Understanding Bacterial Infections and Mechanisms of Damage
Explore the pathology of bacterial infections, including common types like Staphylococcus and Streptococcus. Learn about bacterial classification, mechanisms of injury, and antibiotic resistance in Staphylococcus aureus. Discover how bacteria adhere to host cells, invade tissues, and deliver toxins, causing harm to the human body.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Bacterial infections part 1 Infection pathology
Plan Staphylococcus infection Streptococcus infection Pneumoccocus infection Neisseria infection Respiratory bacterial infection
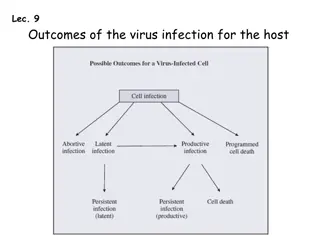
Bacteria Bacteria are classified by Gram staining (positive or negative), shape (spherical, rod-shaped) and need for oxygen (aerobic or anaerobic). Normal healthy people can be colonized by as many as 1012 bacteria on the skin, 1010 bacteria in the mouth, and 1014 bacteria in the gastrointestinal tract. There are at least 395 species of bacteria in the normal intestinal flora. Many bacteria remain extracellular when they invade the body, while others can survive and replicate either outside or inside of host cells ( facultative intracellular bacteria) and some grow only inside host cells (obligate intracellular bacteria).
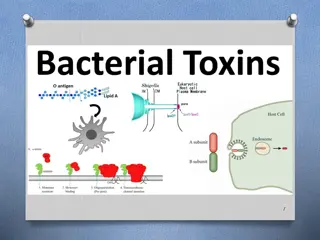
Mechanisms of Bacterial Injury BACTERIAL DAMAGE TO HOST TISSUES DEPENDS ON THE ABILITY OF THE BACTERIA TO ADHERE TO HOST CELLS, INVADE CELLS AND TISSUES, DELIVER TOXINS (ENDO OR EXO).
Staphylococcus infection It is one of the most common human infections. G+ cocci with a number of properties, main species Staphylococcus aureus, Staphylococcus epidermidis, Staphylococcus saprophyticus Staphylococcus aureus are pyogenic gram-positive cocci that form clusters like bunches of grapes.
Staphylococcus infection It is a part of mucous flora (nose, throat, hair, axillas, perineum) One third of people are colonized (carriers) Predisposition to infection is disorder of barrier functions and general weakening of organisms or immunodeficiency S. aureus possess a multitude of virulence factors, which include surface proteins involved in adherence, secreted enzymes that degrade proteins, and secreted toxins that damage host cells S. aureus produces multiple membrane-damaging (hemolytic) toxins, including -toxin, -toxin and -toxin and exfoliating toxins. Also they posses superantigens, who can activate T lymphocytes and lead to a secretion of cytokines and develop shok state.
Staphylococcus infection S. aureus can develop resistency to ATB. The most important are methicillin resistant staphylococci MRSA Also vancomycin resistant staphylococci VRSA are common part of nosocomial infection
Staphylococcus infection Reaction of tissues to staphylococci is purulent inflammation Due to staphylococcal coagulases it creates a bordered form abscess There are 3 groups of diseases: in the place of entering skin, respiratory system System infections Disorders due to toxins
Staphylococcus infection A furuncle, or boil, is a focal suppurative inflammation of the skin and subcutaneous tissue, either solitary or multiple or recurrent in successive crops. A carbuncle is a deeper suppurative infection that spreads laterally beneath the deep subcutaneous fascia and then burrows superficially to erupt in multiple adjacent skin sinuses. Hidradenitis is a chronic suppurative infection of apocrine glands most often in the axilla. Infections of the nail bed (paronychia) or on the palmar side of the fingertips (felons) are exquisitely painful. Staphylococcal lung infections have a polymorphonuclear infiltrate with tissue destruction. A predisposing condition is influenza. Staphylococcal scalded-skin syndrome, also called Ritter disease, most frequently occurs in children with staphylococcal infections of the nasopharynx or skin. There is a sunburn-like rash that spreads over the entire body and evolves into fragile bullae that lead to partial or total skin loss.
