Understanding Diabetic Ketoacidosis: Symptoms, Diagnosis, and Management
Diabetic Ketoacidosis (DKA) is a serious complication of Diabetes Mellitus characterized by high blood sugar levels, dehydration, and acidosis. Learn about the symptoms, diagnosis, and management of DKA, which can be life-threatening if not treated promptly.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
PRESENTED BY: DR. DR. ANAM ANAM MEHMOOD MEHMOOD
Case A 24 year old female with past medical history of diabetes mellitus I is brought to the ER by her mother with complaints of fatigue and increased thirst and urination. Of note patient states she ran out of her insulin last week. She also has had a runny nose and cough for the past week. She noticed her glucose levels have been running very high and got concerned. On Exam: BP 101/72; heart rate: 113; respirations: 32; Temperature: 36.8 BP 101/72; heart rate: 113; respirations: 32; Temperature: 36.8 100% on room air. 100% on room air. HEENT: dry mucous membranes HEENT: dry mucous membranes CV: CV: tachycardic tachycardic, normal s1, s2. No murmurs , normal s1, s2. No murmurs Lung: NVB+0 Lung: NVB+0 Abdomen: + Abdomen: +bs bs, non distended, slight tenderness to deep palpation, no rebound or , non distended, slight tenderness to deep palpation, no rebound or guarding guarding no cyanosis, clubbing or edema no cyanosis, clubbing or edema C; pulse oximetry: C; pulse oximetry:
Case (contin) LAB RESULTS LAB RESULTS EKG sinus tachycardia Biochemistry Na: 124, K: 5.0, Cl: 95 BUN: 38, Cr: 1.8 Glucose 450 AST:40, ALT:41, Alk phos:67 Arterial blood gas: pH 6.9, CO2 9, bicarb 10 WBC 13K, Hb14.4 mg/dL, and Hct 43.5%. 75% neutrophils
UA +glucose, +protein, -leuko esterase, -nitrite NO KETONES Serum ketones test ordered is positive for beta-hydroxybutyrate
Dibetic ketoacidosis Likely Diagnosis!!!!!
Dibetic Ketoacidosis DKA is a serious acute complications of Diabetes Mellitus. It DKA is a serious acute complications of Diabetes Mellitus. It carries significant risk of death and/or morbidity especially with carries significant risk of death and/or morbidity especially with delayed treatment. delayed treatment. The prognosis of DKA is worse in the extremes of age, with a The prognosis of DKA is worse in the extremes of age, with a mortality rates of 5 mortality rates of 5- -10%. 10%.
Dibetic Ketoacidosis: Definition A state of absolute or relative insulin deficiency aggravated by ensuing hyperglycemia, dehydration, and acidosis-producing derangements in intermediary metabolism, including production of serum acetone. Can occur in both Type I Diabetes and Type II Diabetes both Type I Diabetes and Type II Diabetes In type II diabetics with insulin deficiency/dependence The presenting symptom for ~ 25% of Type I Diabetics
Precipitating Factors: New onset of type 1 DM: 25% New onset of type 1 DM: 25% Infections (the most common cause): 40% Infections (the most common cause): 40% Drugs: e.g. Steroids, Thiazides, Dobutamine & Drugs: e.g. Steroids, Thiazides, Dobutamine & turbutaline turbutaline. . Omission of Insulin: 20%. This is due to: Omission of Insulin: 20%. This is due to: Non Non- -availability (poor countries) availability (poor countries) fear of hypoglycemia fear of hypoglycemia rebellion of authority rebellion of authority fear of weight gain fear of weight gain stress of chronic disease stress of chronic disease
Assessment: Assessment: History: History: Symptoms of hyperglycemia, precipitating factors Symptoms of hyperglycemia, precipitating factors diet and insulin dose. diet and insulin dose. Examination: Examination: Look for signs of dehydration, acidosis, and electrolytes imbalance, Look for signs of dehydration, acidosis, and electrolytes imbalance, including shock, hypotension, acidotic breathing, CNS status etc. including shock, hypotension, acidotic breathing, CNS status etc. Look for signs of hidden infections (Fever strongly suggests infection) Look for signs of hidden infections (Fever strongly suggests infection) and If possible, obtain accurate weight before starting treatment. and If possible, obtain accurate weight before starting treatment.
