Understanding Acne Vulgaris: Causes, Classifications, and Treatment
Learn about the common skin condition Acne Vulgaris, affecting millions in the US, its pathogenesis, classifications from mild to severe, and treatment options according to guidelines. Address the impact on mental health and the importance of managing it effectively to prevent scarring and emotional distress.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Acne Vulgaris Scott Stadler, Pharmacy Intern
Introduction Acne Vulgaris is a common skin condition in which pilosebaceous follicles are impacted through various inflammatory pathways This condition impacts approximately 50 million people across the United States Nearly 85% of teenagers experience acne, to some degree No mortality associated with acne vulgaris - why treat? Anxiety Depression Permanent scarring Journal of the American Academy of Dermatology. (2016). Guidelines of Care for the management of acne vulgaris. Retrieved from https://www.jaad.org/article/S0190-9622(15)02614-6/fulltext
Pathogenesis Involves several key pathways, and understanding of how each contributes is evolving: Follicular hyperkeratinization Microbial colonization with Propionibacterium acnes Inflammatory mechanisms involving both innate and acquired immunity Other mechanisms that are not as thoroughly understood: Neuroendocrine regulatory mechanisms Diet Genetics Journal of the American Academy of Dermatology. (2016). Guidelines of Care for the management of acne vulgaris. Retrieved from https://www.jaad.org/article/S0190-9622(15)02614-6/fulltext
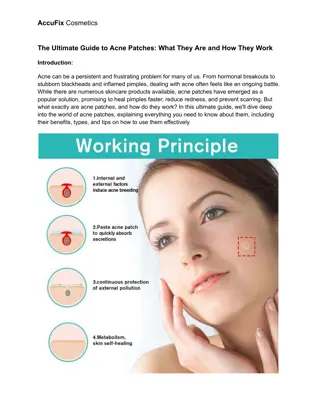
Classifications Mild acne vulgaris: Scattered, small (<5 mm), comedonal or inflamed papules or pustules without associated scarring Limited skin involvement (involvement of one body area or relatively few lesions in more than one body area) Absence of nodules Absence of near confluent skin involvement Moderate to Severe: Refer to provider Visually prominent acne consisting of many comedonal or inflamed papules or pustules Presence of nodules Involvement of multiple body areas with more than a few, scattered lesions Associated scarring Graber, E.. (2021). Acne Vulgaris: Overview of Management. In: UpToDate, Post, TW (Ed), UpToDate, Waltham, MA, 2021.
Classifications Moderate-Severe Mild Picture taken from: Yahia Albaili, DO, Dermatlas; http://www.dermatlas.org. Picture taken from: Douglas Hoffman, MD, Dermatlas; http://www.dermatlas.org.
Treatment Journal of the American Academy of Dermatology. (2016). Guidelines of Care for the management of acne vulgaris. Retrieved from https://www.jaad.org/article/S0190-9622(15)02614-6/fulltext
Treatment Journal of the American Academy of Dermatology. (2016). Guidelines of Care for the management of acne vulgaris. Retrieved from https://www.jaad.org/article/S0190-9622(15)02614-6/fulltext
Benzoyl Peroxide (BP) MOA: Releases free-radical oxygen which oxidizes bacterial proteins in the sebaceous follicles decreasing the number of anaerobic bacteria and decreasing irritating-type free fatty acids Can be used for mild papulopustular and mixed (comedonal and papulopustular) acne Available in many formulations: Gels, Creams, Lotions, Cleansers, Pads, Masks Available strengths range from 2.5%-10% 2.5% recommended for optimal benefit:side effect ratio Recommended use: Apply once daily Onset: Usually take 8-12 weeks for noticeable improvement Adverse reactions: hypersensitivity*, desquamation, contact dermatitis, redness Clinical Pearl: Can bleach clothing! Journal of the American Academy of Dermatology. (2016). Guidelines of Care for the management of acne vulgaris. Retrieved from https://www.jaad.org/article/S0190-9622(15)02614-6/fulltext
