Understanding Antitubercular Drugs and Their Mechanisms of Action
Discover the classification of antitubercular drugs, including first-line oral agents, injectable anti-TB agents, fluoroquinolones, oral second-line agents, and agents with unclear roles in treating drug-resistant TB. Explore the cell envelopes of mycobacteria and mechanisms of action of key drugs like Isoniazid and Ethambutol. Uncover the intricate details of how these medications work to combat tuberculosis infections effectively.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Antitubercular Drugs Dr.B.Padma Asst. Professor Dept. of Pharmaceutical chemistry St Peters Institute of Pharmaceutical sciences Hanamkonda
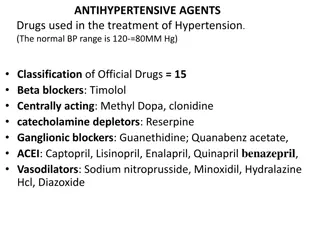
1.First line oral antitubercular agents Pyrazinamide Ethambutol 2.Injectable anti TB agents Amykacin Streptomycin
3.Flouroquinolones Moxifloxacin Ofloxacin 4.Oral second line antiTB agents Para-aminosalicylic acid Ethionamide Thioacetazone
5.Agents with unclear role in treatment of drug resistant TB Clofazimine Clarithromycin
Cell envelopes of mycobacteria The innermost layer of the mycobacterial cell envelope is composed of peptidoglycan and is lined by a layer of arabinogalactan. The presence of mycolic acids covalently bound to arabinogalactan, as well as the interaction of glycolipids and lipoglycans with mycolic acids in the outer layer, confers high hydrophobicity to the mycobacterial cell wall
Mechanism of action of Isoniazid Causes a decreased synthesis of mycolic acid. Mycolic acid is a constituent of mycobacterial cell wall that is thought to be responsible for the acid fastness of the bacteria. - Isoniazid is a prodrug that is activated on the surface of M. tuberculosis by katG enzyme to isonicotinic acid. Isonicotinic acid inhibits the bacterial cell wall mycolic acid, thereby making M. tuberculosis susceptible to reactive oxygen radicals. Isoniazid may be bacteriostatic or bactericidal in action, depending on the concentration of the drug attained at the site of infection and the susceptibility of the infecting organism. T he drug is active against susceptible bacteria only during bacterial cell division. Uses Isoniazid is an antibiotic used to treat mycobacterial infections; most commonly use in combination with other antimycobacterial agents for the treatment of active or latent tuberculosis. Adverse Reactions: - Peripheral neuropathy, elevated serum transaminases (SGOT; SGPT), bilirubinemia, bilirubinuria, jaundice, hepatitis (may be fatal), nausea, vomiting, epigastric distress, pancreatitis, blood dyscrasias, hypersensitivity reactions, hyperglycemia, pellagra, metabolic acidosis, rheumatic syndrome
Ethambutol (EMB) Mechanism of action - It causes inhibition of mycobacterial arabinosyl transferases which is involved in polymerization reaction of arabinoglycan, which is an essential component of mycobacterial cell wall. - It is also thought to inhibit RNA synthesis. Adverse effects It may cause fever and skin rashes. - It may cause optic neuritis and reduction in visual acuity. It may also cause a loss of red and green color discrimination Uses Ethambutol is used to treat tuberculosis (TB). It is used with other medicines for TB.
Pyrazinamide (PZA) Mechanism of action Pyrazinamide diffuses into the granuloma of M. tuberculosis, where the tuberculosis enzyme pyrazinamidase converts pyrazinamide to the active form pyrazinoic acid. - Under acidic conditions of pH 5 to 6, the pyrazinoic acid that slowly leaks out converts to the protonated conjugate acid, which is thought to diffuse easily back into the bacilli and accumulate. The net effect is that more pyrazinoic acid accumulates inside the bacillus at acid pH than at neutral pH. - Pyrazinoic acid was thought to inhibit the enzyme fatty acid synthase-I (FAS), which is required by the bacterium to synthesize fatty acids. - Pyrazinoic acid was proposed to bind to the ribosomal protein S1 (RpsA) and inhibit trans-translation process. Uses Pyrazinamide is an antibiotic that fights bacteria. Pyrazinamide is used to treat tuberculosis (TB) in adults and children Adverse effects The most common (approximately 1%) side effect of pyrazinamide is joint pains (arthralgia) - The most dangerous side effect of pyrazinamide is hepatotoxicity. - Other side effects include nausea and vomiting, anorexia, sideroblastic anemia, skin rash, urticaria, pruritus, dysuria, interstitial nephritis, malaise; rarely porphyria, and fever
Ethionamide (ETH) Mechanism of action Ethionamide (ETH) is a prodrug which is activated by the enzyme ethA, a mono-oxygenase in Mycobacterium tuberculosis, and then binds NAD+ to form an adduct (ETH-NAD) which inhibitory effect on the mycolic acid synthesis. Uses Ethionamide is an antibiotic used to treat tuberculosis. Specifically, it is used, along with other antituberculosis medications, to treat active multidrug-resistant tuberculosis. - Adverse effects Most common side effects: nausea, vomiting, diarrhoea, abdominal pain, excessive salivation, metallic taste, stomatitis, anorexia and weight loss. o Ethionamide can cause hepatocellular toxicity and is contraindicated in patients with severe liver impairment
Para-amino-salicylic acid (PAS) Para-amino-salicylic acid, also known as 4-Aminosalicylic acid. - Amino-salicylic acid is bacteriostatic against Mycobacterium tuberculosis (prevents the multiplying of bacteria without destroying them). - It also inhibits the onset of bacterial resistance to streptomycin and isoniazid Mechanism of action There are two mechanisms responsible for amino-salicylic acid's bacteriostatic action against Mycobacterium tuberculosis. o Amino-salicylic acid is an inhibitor of bacterial folate metabolism (inhibit Dihydrofolate reductase). o Amino-salicylic acid also inhibit the synthesis of the cell wall component, mycobactin, thus reducing iron uptake by M. tuberculosis. Adverse effects The most common side effect is gastrointestinal intolerance manifested by nausea, vomiting, diarrhea, and abdominal pain. - Hypersensitivity reactions: Fever, skin eruptions, dermatitis, or lymphoma-like syndrome, leucopenia, agranulocytosis, thrombocytopenia, hemolytic anemia, jaundice, hepatitis, hypoglycemia, optic neuritis, encephalopathy, Loeffler's syndrome, and vasculitis and a reduction in prothrombin
Rifampicin(R, RMP, RA, RF, or RIF) Mechanism of action of Rifampin Acts via the inhibition of DNA-dependent RNA polymerase, leading to a suppression of RNA synthesis and cell death. o Rifampin is bactericidal for mycobacteria. Human RNA polymerase is not affected by rifampin. Uses Rifampicin is a broad antibacterial spectrum antibiotic used to treat several types of mycobacterial infections including Mycobacterium avium complex, leprosy, and in combination with other antibacterial to treat latent or active tuberculosis. - Rifampin is bactericidal, and acts on both intracellular and extracellular organisms. - Adverse effects The most serious adverse effect is hepatotoxicity. The more common side effects include fever, gastrointestinal disturbances, rashes, and immunological reactions.