carbuncle furuncle Toxic epidermolysis Hidradenitis
Streptococcus infection Streptococci are gram-positive cocci that grow in pairs or chains and cause a myriad of suppurative infections of the skin, oropharynx, lungs, and heart valves. They are also responsible for a number of post-infectious syndromes, including rheumatic fever, immune complex glomerulonephritis, and erythema nodosum. -hemolytic streptococci are typed according to their surface carbohydrate antigens. S. pyogenes (group A) causes pharyngitis, scarlet fever, erysipelas, impetigo, rheumatic fever, TSS, and glomerulonephritis. S. agalactiae (group B) colonizes the female genital tract and causes sepsis and meningitis in neonates and chorioamnionitis in pregnancy. S. pneumoniae, the most important -hemolytic streptococcus, is a common cause of community-acquired pneumonia and meningitis in adults. S. mutans is the major cause of dental caries.
Streptococcus infection. Pathogenesis. The different species of streptococci produce many virulence factors and toxins. S. pyogenes, S. agalactiae, and S. pneumoniae have capsules that resist phagocytosis. S. pyogenes secrete a phage-encoded pyrogenic exotoxin that causes fever and rash in scarlet fever. Poststreptococcal acute rheumatic fever is probably caused by antistreptococcal M protein antibodies and T cells that cross-react with cardiac proteins. S. pyogenes have been referred to as flesh-eating bacteria because they cause a rapidly progressive necrotizing fasciitis. Pneumolysin is a cytosolic bacterial protein released on disruption of S. pneumoniae. S. mutans produces caries by metabolizing sucrose to lactic acid (which causes demineralization of tooth enamel).
Streptococcus infection. Streptococcal infections are characterized by diffuse interstitial neutrophilic infiltrates with minimal destruction of host tissues. The skin lesions caused by streptococci (furuncles, carbuncles, and impetigo) resemble those of staphylococci, although streptococci are less likely to cause the formation of discrete abscesses.
Streptococcus infection. Erysipelas is most common among middle- aged persons in warm climates and is caused by exotoxins from superficial infection with S. pyogenes. It is characterized by rapidly spreading erythematous cutaneous swelling that may begin on the face or, less frequently, on the body or an extremity. The rash has a sharp, well-demarcated, serpiginous border and may form a butterfly distribution on the face.
Streptococcus infection. At weakened patients we can observe invasive types os streptococci flesh eating bacteria They develop phlegmonous up to necrotizing inflammation It spreads in subcutis and soft tissues with muscle fascias necrotizing fasciitis
Streptococcus infection. Streptococcal pharyngitis is marked by edema, epiglottic swelling, and punctate abscesses of the tonsillar crypts, sometimes accompanied by cervical lymphadenopathy.
Streptococcus infection. Scarlet fever, associated with pharyngitis caused by S. pyogenes, is most common between the ages of 3 and 15 years. It is manifested by a punctate erythematous rash that is most prominent over the trunk and inner aspects of the arms and legs. The face is also involved, but usually a small area about the mouth remains relatively unaffected to produce a circumoral pallor.
Pneumoccocus infection S. pneumoniae is an important cause of lobar pneumonia Especially important at senior and immunocompromised patients It can produce not only respiratory infections, but invasive diseases including meningitis It has polysaccharide capsule which protects it against phagocytes
Pneumoccocus infection Local pneumococcal infection: inflammation of upper respiratory tract especially at children, it spreads to surrounding structures otitis and sinusitis. Later it can spread to meninges. Pneumococ is the most common cause for nosocomial pneumonia lobar pneumonia Invasive pneumococcal infection: after pneumonia it can spread via blood bacteriemia and development of general infection or infection in distant places arthritis, peritonitis, endocarditis.
Neisseria infection Neisseria are gram-negative diplococci that are flattened on the adjoining sides, giving the pair the shape of a coffee bean The two clinically significant Neisseria are N. meningitidis and N. gonorrhoeae.
Neisseria infection N. meningitidis is a significant cause of bacterial meningitis, particularly among children younger than 2 years of age. The organism is a common colonizer of the oropharynx and is spread by the respiratory route. Approximately 10% of the population is colonized. Invasive disease mainly occurs when people encounter new strains to which they are not immune, as may happen to young children or young adults living in crowded quarters such as military barracks or college dormitories. Even in the absence of pre-existing immunity, only a small fraction of people infected with N. meningitidis develop meningitis. The bacteria must invade respiratory epithelial cells and travel to the basolateral side of the cells to enter the blood. If N. meningitidis escapes the host response, the consequences can be severe. death rate is still about 10%.
