Control the inputs (stimuli) Make use of adaptive modulation Symptom management 19
Bottom-up strategies Control the pain inputs (stimuli) Control the pain inputs (stimuli) Minimize intermittent (evocative) stimuli (e.g. sheet lifter or swaddling ) adapting activities and environments Graded exposure to COMFORTABLE tactile and proprioceptive stimuli (not flooding if any signs of central sensitization sensory retraining vs. desensitization) Reduce oxidative stress by decreasing inflammation, increasing blood flow (e.g. prox. heat, deep breathing, compression wrapping) Mirror visual feedback (substituting vision for proprio?) (Packham & Holly, 2018; Packham et al, 2018; McCabe 2011) 20
Bottom-up strategies Make use of adaptive modulation Make use of adaptive modulation Consistent signalling raises the threshold for subsequent signals (e.g. gentle pressure from a compression wrap may decrease sensitivity to light touch) Comfortable stimulation of a related neuroanatomic Comfortable stimulation of a related neuroanatomic area area creates adaptive spinal cord response (convergence) TENS applied using above principle Stimpod? (radiofrequency stimulation) (Spicher et al, 2015; Lewis et al, 2014) 21
Symptom management Adapting activities and environments temperature sound navigation & attention movement patterns to minimize evocative elements Standard rehabilitation treatments like heat, stretching 22
Top down strategies Key principle: (Re)Train your brain: Use activities carefully to shape new perceptions (graded exposure) Get back to the joy of living System management 23
Top down strategies Take a Marie Kondo approach to activities Take a Marie Kondo approach to activities look for things that give and don t take for things that give and don t take Small steps to create success, new positive memories Graded motor imagery Laterality Motor imagery Mirror Box Bilateral rhythmic movements Familiar meaningful activities External focus (task, not movement)* look (Packham & Holly, in press; Gobeil et al, 2018) 24
Top down strategies Getting back to life Getting back to life (maybe a new one) Valued roles Graded environmental demands and contexts (graded exposure): new places, more things Pain neuroscience education Practice joy and hope Don t be a victim Cognitive behavioural therapy Acceptance and commitment therapy (Packham & Holly, in press; Gobeil et al, 2018; Rome, 2016) 25
System management Sleep management Stress & emotional management Inflammation & hormone management Edema control Diet? Opioid tapering and testosterone monitoring Activity & fatigue management Medication management (Goebel et al, 2018; Packham & Holly, 2018) 26
Questions? @TaraLPackham 27
References Bruehl S. Complex regional pain syndrome. BMJ. 2015 Jul 29;351:h2730. Gierthm hlen J, Binder A, Baron R, Gierthmuhlen J, Binder A, Baron R. Mechanism-based treatment in complex regional pain syndromes. Nat Rev Neurol. 2014;10(9):1-11. Grieve S, Perez RS, Birklein F, Brunner F, Bruehl S, Harden RN, et al. Recommendations for a first Core Outcome Measurement set for complex regional PAin syndrome Clinical sTudies (COMPACT). Pain. 2017;158(6):1083 90. Goebel A, Barker C, Turner-Stokes L, Atkins RM, Barker C, Cameron H, et al. Complex regional pain syndrome in adults: UK guidelines for diagnosis, referral and management in primary and secondary care. 2nd edition. London; 2018. Harden RN, Oaklander AL, Burton AW, et al. Complex regional pain syndrome: practical diagnostic and treatment guidelines. Pain Med. 2013;14:180-229. Harden RN, Maihofner C, Abousaad E, et al. A prospective, multisite, international validation of the Complex Regional Pain Syndrome Severity Score. Pain. 2017;158(8):1430-1436. Lewis JS, Coales K, Hall J, McCabe CS. Now you see it, now you do not : sensory-motor re-education in complex regional pain syndrome. Hand Ther. 2011;16(2):29-38. Llewellyn A, McCabe CS, Hibberd Y, et al. Are you better? A multi-centre study of patient-defined recovery from Complex Regional Pain Syndrome. Eur J Pain (United Kingdom). 2018;22(3):551 64. Mansour AR, Farmer MA, Baliki MN, Apkarian AV. Chronic pain: the role of learning and brain plasticity. Restor Neurol Neurosci. 2014;32(1):129 39. McCabe C. Mirror visual feedback therapy. a practical approach. J Hand Ther. 2011;24(2):170-179. 28
References Moseley GL, Flor H. Targeting cortical representations in the treatment of chronic pain: A review. Neurorehabil Neural Repair. 2012;26(6):646-652. Packham T, Holly J. Mechanism-specific rehabilitation management of complex regional pain syndrome: Proposed recommendations from evidence synthesis. J Hand Ther. 2018;31(1):10-19. Packham T, Holly J. Therapists management of complex regional pain syndrome. In Skirven et al (eds) Rehabilitation of the Hand (7th ed.) Packham T, Spicher CJ, MacDermid JC et al. Somatosensory rehabilitation for allodynia in complex regional pain syndrome of the upper limb: A retrospective cohort study. J Hand Ther. 2018;31(1):1-9. Packham T, MacDermid JC, Henry J, Bain JR. The Hamilton Inventory for Complex Regional Pain Syndrome: A cognitive debriefing study of the clinician-based component. J Hand Ther. 2012;25(1):97- 112. Packham TL, MacDermid JC, Michlovitz SL, Buckley N. Content validation of the Patient-Reported Hamilton Inventory for Complex Regional Pain Syndrome: Validit de contenu du Hamilton Inventory for Complex Regional Pain Syndrome, une mesure des r sultats d clar s par le patient. Can J Occup Ther. 2018. Rome L. The place of occupational therapy in rehabilitation strategies of complex regional pain syndrome: Comparative study of 60 cases. Hand Surg Rehabil. 2016;35(5):355-362. Spicher C, Quintal I, Vittaz M. Reeducation Sensitive Des Douleurs Neuropathiques. (3rd ed). Montpellier, France: Sauramps Medical, 2015. 29
References Woolf CJ. Central Sensitization: Implications for the diagnosis and treatment of pain. Pain. International Association for the Study of Pain; 2011;152(3 Supplemental):S2 15. Vlaeyen JWS, Crombez G, Linton SJ. The fear-avoidance model of pain. Pain. 2016; 157(8): 1588 9. Wall, P. D. And Melzack, R. (1994), Textbook of Pain, Churchhill Livingstone, New York, pp. 339- 345 Woolf CJ. What is this thing called pain ? J Clin Invest. 2010;120(11):10-12. Picture credits: Slide 6 https://commons.wikimedia.org/wiki/File:RSI-symptoms.jpg Slide 13 - https://www.publicdomainpictures.net/en/view- image.php?image=39356&picture=waterfall All other pictures authors own. 30
![Thinking outside the [mirror] box](https://cdn1.slideorbit.com/274498/thinking-outside-the-mirror-box-for-crps-n.jpg)