Thyroid Nodules and Cancers: Insights and Statistics
Understand the prevalence of thyroid nodules and cancers, with data on incidence rates, mortality, and malignancy percentages. Learn about diagnostic procedures, treatment options, and key features of thyroid malignancies.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
. 2 23 . . 40 . TSH= 8 T4= 8 g/dl (n=4.5-12.5) . T3 resine uptake= (THBR) mU/L (n= 0.4-5) T4 T4 TSH
. 2 23 40 . . . T3 resine uptake= TSH= 8 mU/L (n= 0.4-5) T4= 8 g/dl (n=4.5-12.5) . (THBR)
2 . . . TSH = 4.8 (n=0.4-0.5) FT4= 1.0 ng/dl (n= 0.7-2.0) FT4
T3= 240 ng/dl, . TSH<0.1 mU/L FT4= 2.0 ng/dl T4= 16.5 g/dl . Euthyroid T4 TSH
Thyroid nodules and cancers Thyroid nodules present in 4.2% of population (Women 6.4% Men 1.6%) Only 1/1000 of nodules is a clinically recognized thyroid cancer. Yearly incidence of Cancer 40/1,000,000 5 Deaths per million per year Thyroid cancer is the most frequent endocrine gland malignancies Accounting for 0.5-1.5% of all malignacies
Third generation TSH Free T4 TSH Normal High Low Thyroid Scan Hot nodule Cold nodule Workup and treatment of hypothyroidism if there is single dominant nodule FT4 High NL Observe I 131 RX Or Surgery FNA
US Features of Thyroid Malignancy Value and Limitation Microcalcification Marked Hypoechogenicity Irregular margin Absence of a hypoechoic halo Vascularity Lymphadenopathy & local invasion
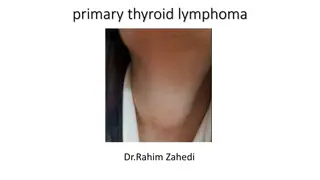
Papillary Carcinoma Poorly defined tumor with marked hypoechogenicity and irregular margins and without a yhpoechoic halo
Demonstration of nonsuction FNA of the thyroid (modified from reference (A) The needle is held directly between the thumb and the index finger. The nodule is immobilized with the index and middle fingers of the other hand. The needle is moved back and forth several times within the nodule with a rapid, gentle, stabbing motion
(Bengin) 90 53 70 20 15 16 (Inssufficient) ( suspicious) 23 5 10 (Malignat) 10 1 4
Calcitonin Screening 1. Highly sensitive tool for the presurgical diagnosis of MTC , far more sensitive than cytology. 2. Allows earlier diagnosis of MTC than the classical approach 3. Two recent independent reports one from Europe and the other from the U.S. suggested that CT screening is actually cost-effective Costante & Filetti. Occologist 2011; 16: 49.
Warning: False positives Smoking Renal failure Autoimmune thyroiditis Nonthyroidal neuroendocrine neoplasms Heterophilic antibodies Injury to thyroid tissue
Reasonable approach Selective aggressive case finding. Attention should be focused on clinical risk factors for MTC. 1. In affected families with documented RET mutations, basal and stimulated CT assays play pivotal roles in decisions regarding the timing of prophylactic surgery for mutation carriers 2. Periodic CT assays indicated for relatives of MTC patients belonging to the rare kindreds that are negative for RET mutations but still meet the clinical criteria for multiple endocrine neoplasia (MEN) 2A or MEN 2B Costante & Filetti. Occologist 2011; 16: 49.
Vigourous Screening More aggressive workup is needed: Thyroid nodules with clinical features that are suggestive of MTC 1.location in the upper third of a lobe 2.pain on palpation 3.Hypoechogenicity with microcalcifications 4.Lymph node abnormalities 5.Association with flushing and/or diarrhea).
RET Analysis RET analysis of MEN has revolutionized the management of children of families with MEN2 and allowed surgical prediction and prophylaxis to take place. The REarranged during Transfection (RET) proto-oncogene is the major etiologic factor in inherited medullary thyroid carcinoma (MTC) and is strongly associated with several clinical conditions such as multiple endocrine neoplasia types 2A and 2B (MEN2A and MEN2B), familial MTC, Hirschsprung s disease, papillary thyroid carcinoma. Moore SW. J Pediatr Surg 2007; 24: 326.