Neisseria infection N. gonorrhoeae is an important cause of sexually transmitted disease (STD). Infection in men causes urethritis. In women, N. gonorrhoeae infection is often asymptomatic and so may go unnoticed. Untreated infection can lead to pelvic inflammatory disease Although N. gonorrhoeae infection usually manifests locally in the genital or cervical mucosa, pharynx, or anorectum, disseminated infections may occur. Disseminated infection of adults and adolescents usually causes septic arthritis accompanied by a rash of hemorrhagic papules and pustules. Neonatal N. gonorrhoeae infection causes blindness and, rarely, sepsis.
Respiratory bacterial infection Haemophilus influenza Whooping Cough Diphtheria
Haemophilus influenza Haemophilus influenzae is a pleomorphic gram-negative rod. They are divided according to serotype into groups a f, of which the most dangerous is group b. Virulence is conditioned by the presence of the capsule, non-encapsulated strains are part of the normal flora of the upper respiratory tract. The most virulent is type b. Pili enhance adherence, IgA protease. Diseases Hemophilic epiglottitis Pneumonia Otitis media Sinusitis Meningitis purulenta - mainly in children (most common etiological agent of meningitis up to 2 years). They are also at risk of permanent neurological damages. In adults, it is often a complication of an upper respiratory tract infections.
Haemophilus influenza Hemophilic epiglottitis - life-threatening, the child appears calm (saves breath), does not want to swallow (drooling), do not touch the throat much (there is a risk of laryngospasm), does not want to lie down (lying down can cause the epiglottis to bog down and result in death).
Whooping Cough Whooping cough, caused by the gram-negative coccobacillus Bordetella pertussis, is an acute, highly communicable illness characterized by paroxysms of violent coughing followed by a loud inspiratory whoop. B. pertussis vaccination, whether with killed bacteria or the newer acellular vaccine, has been effective in preventing whooping cough. Since the 1980s, however, rates of pertussis have been increasing. Bordetella pertussis colonizes the brush border of the bronchial epithelium and also invades macrophages. The toxin produced by B. pertussis paralyzes the cilia, thus impairing an important pulmonary defense. Bordetella bacteria cause a laryngotracheobronchitis that in severe cases features bronchial mucosal erosion, hyperemia, and copious mucopurulent exudate. Unless superinfected, the lung alveoli remain open and intact.
Diphtheria Diphtheria is caused by Corynebacterium diphtheriae, a slender gram-positive rod with clubbed ends, that is passed from person to person through aerosols or skin exudate. C. diphtheriae may be carried asymptomatically or cause illnesses ranging from skin lesions in neglected wounds of combat troops in the tropics, and a life-threatening syndrome that includes formation of a tough pharyngeal membrane and toxin-mediated damage to the heart, nerves, and other organs. C. diphtheriae produces only one toxin. A single molecule of diphtheria toxin can kill a cell. Immunization with diphtheria toxoid (formalin-fixed toxin) does not prevent colonization with C. diphtheriae but protects immunized people from the lethal effects of the toxin.
Diphtheria Inhaled C. diphtheriae proliferate at the site of attachment on the mucosa of the nasopharynx, oropharynx, larynx, or trachea but also form satellite lesions in the esophagus or lower airways. Release of exotoxin causes necrosis of the epithelium, accompanied by an outpouring of a dense fibrinosuppurative exudate. The coagulation of this exudate on the ulcerated necrotic surface creates a tough, dirty gray to black, superficial membrane. When the membrane sloughs off its inflamed and vascularizedbed, bleeding and asphyxiation may occur. With control of the infection, the membrane is coughed up or removed by enzymatic digestion, and the inflammatory reaction subsides. Although the bacterial invasion remains localized, generalized hyperplasia of the spleen and lymph nodes. The exotoxin may cause fatty change in the myocardium with isolated myofiber necrosis, polyneuritis with degeneration of the myelin sheaths and axis cylinders, and fatty change and focal necroses of parenchymal cells in the liver, kidneys, and adrenals.