Rifabutin (Rfb) Mechanism of action Rifabutin acts via the inhibition of DNA-dependent RNA polymerase in gram-positive and some gram-negative bacteria, leading to a suppression of RNA synthesis and cell death Uses Rifabutin is a member of the class of rifamycins that is a semisynthetic antibiotic derived from Amycolatopsis rifamycinica. - A broad-spectrum antibiotic that is being used as prophylaxis against disseminated Mycobacterium avium complex infection in HIV-positive patients. - Rifabutin is now recommended as first-line treatment for tuberculosis. - Rifabutin is used in the treatment of Mycobacterium avium complex disease, a bacterial infection most commonly encountered in people with late-stage AIDS. - It has also found to be useful in the treatment of Chlamydophila pneumoniae infection. Adverse effects : Diarrhea , Stomach upset or pain ,Changes in taste , Nausea , Vomiting ,Belching Bloating ,Loss of appetite , Headache , Skin rash Rifabutin , Itching , Red, orange, or brown discoloration of your skin, tears, sweat, saliva, urine, or stools (this side effect is harmless and will disappear when the medication is stopped
Cycloserine (Cs) Mechanism of action Cycloserine disrupts D-alanine incorporation into peptidoglycan during bacterial cell wall synthesis. - Cycloserine is an analog of the amino acid D-alanine. It interferes with an early step in bacterial cell wall synthesis in the cytoplasm by competitive inhibition of two enzymes, L-alanine racemase, which forms D-alanine from L-alanine, and D-alanylalanine synthetase, which incorporates D-alanine into the pentapeptide necessary for peptidoglycan formation and bacterial cell wall synthesis. Uses Is a broad-spectrum antibiotic (may be bactericidal or bacteriostatic) used in the treatment of Tuberculosis and certain Urinary Tract Infections (UTI). -It is an antibiotic produced by Streptomyces garyphalus or S. orchidaceus. Cycloserine, is a GABA transaminase inhibitor and inhibition of peptidoglycan synthesis Adverse effects CNS: seizures, drowsiness, somnolence, headache, tremor, dysarthria, vertigo, confusion, memory loss, suicidal tendencies, psychosis, hyper-irritability, character changes, aggression, paresthesia, paresis, hyperreflexia, coma. CV: sudden-onset heart failure. Skin: rash. Other: hypersensitivity reactions (allergic dermatitis).
Mechanism of action Capreomycin inhibit protein synthesis by binding to the 70S ribosomal unit. - Capreomycin also binds to components in the bacterial cell which result in the production of abnormal proteins. These proteins are necessary for the bacteria's survival. - Therefore, the production of these abnormal proteins is ultimately fatal to the bacteria. Uses Capreomycin is an aminoglycoside antibiotic used as an adjunct drug in tuberculosis. - Capreomycin is effective against a number of Gram-positive and Gram-negative organisms but is primarily active against mycobacteria. It has been used in the treatment of certain resistant strains of Mycobacterium tuberculosis Adverse effects - High incidence: hematuria, urine output or urinary frequency significantly increased or decreased, loss of appetite or extreme thirst (hypokalemia, renal toxicity). - Less incidence: hearing loss, tinnitus, gait instability, dizziness, dyspnea, lethargy, extreme weakness (neuromuscular blockade, renal toxicity, hypokalemia), nausea or vomiting. - Significant renal toxicity: blood creatinine increase, blood urea nitrogen increase, poor creatinine clearance, proteinuria (need routine blood monitoring of renal functions and urine analysis) during usage of this medication. - Damaging to the 8th cranial nerve.
Streptomycin Mechanism of action Streptomycin is a protein synthesis inhibitor. It binds to the small S12 and 16S rRNA of the 30S subunit of the bacterial ribosome irreversibly, interfering with the binding of formyl- methionyl-tRNA to the 30S subunit. - This leads to codon misreading, eventual inhibition of protein synthesis and ultimately death of microbial cells. Adverse effects Vertigo, vomiting, numbness of the face, fever, and rash. Fever and rashes may result. - The most concerning side effects are kidney toxicity and ear toxicity. - Use is not recommended during pregnancy. - It is not recommended in people with myasthenia gravis. Uses An antibiotic used to treat a variety of infections including tuberculosis