Features of papillary and follicular thyroid cancer
Changing Paradigms in the Management of Thyroid Cancer Risk Adapted Paradigm Management recommendations based individualized risk assessment Traditional Paradigm One Size Fits All Total thyroidectomy RAI remnant ablation All with same follow up Increased Emphasis Risk of death Risk of recurrence Risk of persistent disease Risk of failing initial therapy
Targeted Therapies What are our options? Systemic Therapies Chemotherapy/Novel Therapies Radioactive Iodine Embolization Surgery External Beam Radiation Often, multiple targeted therapies are used over the life time of a patient with advanced thyroid cancer
Risk stratification for the likelihood of clinically evident thyroid cancer recurrence following complete resection of primary tumor in patients with no evidence of distant metastases at initial evaluation
Risk of Structural Disease Recurrence Risk stratification by category Risk stratification within categories* High Risk Gross extrathyroidal extension incomplete tumor resection, or distant metastases FTC, extensive vascular invasion (30-55%) pT4a gross ETE (23-40%) PTC, vascular invasion (16-30%) pN1, any LN > 3 cm (27%) Clinical N1 (22%) Intermediate Risk N1 disease, minor extrathyroidal extension vascular invasion, or aggressive histology pN1, > 5 LN involved (19%) pT3 minor ETE (3-8%) pN1, all LN < 0.2 cm (5%) pN1, < 5 LN involved (4%) Intrathyroidal 2-4 cm PTC (5-6%) Multifocal PMC (4-6%) Low Risk Intrathyroidal DTC Minimally invasive FTC (0-7%) Unifocal PMC (1-2%)
First Example Patient 32 yr old male Total thyroidectomy 1.9 cm unifocal Intrathyroidal PTC No lymph nodes were sampled RAI Ablation Yes or No? 2-3 months post-op: Tg 1 ng/mL TSH was 1 mIU/mL Tg Ab negative Neck US is normal
32 yr old male Total thyroidectomy, 1.9 cm intrathyroidal PTC Risk Without RRA Recurrence 2-4% Disease Specific Mortality < 1% Distant Metastases about 1% Risks of RAI Potential Benefits of RAI Facilitate Staging/Follow-up +/- Recurrence No impact on mortality Permanent dry mouth 1-2% Blocked tear duct 1% Second cancer < 1% Tilting the Balance Toward Benefit Selective Use Lower administered activities (30 mCi) rhTSH preparation Using RAI as salvage therapy
Risk of Structural Disease Recurrence My personal practice as of Jan 2014 Risk stratification by category Risk stratification within categories* High Risk RAI given Probably withdrawal 150 mCi FTC, extensive vascular invasion (30-55%) pT4a gross ETE (23-40%) PTC, vascular invasion (16-30%) pN1, any LN > 3 cm (27%) Clinical N1 (22%) Intermediate Risk Selective use rhTSH or withdrawal 0 to 30 to 150 mCi depending on risk pN1, > 5 LN involved (19%) pT3 minor ETE (3-8%) pN1, all LN < 0.2 cm (5%) pN1, < 5 LN involved (4%) Intrathyroidal 2-4 cm PTC (5-6%) Multifocal PMC (4-6%) Low Risk Usually no RAI If given, 30 mCi rhTSH Minimally invasive FTC (0-7%) Unifocal PMC (1-2%)
RAI ablation is recommended for: All patients with known distant metastases, gross extrathyroidal extension of the tumor regardless of the rumor regardless of tumor size, or primary tumor size >4 cm even in the absence of other higher risk features. Selected patients with 1-4 cm thyroid cancers confined to the thyroid, who have documented lymph node metastases, or other higher risk features. RAI ablation is not recommended for: For patients with univocal cancer <1 cm without other higher risk features. The American Thyroid Association Guideline. Thyroid 2009; 19: 1167 42
Second Example Patient RAI Ablation Yes or No? 22 year old female Total thyroidectomy & left MRN dissection 2.5 cm, multifocal, well differentiated PTC 20/32 lymph nodes positive No extrathyroidal extension No vascular invasion
22yr old female Total thyroidectomy, 2.5 cm intrathyroidal PTC, N1b Risk Without RRA Recurrence 25-30% Disease Specific Mortality < 1% Distant Metastases about 5-10% What if her post-operative Tg was <0.2 ng/mL (TSH of 56 mU/L, no Tg antibodies)? Risks of RAI Potential Benefits of RAI Facilitate Staging/Follow-up +/- Recurrence No impact on mortality Permanent dry mouth 1-2% Blocked tear duct 1% Second cancer < 1% Tilting the Balance Toward Benefit Selective Use 100 mCi rhTSH?
Changing Paradigms in the Management of Thyroid Cancer Risk Adapted Paradigm Management recommendations based individualized risk assessment Traditional Paradigm One Size Fits All Total thyroidectomy RAI remnant ablation All with same follow up Increased Emphasis Risk of death Risk of recurrence Risk of persistent disease Risk of failing initial therapy