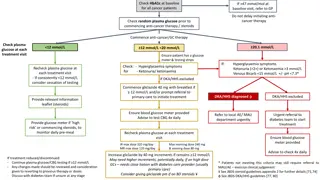
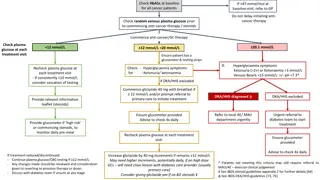
Management: The management steps of DKA includes: The management steps of DKA includes: Assessment of causes & Assessment of causes & sequele sequele of DKA by taking a short history & of DKA by taking a short history & performing a brief examination. performing a brief examination. Quick diagnosis of DKA at the ER. Quick diagnosis of DKA at the ER. Baseline investigations. Baseline investigations. Treatment, Monitoring & avoiding complications. Treatment, Monitoring & avoiding complications. Transition to outpatient management. Transition to outpatient management.
Diagnosis: You should suspect DKA if a diabetic patient presents with: You should suspect DKA if a diabetic patient presents with: Dehydration. Dehydration. Acidotic ( Acidotic (Kussmaul Kussmaul s s) breathing, with a fruity smell (acetone). ) breathing, with a fruity smell (acetone). Abdominal pain & Abdominal pain &\ \or distension. or distension. Vomiting. Vomiting. An altered mental status ranging from disorientation to coma. An altered mental status ranging from disorientation to coma.
Diagnosis: To diagnose DKA, the following criteria must be To diagnose DKA, the following criteria must be fulfilled : fulfilled : 1. 1. Hyperglycemia Hyperglycemia: of > 300 mg/dl & : of > 300 mg/dl & glucosuria glucosuria 2. 2. Ketonemia and ketonuria Ketonemia and ketonuria 3. 3. Metabolic Metabolic acidosis mmol mmol/l. Anion gap >10. /l. Anion gap >10. acidosis: : pH < 7.25 pH < 7.25, serum bicarbonate < 15 , serum bicarbonate < 15 Anion gap= [Na]+[K] Anion gap= [Na]+[K] [Cl]+[HCO3]. [Cl]+[HCO3]. This is usually accompanied with severe This is usually accompanied with severe dehydration and electrolyte imbalance. dehydration and electrolyte imbalance.
Diagnostic Criteria for DKA: Diagnostic Criteria for DKA: Mild DKA Mild DKA Moderate DKA Moderate DKA Severe DKA Severe DKA Plasma glucose Plasma glucose (mg/ (mg/dL dL) ) Arterial pH Arterial pH > 250 > 250 > 250 7.25-7.30 7.00-7.24 < 7.00 Sodium Sodium Bicarbonate Bicarbonate ( (mEq mEq/L) /L) Urine Ketones Urine Ketones 15 18 10 - <15 < 10 Positive Positive Positive Serum Ketones Serum Ketones Positive Positive Positive Serum Osmolality Serum Osmolality ( (mOsm mOsm/kg) /kg) Anion Gap Anion Gap Variable Variable Variable > 10 > 12 > 12 Mental Status Mental Status Alert Alert/Drowsy Stupor/Coma
Diagnostic Studies in DKA Chemistry Chemistry Glucose Bicarbonate Anion gap = (Na Anion gap = (Na+ +) ) (Cl Frequently seen: BUN/ /creatinine (dehydration) potassium sodium Pseudohyponatremia Pseudohyponatremia: to correct, add 1.6 of glucose above normal of glucose above normal (Cl- -+ HCO + HCO3 3- -) ) add 1.6 mEq mEq of sodium to every 100mg/ of sodium to every 100mg/dL dL Serum acetones Serum acetones Positive in DKA
Diagnostic Studies in DKA (continued..) Urinalysis Urinalysis Ketones (for DKA); leukocyte esterase, WBC (for UTI) CBC CBC Leukocytosis (possible infection) Amylase/Lipase Amylase/Lipase To evaluate for pancreatitis BUT, DKA by itself can also increase them! EKG EKG Evaluate for possible MI
MANAGEMENT: Correction of fluid loss with intravenous fluids Correction of hyperglycemia with insulin Correction of electrolyte disturbances, particularly potassium loss Correction of acid-base balance Treatment of concurrent infection, if present
Correction of Fluid Loss: Determine hydration status Determine hydration status: : Hypovolemic shock: Hypovolemic shock: Administer 0.9% saline, Ringer s lactate or a plasma Administer 0.9% saline, Ringer s lactate or a plasma expander as a bolus dose of 20 expander as a bolus dose of 20- -30 ml/kg. This can 30 ml/kg. This can be repeated if the state of shock persists. be repeated if the state of shock persists. Patient needs to be catheterized to measure the urine output to Patient needs to be catheterized to measure the urine output to forsee forsee Acute kidney injury. Acute kidney injury.
