Understanding Chronic Kidney Disease in Children
Learn about chronic kidney disease in children, including its definition, etiology, and pathogenesis. Discover the causes, progression, and impact on renal function, providing insights into this important pediatric health issue.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Chronic Renal Failure Chronic Renal Failure Dr Maria Darko
Definition Definition Chronic kidney disease (CKD) is defined as renal injury (proteinuria) and/or a glomerular filtration rate <60 mL/min/1.73 m2 for >3 mo. The prevalence of CKD in the paediatric population is approximately 18 per 1 million.
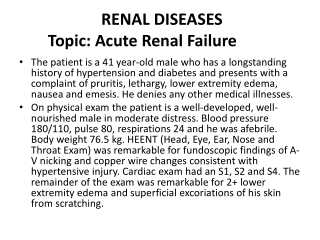
Aetiology Aetiology In children, CKD may be the result of congenital, acquired, inherited, or metabolic renal disease. The underlying cause correlates closely with the age of the patient at the time when the CKD is first detected. CKD in children < 5 yr old is most commonly a result of congenital abnormalities such as Renal hypoplasia, dysplasia Obstructive uropathy. Congenital nephrotic syndrome Prune belly syndrome Cortical necrosis Focal segmental glomerulosclerosis Polycystic kidney disease Renal vein thrombosis, and Hemolytic uremic syndrome.
Aetiology Aetiology After 5 yr of age causes of CKD include Acquired diseases (various forms of glomerulonephritis including lupus nephritis) and Inherited disorders (familial juvenile nephronophthisis, Alport syndrome). Metabolic disorders (cystinosis, hyperoxaluria) and certain inherited disorders (polycystic kidney disease) . This can occur occur throughout the childhood years.
Pathogenesis Pathogenesis There is progressive injury with ongoing structural or metabolic genetic diseases Renal injury can progress despite removal of the original insult. As nephrons are lost, the remaining nephrons undergo structural and functional hypertrophy characterized by an increase in glomerular blood flow. The driving force for glomerular filtration is thereby increased in the surviving nephrons.
Pathogenesis Pathogenesis This compensatory hyperfiltration temporarily preserves total renal function. It can however cause progressive damage to the surviving glomeruli This damage is by a direct effect of the elevated hydrostatic pressure on the integrity of the capillary wall and/or the toxic effect of increased protein traffic across the capillary wall. Over time, as the population of damaged nephrons increases, the surviving nephrons suffer an increased excretory burden This results in a vicious cycle of increasing glomerular blood flow and hyperfiltration injury.
Pathogenesis Pathogenesis Proteinuria can contribute to renal functional decline. Proteins that cross the glomerular capillary wall can exert a direct toxic effect on tubular cells and recruit monocytes and macrophages This enhances the process of glomerular sclerosis and tubulointerstitial fibrosis. Uncontrolled hypertension can worsen disease progression
Pathology Pathology Accumulation of nitrogenous waste Acidosis Electrolyte imbalance Renal bone disease ( Renal osteodystrophy) Growth retardation Anaemia Bleeding tendency Infection Neurologic symptoms GI symptoms Hypertension Hyperlipidemia Pericarditis Cardiomyopathy Glucose tolerance
Stages Stages
Clinical Manifestations Clinical Manifestations The clinical presentation of CKD is varied and depends on the underlying renal disease. Children and adolescents with CKD from chronic glomerulonephritis (membranoproliferative glomerulonephritis) can present with oedema, hypertension, hematuria, and proteinuria. Infants and children with congenital disorders can present in the neonatal period with failure to thrive, polyuria, dehydration, urinary tract infection, or overt renal insufficiency. Congenital kidney disease is diagnosed with prenatal ultrasonography in many infants.
Clinical Manifestations Clinical Manifestations The physical examination in patients with CKD can reveal pallor and an ill looking appearance. Patients with long-standing untreated CKD can have short stature and the bony abnormalities of renal osteodystrophy. Children with CKD due to chronic glomerulonephritis (or children with advanced renal failure from any cause) can have oedema, hypertension, and other signs of extracellular fluid volume overload.
Laboratory Findings Laboratory Findings Elevations in blood urea nitrogen and serum creatinine. Electrolyte imbalance - hyperkalemia, hyponatraemia (if volume overloaded), acidosis, hypocalcemia, hyperphosphataemia, and an elevation in uric acid. Heavy proteinuria can have hypoalbuminaemia. Normochromic, normocytic anaemia. Elevated serum cholesterol and triglyceride levels. If caused by glomerulonephritis, the urinalysis shows hematuria and proteinuria. If due to congenital lesions such as renal dysplasia, the urinalysis usually has a low specific gravity and minimal abnormalities by dipstick or microscopy.
Treatment Treatment The treatment of CKD is aimed at replacing absent or diminished renal functions, and slowing the progression of renal dysfunction Children with CKD should be treated at a paediatric centre capable of supplying multidisciplinary services, including medical, nursing, social service, nutritional, and psychological support. The management of CKD requires close monitoring of a patient's clinical and laboratory status.
Monitoring Monitoring Blood studies to be followed routinely include Serum electrolytes Blood urea nitrogen Creatinine Calcium Phosphorus Albumin Alkaline phosphatase, and Haemoglobin levels.
Monitoring Monitoring Periodic measurement of intact parathyroid hormone (PTH) levels and x-ray studies of bone may be of value in detecting early evidence of renal osteodystrophy. Echocardiography should be performed periodically to identify left ventricular hypertrophy and cardiac dysfunction that can occur as a consequence of the complications of CKD.