Topical Retinoids MOA: Decreases the cohesiveness of follicular epithelial cells and decreases micromedo formation. Additionally, stimulates mitotic activity and increased turnover of follicular epithelial cells causing extrusion of the comedones Can be used for comedonal acne Available in many formulations: Gels, Creams, Lotions, Foams Products available: Tretinoin, Adapalene*, Tazarotene, Trifarotene Most products typically applied once daily in the evening May see improvement beginning at week 2 to week 7 Adverse effects: irritation, dryness, and flaking of the skin, an effect most notable during the first month of therapy Patients may benefit by slowly titrating frequency/potency Journal of the American Academy of Dermatology. (2016). Guidelines of Care for the management of acne vulgaris. Retrieved from https://www.jaad.org/article/S0190-9622(15)02614-6/fulltext
Combination Therapy Topical Clindamycin can be combined with Benzoyl Peroxide or retinoids Clindamycin + Benzoyl Peroxide may be more efficacious than Benzoyl Peroxide alone Why not use Clindamycin alone? ANTIBIOTIC RESISTANCE Benzoyl Peroxide can be used in combination with retinoids Do not use tretinoin at same time as BP BP causes tretinoin to be less stable Other topical retinoids are less susceptible to this interaction Ideal to use BP in the morning and topical retinoid in the evening to avoid interaction altogether More effective than either agent used alone Journal of the American Academy of Dermatology. (2016). Guidelines of Care for the management of acne vulgaris. Retrieved from https://www.jaad.org/article/S0190-9622(15)02614-6/fulltext
Alternative Agents Salicylic acid Appropriate alternative for people who cannot tolerate retinoids Azelaic acid Antimicrobial and comedolytic properties Typically well tolerated Topical erythromycin Can be used in place of clindamycin Higher rates of resistance Ondo, W. G. (2021). Clinical features and diagnosis of restless legs syndrome and periodic limb movement disorder in adults. In: UpToDate, Post, TW (Ed), UpToDate, Waltham, MA, 2021.
Role of Diet in Acne? Data are limited Some research suggests that high glycemic index diets are associated with acne Important to note: there may be confounding variables When switching to LGI diet, participants lost weight, improved BMI, and improved insulin sensitivity Also, consumption of dairy products may be associated with acne Journal of the American Academy of Dermatology. (2016). Guidelines of Care for the management of acne vulgaris. Retrieved from https://www.jaad.org/article/S0190-9622(15)02614-6/fulltext
Hormonal Agents Estrogen-containing combined oral contraceptives are effective and recommended in the treatment of inflammatory acne in females Weigh risk vs. benefit Recommended moderate category, but use as monotherapy? Spironolactone is useful in the treatment of acne in select females Oral corticosteroid therapy can be of temporary benefit in patients who have severe inflammatory acne while starting standard acne treatment Journal of the American Academy of Dermatology. (2016). Guidelines of Care for the management of acne vulgaris. Retrieved from https://www.jaad.org/article/S0190-9622(15)02614-6/fulltext
Complementary/Alternative Medicine Beware of social media trends Often can pose unwanted risks Always advise patient to check with their doctor/pharmacist first Tea Tree Oil Some studies show efficacy equivalent to BP Safety data not robust, but may be better tolerated than BP Journal of the American Academy of Dermatology. (2016). Guidelines of Care for the management of acne vulgaris. Retrieved from https://www.jaad.org/article/S0190-9622(15)02614-6/fulltext
Take-home points Acne is a common skin condition and can impose severe mental health challenges for our patients Set realistic standards: It may take several weeks for patients to begin to see improvements after starting therapy, and the improvements may not reach their hopeful expectations Know which products you carry over-the-counter and counseling points Adverse reactions, timing, when to follow-up with doctor Assess whether the acne is mild enough to be treated OTC Clindamycin should not be used alone due to antibiotic resistance Help patients make safe decisions