Correction of Fluid Loss: B B- - Dehydration without shock: Dehydration without shock: Initially correction is by isotonic saline, recommended schedule is: Administer 1-3 L during the first hour. Administer 1 L during the second hour. Administer 1 L during the following 2 hours Administer 1 L every 4 hours, depending on the degree of dehydration and central venous pressure readings BSL<180mg/dl . Switch to 5-10% dextrose with half isotonic saline.
Insulin Therapy: Short acting insulin i.e regular Insulin is the best choice. The initial insulin dose is a continuous IV insulin infusion using an infusion pump, if available, at a rate of 0.1 U/kg/h. A mix of 24 units of regular insulin in 60 mL of isotonic sodium chloride solution usually is infused at a rate of 15 mL/h (6 U/h) until the blood glucose level drops to less than 180 mg/dL; the rate of infusion then decreases to 5-7.5 mL/h (2-3 U/h) until the ketoacidotic state abates. The optimal rate of glucose decline is 100 mg/dL/h. If insulin pump is not available, IV insulin can be givenly hourly i.e Loading dose of 10U followed by 6U/hr, adjusted according to Bsl.
Electrolyte Correction: Potassium replacement: If K >6mEq/L no replacement If K 4.5-6mEq/L administer 10mEq/L If K 3-4.5mEq/L administer 20mEq/L Usually rule of thumb: 20mEq/L in alternate drip Correction of Acid base balance: IV sodium bicarbonate only in case of decompensated acidosis.
Metabolic Acidosis: Acidosis K correction If pH <7.0 If K<3.3mmol/l If K<3.3mmol/l start correcting K before start correcting K before correcting insulin correcting insulin If K > If K >3.3 3.3mmol/l mmol/l NaHCO3 NaHCO3 one ampoule per one ampoule per hour until pH>7.0 hour until pH>7.0 give IV short acting give IV short acting insuin 0.1 0.1U/kg/h U/kg/h insuin
Treatment of Concurrent Infection In the presence of infection, the administration of proper antibiotics is guided by the results of culture and sensitivity studies. Starting empiric antibiotics on suspicion of infection until culture results are available may be advisable.
Monitoring A flow chart must be used to monitor fluid A flow chart must be used to monitor fluid Balance, urine output & Lab measures. Balance, urine output & Lab measures. serum glucose must be measured hourly. serum glucose must be measured hourly. electrolytes also 2 electrolytes also 2- -3 hourly. 3 hourly. ABGs and urine ketones ABGs and urine ketones atleast atleast 4 hourly 4 hourly Ca, Mg, & phosphate must be measured initially & at least once Ca, Mg, & phosphate must be measured initially & at least once during therapy. during therapy. Neurological & mental state must examined frequently Neurological & mental state must examined frequently, , & any complaints of headache or deterioration of mental & any complaints of headache or deterioration of mental status should prompt rapid evaluation for possible cerebral edema. status should prompt rapid evaluation for possible cerebral edema.
When to shift to S/C Insulin When urinary ketones are negative (Atleast 2 consecutive sets) Anion gap closes Patient becomes conscious and starts tolerating orally Acidosis settles
Treatment complications: Cerebral edema Rare, but life threatening Usually in pediatric, adolescent patients Symptoms: Headache, altered mental status Treat with mannitol, hyperventilation Myocardial infarction, DVT/PE, cardiac dysrhythmias AKI (acute tubular necrosis, hypovolemia) Hypoglycemia, Hypokalemia Hypophosphatemia Occurs after aggressive hydration/treatment Monitor phosphorus and replete as needed to keep > 1
PREVENTION of DKA: Type 1 diabetes Type 1 diabetes Education around sick day management Continuation of insulin even when not eating Frequent monitoring when ill Type 2 diabetes Type 2 diabetes Education around sick day management Frequent monitoring when ill