Understanding Antiepileptic Drugs and Their Mechanisms
Discover how antiepileptic drugs like barbiturates and valproate work in the liver, their mechanisms of action, clinical uses, and potential drug interactions. Learn about phenobarbitone, mephobarbitone, primidone, and valproate as effective antiepileptic medications for various seizure types.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
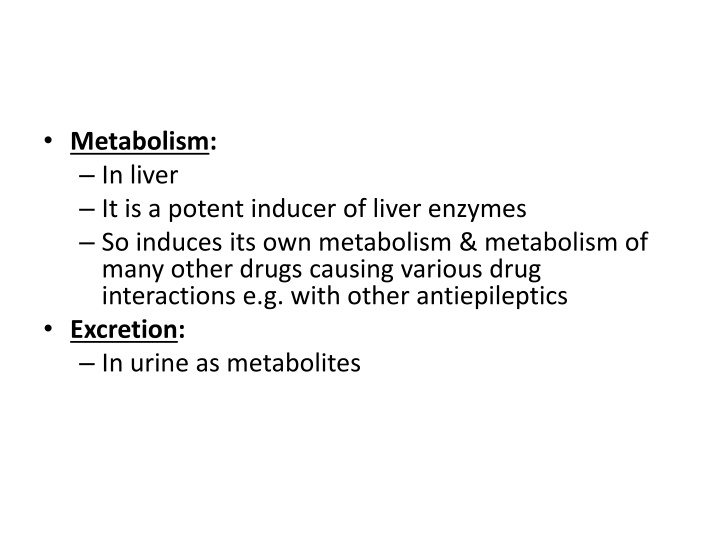
Metabolism: In liver It is a potent inducer of liver enzymes So induces its own metabolism & metabolism of many other drugs causing various drug interactions e.g. with other antiepileptics Excretion: In urine as metabolites
BARBITURATES Phenobarbitone: Oldest available antiepileptic. Mephobarbitone: Similar to phenobarbitone but may have lesser adverse effects Primidone: Uses & ADRs similar to phenobarbitone
Acts partly by converting into phenobarbitone but the mechanism is similar to phenytoin May be more effective than phenobarbitone but less than phenytoin and carbamazepine All Barbiturates are contraindicated in Porphyrias
Phenobarbitone Mechanism: GABA mediated neuronal inhibition Blocks Na+channels & Ca++channels at higher concentrations Clinical Use: Broad spectrum antiepileptic Partial seizures Generalized tonic clonic seizures But being a sedative drug, is only preferred in infants.
Carboxylic acids Valproate: Available as both valproic acid and its sodium salt, sodium valproate Divalproex: It is a 1:1 co-ordination complex of valproic acid & sodium valproate Its absorption is slow causing lesser side-effects Preferred by most patients
Valproate Mechanism: GABA levels in brain by inhibiting its degradation by GABA transaminase enzyme Na+channels Ca++channels (T-type) Clinical Use: Broad spectrum antiepileptic Generalized tonic clonic seizures: DOC Partial seizures
Absence seizures Atonic seizures: DOC Myoclonic seizures: DOC Infantile spasms Non-epileptic uses: Mood stabilizer & Migraine prophylaxis
Valproate Absorption: Good; Food delays absorption Can be given after meals to toxicity Distribution: Highly plasma protein bound It occurs in highly ionized form
Metabolism: In liver Excretion: In urine with a half life of 9-18 hours At high concentration follows zero order kinetics
Valproate: Adverse Effects Vomiting A lopecia: Hair loss Liver toxicity: Can be prevented by Carnitine ancreatitis: So, Contraindicated in alcoholics P R ashes O A T E edema taxia eratogenicity* (e.g. Spina bifida) and Tremors nzyme inhibition: Metabolism of Phenobarb. & Phenytoin
Newer Antiepileptics Gabapentin: GABA effect by ing its release Vigabatrin: GABA-ergic transmission either by acting as GABA agonist or by ing GABA transaminase enzyme It is reserved for use in resistant epilepsy
Tiagabine: GABA effect by ing its reuptake Lamotrigine: Blocks Na+ & Ca2+ channels Topiramate: Blocks Na+ & Ca2+ channels and GABA effect; Can cause weight loss
Zonisamide: Blocks Na+ & Ca2+ channels and GABA effect Felbamate: Blocks glutamate NMDA receptors; May produce fatal aplastic anemia & severe hepatitis; So reserved for resistant epilepsies like Lennox Gestaut Syndrome
Levetiracetam: Under development; Mechanism unknown No enzyme induction/ inhibition; Minimal interactions
Ethosuximide Mechanism: Main action: Blocks Ca++ channels (T-type) Other actions: Na+K+ATPase, Cerebral metabolism & GABA aminotransferase Clinical Use: Only in Absence seizures (Petit Mal): DOC
Pharmacokinetics: Completely absorbed & then distributes uniformly except in fat Not plasma protein bound Metabolized in liver & then excreted in urine with a half-life of 40 hours
Adverse effects: Very safe drug Gastric irritation is common Other adverse effects much less e.g. fatigue, headache, hiccups, rashes & blood dyscrasias Drug interaction:Valproate sethosuximide metabolism
Benzodiazepines Diazepam: I.V. or rectal administration is highly effective in status epilepticus Oral administration for long term epilepsy control is not very effective because of rapid development of tolerance Lorazepam: DOC in status epilepticus because of more efficacy & longer duration of action than Diazepam
Clonazepam: Is highly effective in absence seizures Also useful in myoclonic seizures & infantile spasms Nitrazepam: Used as an alternative to Clonazepam Clorazepate: Used as an adjuvant in complex partial seizures Clobazam: Useful in a variety of seizure types. Lesser sedation
Acetazolamide It is a diuretic Inhibits carbonic anhydrase enzyme Neuronal excitation Useful as an adjuvant to antiepileptics in all types of seizures But its usefulness is limited to only few weeks because of rapid development of tolerance