Transforming Health Payment Systems for Integrated Care Models
Explore how All-Payer Pilots and Payment Reform initiatives aim to bridge the gap between whole-person care practices and cost-conscious health payment models. Discover the potential of integrating social determinants of health (SDOH) in team-based care to enhance patient outcomes, population health, and health equity while addressing the challenges in payment structures and metrics alignment.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
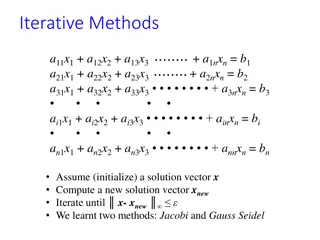
Presentation Transcript
All-Payer Pilots: Payment Reform and/or Health Reform ASLME Health Law Professors Conference 2024 John V. Jacobi Seton Hall Law School John.Jacobi@shu.edu @johnjacobi6
Can health insurance be structured/motivated to support whole-person care practices? Team-based care models integrating levels of medical care with social services responsive to SDOH show promise Health payment systems have been slow to support/utilize these models (with some exceptions) Goal: see consilience between WPC models for care and cost- conscious models in health payment practices Can two new CMS initiatives do more to wed practice transformation to payment reform? All-Payer Health Equity Approaches and Development (AHEAD) Model Making Care Primary (MCP) Model
Integrated care addressing SDOH Well-developed models transform care (usually primary care) to address SDOH/HRSN Team-based innovations are based on insight that failure to address social (e.g., homelessness, limited access to nutritious food), behavioral health (i.e., substance misuse, anxiety disorder), and medical/chronic conditions (e.g., diabetes, HBP) together can have disastrous consequences for: Health of individual patients Health of populations Health equity Cost of care
Integrating payment? The match between public and private insurance on one hand and whole-person primary care remains clunky because, inter alia, Path dependence: even in managed or integrated programs, payment for services continues to include FFS The ROI is uncertain particularly if the return redounds to the benefit of someone other than the sponsor Confusion over metrics and quality measures applicable in many VBP models frustrates health providers, impedes signals
Origin of this paper Seton Hall s long-term project to advance Community Health Workers professionalization focused us on payment streams Focus on codes, case payments, etc. for Medicaid, Medicare, commericals But many of those systems include outcomes/process metrics for payment; should health systems pay for CHW services out of operating revenue? initial response no. But more recently, Anecdotal evidence that systems with more comprehensive VBP mechaisms such as total cost of care contracts have moved to use of CHWs, LCSWs, navigators, etc., for the purposes social care models have been advocating Consilience here would mean leapfrogging discrete code/case based payments to incorporate social care into standard practices Shift from medical care to health care
What needs to be leapfrogged: Medicaid The move to Medicaid Managed Care in the 90s 10s organized payment at the top level, but MCOs often continued to pay FFS There are bright spots: Some 1115 waiver programs are innovative in this regard: Oregon s use of Coordinated Care Organizations with geographically-defined population health responsibilities and SDOH obligations is bearing fruit NY s 1115 program will use regional, mission-based organization to foster collaboration and coordination for social and medical care Some states are using their Medicaid contracts with old-fashioned MCOs (with CMS s encouragement, see CMS Dear State Health Official Letter #21-001) to require MCO collaboration with local NGOs to address SDOH
Medicare, commercial Medicare is an important payer for vulnerable, historically underserved people although it s not as central to the issue as is Medicaid Medicare done a few things: It has issued new Part B codes allowing payment for services related to patients Health Related Social Needs (see report from HLS CHLPI: https://www.healthlawlab.org/wp-content/uploads/2023/11/Review-of- CY-2024-PFS-Final-Rule-CHLPI-11-03-23.pdf) ACOs: both Medicare and commercial carriers use ACOs to create incentives for providers to collaborate and coordinate, but Most (not all) assessment measures are financial Evaluation of equity/SDOH effects are incomplete and sketchy Social gains not captured - they re external to the financial relationships
Global payment systems far from a silver bullet, but In theory, global payment systems particularly those incorporating all-payer (or many-payer) aspects have some success in Containing cost Supporting integrated medical care Supporting attention to the social/community needs of patients Some examples cited by CMS ins support of new pilots: Md. Total Cost of Care model (https://www.cms.gov/priorities/innovation/innovation-models/md-tccm) Vt. All-Payer ACO model (https://gmcboard.vermont.gov/content/APM/AboutTheAPM) Pa. Rural Health model (https://www.cms.gov/priorities/innovation/innovation-models/pa-rural-health-model)
Is TCOC contracting a means of advancing SDOH care? Hospital systems have often seen addressing social needs of patients as a special service, funded through grants, state programs ... Arguments have been made that this care can reduce patient costs, and might be funded out of operating expenses. It can be a hard sell But if, as our anecdotal evidence suggests, comprehensive contractual/payment programs induce hospitals systems to take responsibility for patient health in a meaningful way good, right? Can these two new CMS programs supply the jump-start?
High quality primary care was described by the NAS as whole person, integrated, accessible, and equitable health care delivered by interprofessional teams who are accountable for addressing the majority of an individual s health and wellness needs across settings and through sustained relationships with patients, families, and communities.
So, what do AHEAD and MCP add? Provide financial incentives for All-Payer (or, Many-Payer) systems, and for standardization of reporting requirements to lessen VBP fatigue Provide start-up, organizational funding and technical support to states and participants in the programs Offer mechanisms and financial incentives to structurally engage health-related social needs as part of a comprehensive business model (Bonuses? Tentative step to normalize rates between public and private payers Hand-holds for cost containment)
How might these programs advance emphasis on whole-person care? ACOs and (other) VBP programs had the effect of advancing, however fitfully, movements to integrate medical care across primary, specialty, and hospital services The ROI in most of existing programs is measured in cash (with some quality metrics as guardrails); treating people for their medical conditions at the right time in the right setting should save money, although the jury is out on how well These methods have been less successful at addressing non- medical determinants of health (although there have been some bright spots)
So how are these new programs different AHEAD and MPC models strive to provide financial and technical assistance to incorporate integration of social services into care in a systematic way Addressing SDOH/HRSN hasn t happened (much) as a market response to VBP models, in many cases because The benefits were externalized the benefits went beyond savings to the health insurance system, and therefore fell off the radar If this is just a market failure, or a variance of social and business goals, it is important to have government structure this aspect of the payer/provider relationship to internalize and/or require/incentivize pursuit of social goals
What will success look like? Diffusion of whole person care models; attention to social needs affecting health status; the rendering of care attentive to SDOH the default model Realistically? More attention to the problems, some funding for promising models, and a reduction in the fragmentation of billing/payment systems Hospital systems might reject AHEAD because they could lose their leverage to cost-shift to private insurance their perceived losses in public insurance The dangers? Medicalization of poverty, bridges to nowhere, frustration with attempts to broaden medical insurance into health insurance and, of course, just more of the same instead of innovation
Summing up Diffusion of whole-person care attentive to SDOH sometimes stalls at the hospital system and/or health insurance level Absent buy-in from systems and payers, primary care is on an unsustainable island Total cost of care models might bring incentives together AHEAD and MCP are intended to move the needle To work: States and hospitals must buy in (AHEAD) Primary care providers must buy in (MPC) (but hospitals have been buying primary care (again), so maybe the same audience?) The payment/monitoring must be workable but effective The feds must support the cost existing Medicare FFS payments can t be the sole standard of payment