Understanding Dyspepsia in Family Medicine Practice
Explore a family medicine seminar focusing on dyspepsia, including case studies, consultations, and patient interactions with a Saudi teacher experiencing upper gastrointestinal symptoms. Dr. Ali, a family physician, conducts a thorough bio-psycho-social analysis to identify potential causes and factors affecting the patient's health.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Family Medicine Seminar Dyspepsia
Lets GO Case Study Knowledge Approach If you Don t know it, you will Not see it
Case Study As a family physician
DR. ALI Family Physician
Family Medicine Consultation in family medicine practice To establish rapport with the patient To find out risk factors To find out possible cause
Hello Ahmed ! Hi Doc ! Prepare the setting Introduce yourself, call by name , smile , hand shaking Verbal / non-verbal Establish Rapport
Hello Ahmed ! Hi Doc ! Empathy Respect Confidentiality Eye contact Silence and understanding of the patient Show as possible
Mr. Ahmed 40 yrs old Saudi From Abha Father of 4 children Teacher
What's Wrong with you Ahmed ? I don t feel good doctor Presenting complaint What do you mean ?? Tell me more
pain Intermittent 6 months epigastric Retrosternal burning sensation Regurgitation Nausea
Let me ask you few questions Ahmed OK doctor Bio-Psych-Social Analysis
Bio-Psych-Social 6-month history of intermittent upper gastrointestinal symptoms. He describes an epigastric and retrosternal burning sensation but finds it difficult to decide in which of these areas symptoms are predominant. He occasionally notices regurgitation and feels nauseated. Eating, swallowing, postural change, or exercise do not influence her symptoms. Antacids provide some relief. Unremarkable past history and family history. Bio Psycho He feels unwell but the pain does not affect his life or his sleeping frequently Social He is smoker for >15 years , school teacher and a father of 4 children
Progressive weight loss Persistent vomiting IDA Epigastric mass Progressive dysphagia Acute GI bleeding
What do you think you have ? I don t think it is bad Idea/Concern/Expectation/Effect ICEE
OK Ahmed, May I examine you please Sure doctor
On Examination : Was vitally stable Obese: BMI= 32 No signs of anemia No jaundice Abdomen is soft and lax and not distended No abdominal mass No abdominal tenderness
Lets GO Case Study Knowledge Approach If you Don t know it, you will Not see it
Approach What Do you Think Ahmed Has ???
History: Complaint: Epigastric pain. Analysis of complaint: Onset. Duration. Nature, quality. Radiation. Course. Aggravating & relieving factors.
Risk factor and History Past medical Hx: Previous ulcer, GI bleed DM, hypo/hyperthyroidism, parathyroid dis. Colitis, diverticulosis, liver disease Previous Upper GI series, OGD, Abdo U/S Anxiety, stress, depression.
Risk factor and History Drug Hx: - iron, NSAIDs, bisphosphonates, antibiotics, etc. Life style Hx: Diet (fatty, big meals) Smoking Alcohol use Exercise Family Hx:
Bio-Psych-Social Analysis Psychosocial: Ideas - Ideas and beliefs of the patient towards his illness Concern - Patient might think that this complaint is due to cancer, ulcer or other serious disease, he might also feel concern that he could not work because of this problem. Expectations: Patient may expect any of the following: Reassurance Investigation, endoscopy - Barium meal Peferral Sick leave
Risk factor and History Effect on life: You need to explore the effect of this problem on his family, work, etc. Depression, anxiety and stress: Screen your patient for depression, anxiety and stress and go in details when needed. Supporting system: Sources of support at home, work, friends, community.
Physical Examination Vital signs: Weight Height. Blood Pressure. Pulse. Respiratory rate, Temperature . Signs anemia Brittle nails Cheilosis Pallor palpebral mucosa or nail beds Other Teeth (loss enamel) Lymphadenopathy - Virchow s node Acanthosis nigrans Hypo/Hyperthyroid Respiratory & Cardiovascular Examination.
Specific Examination Abdominal Examination: Epigastric tenderness Palpable mass Distention Colon tenderness Jaundice Murphy s sign Stool for OB Hernia
Lets GO Case Study Knowledge Approach If you Don t know it, you will Not see it
What is Dyspepsia? It is a group of symptoms characterized by upper abdominal discomfort, retrosternal pain, vomiting, heartburn, upper abdominal fullness and feeling full earlier than expected when eating.