Principles of Management Principles of Management Fluid and electrolyte balance Sodium supplementation or restriction Fluid restriction Hyperkalemia may be treated by restriction of dietary potassium intake, administration of oral alkalinizing agents, and/or treatment with Kayexalate. Acidosis Sodium bicarbonate or sodium citrate Nutrition Growth Anaemia Bone disease Hypertension Immunizations Adjustments in drug dosage
Nutrition Nutrition Restrict dietary phosphorus, potassium, and sodium according to the individual patient's laboratory studies and fluid balance. In infants with CKD, formulas containing a reduced amount of phosphate (Similac PM 60/40) are commonly used. Protein intake should be 2.5 g/kg/24 hr and should consist of proteins of high biologic value that are metabolized primarily to usable amino acids rather than to nitrogenous wastes. The proteins of highest biologic value are those of eggs and milk, followed by meat, fish, and fowl.
Nutrition Nutrition Dietary intake should be adjusted according to response, optimally through consultation with a dietitian with expertise in childhood CKD. If oral caloric intake remains inadequate enteral tube feedings should be considered. Supplemental feedings may be provided via a nasogastric, gastrostomy, or gastrojejunal tube.
Nutrition Nutrition Children with CKD can become deficient in water-soluble vitamins either because of inadequate dietary intake or dialysis losses. These should be routinely supplemented Zinc and iron supplements should be added only if deficiencies are confirmed. Supplementation with fat-soluble vitamins A, E, and K is usually not required
Growth Growth Short stature is a significant long-term sequela of childhood CKD. Treatment with pharmacologic doses of recombinant human GH (rHuGH). Treatment may be initiated with rHuGH (0.05 mg/kg/24 hr) subcutaneously, with periodic adjustment in the dose to achieve a goal of normal height velocity for age. Treatment with rHuGH continues until the patient achieves a final adult height or undergoes kidney transplantation.
Anaemia Anaemia Anaemia in patients with CKD is primarily the result of inadequate erythropoietin production by the failing kidneys and usually becomes manifest in patients with stages 3-4 CKD. Other possible contributory factors include Iron deficiency Folic acid Vitamin B12 deficiency, and Decreased erythrocyte survival.
Anaemia Anaemia Recombinant human erythropoietin (rHuEPO) therapy has decreased the need for transfusion in patients with CKD. Erythropoietin is usually initiated when the patient's haemoglobin concentration falls below 10 g/dL Dose - 50-150 mg/kg/dose subcutaneously 1-3 times weekly.
Anaemia Anaemia The dose is adjusted to maintain the haemoglobin concentration between 11 and 12 g/dL, not more than 13 g/dL. All patients receiving rHuEPO therapy should be provided with either oral or intravenous iron supplementation. Patients who appear to be resistant to rHuEPO should be evaluated for iron deficiency, occult blood loss, chronic infection or inflammatory state, vitamin B12 or folate deficiency, and bone marrow fibrosis related to secondary hyperparathyroidism
Renal Bone Disease Renal Bone Disease Low-phosphorus diet for children and adolescents Infants should be provided with a low-phosphorus formula such as Similac PM 60/40. Phosphate binders are used to enhance faecal phosphate excretion - Calcium carbonate , Calcium acetate , non calcium-based binders such as sevelamer (Renagel). Vitamin D administration.
Hypertension Hypertension Salt-restricted diet (2-3 g/24 hr) Diuretic therapy Thiazide diuretics - CKD stages 1-3. Stage 4 CKD - loop diuretics (furosemide 1-2 mg/kg/dose bid or tid) become the diuretic class of choice.
Hypertension Hypertension Proteinuria - Angiotensin-converting enzyme (ACE) inhibitors (enalapril, lisinopril) and angiotensin II blockers (losartan) Calcium channel blockers (amlodipine), -blockers (propranolol, atenolol), and centrally acting agents (clonidine) in children with CKD whose blood pressure cannot be controlled using dietary sodium restriction, diuretics, and ACE inhibitors.
Immunizations Immunizations Should receive all standard immunizations according to the schedule used for healthy children. Withhold live vaccines from children with CKD related to glomerulonephritis during treatment with immunosuppressive medications. Administer live virus vaccines for measles, mumps, and rubella (MMR) and varicella before kidney transplantation because these vaccines are not advised for use in immunosuppressed patients.
Adjustment in Drug Dosage Adjustment in Drug Dosage This is important because many drugs are excreted by the kidneys Dosing might need to be adjusted in patients with CKD to maximize effectiveness and minimize the risk of toxicity. Strategies in dosage adjustment include Lengthening of the interval between doses Decreasing the absolute dose, or Both.
Halting Disease Progression Halting Disease Progression There are no definitive treatments to improve renal function in children with CKD Strategies that may be effective in slowing the rate of progression of renal dysfunction include : Optimal control of hypertension. Maintenance of serum phosphorus within the normal range for age to minimize renal calcium-phosphorus deposition. Prompt treatment of infectious complications and episodes of dehydration to minimize additional loss of renal parenchyma.
Halting Disease Progression Halting Disease Progression Correction of anaemia with erythropoietin therapy Control of hyperlipidemia Avoidance of cigarette smoking Prevention of obesity Minimization of use of nonsteroidal anti-inflammatory medications. Although dietary protein restriction has been shown to be useful in adults, this recommendation is generally not suggested for children with CKD because of the concern of adverse effects on growth and development
Prognosis Prognosis The prognosis for the infant, child, or adolescent with CKD has improved dramatically because of improvements in medical management (aggressive nutritional support, recombinant erythropoietin, recombinant growth hormone [rGH]), dialysis techniques, and kidney transplantation.
Conclusion Conclusion Management with medication , dialysis. Renal transplantation is curative Survival greatly improved by mechanisms that slow down disease progression.
Thank You Thank You Questions? Comments? Contributions?