Prevalence: Surveys carried out in western countries reported that: between 23-41%. Only 25% of dyspeptic populations visit their own doctors (About 4% of G.P.) Only 10% of the patients with dyspepsia are referred to hospital .
Differential Diagnosis: Functional Organic 50 70% 30 40%
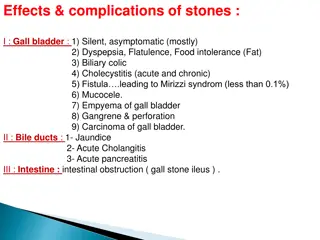
Medications (ASA/NSAIDS, Abx) Gastroparesis Cholelithiasis, Choledocholithiasis Peptic Ulcer 5- 21% Pancreatitis (acute or chronic) Gastric cancer 1- 3% Carbohydrate malabsorption Esophagitis 0-18% Ischemic bowel Other GI malignancy (ep. Pancreatic Organic cancer) Systemic disease (DM, Thyroid, Parathyroid, CTD) Intestinal parasite
Risk Factors: Obesity. Smoking. Anxiety, depression. Fatty meal. Junk food.
Functional Dyspepsia The most common cause overall. Defined as: at least 12 weeks (need not be consecutive) within the last 12 months of: Dyspepsia No evidence of organic disease Dyspepsia not exclusively relieved by defecation or associated with change in stool frequency or form (i.e. not IBS).
Pathophysiology The pathophysiology of dyspepsia is not well understood. Researchers have focused on several key factors: (Motility Disorders) vs .( Nonmotility Disorders). Psychosocial factors.
Abnormal Fundic Relaxation in Response to Meal in Functional Dyspepsia Normal Fundic accommodation or receptive relaxation Meal Impaired fundic accommodation with a redistribution of food to antrum Functional dyspepsia
Stress Behavioural Factors Local Factors: Gastritis H. pylori infection Abnormal Motility Decreased antral motility Impaired fundal relaxation
NONMOTILITY DISORDERS with motility disorders, there is little correlation between symptoms and severity of duodenitis, and no relationship between treatment and improvement of mucosal appearance on endoscopy. One of the most prevalent theories currently being evaluated is the possible involvement of H. pylori infection in non-ulcer dyspepsia (as in ulcer disease).
PSYCHOSOCIAL FACTORS Patients with nonulcer dyspepsia are more likely to have symptoms of anxiety and depression than are healthy persons or patients with ulcers. Multiple somatic complaints also are more common in patients who have nonulcer dyspepsia. A history of child abuse has been linked to the symptoms of nonulcer dyspepsia. Stress from life events also has been correlated with these symptoms and has been linked to exacerbations of nonulcer dyspepsia.
Specific investigations - Depend on expected cause: Usually we use the invasive procedure (endoscopy) to exclude the serious causes epically with patents have alarm symptoms: Alarm symptoms: Age > 45 Weight loss Bleeding Palpable mass Dysphagia
Specific investigations Peptic ulcer disease : Hx : Past history of ulcers, NSAIDs, Smoking. Dx: Endoscopy (0.99 specificity) Gastric ulcer or Duodenal ulcer : Dx : Endoscopy (0.98 specificity)
Specific Investigations: Gastroesophygeal reflux ( GERD): Hx : Heartburn or regurgitation symptoms, aggravated when supine, chronic cough Dx: Omeprazole Test (0.89 specificity) Endoscopy. 24 Hrs PH monitoring ,
Specific investigations Gastric Cancer: Hx .Older (>50),unexplained wt. loss, dysphagia, smoker Dx : Endoscopy Helicobacter pylori infection : - Urea breath test. - Stool antigen test. - Serum IGg antibody test. - Whole- blood antibody test .
Key Points Step One: Hx & Px attempt to establish a specific diagnosis Step Two: Consider Cancer urgent endoscopy if red flags Step Three: Treat for Non-Ulcer Dyspepsia Test & Eradicate H. pylori Acid suppression or Prokinetics x 1 month Step Four: Endoscopy Endoscopy if still symptomatic Step Five: Post-Endoscopy Management
MANGEMENT management
Management: Clarification; Explanation: Nature of the problem. What is ulcer & non-ulcer dyspepsia. Prognosis: Ulcer dyspepsia can be treated effectively. Non-ulcer remains recurrent since the cause is unclear.
Management: Reassure: Advice: Quit smoking Stop / reduce caffeine Stop / reduce EtOH Hold medications associated w/ dyspepsia NSAIDS, ASA Avoid foods and other factors precipitate symptoms Better eating habits.