Understanding Ischemic Heart Disease and Its Impact on Cardiovascular Health
Learn about the pathology, forms, outcomes, and epidemiology of ischemic heart disease, a leading cause of death in the industrial world. Explore the pathogenesis and common risk factors associated with this serious cardiovascular condition.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
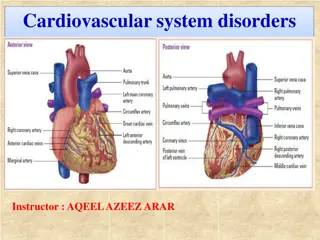
Cardiovascular pathology 2 Coronary heart disease
Plan Ischemic heart disease and its forms Myocardial infarction: clinical forms, complications and outcomes Sudden cardiac death Heart failure
Myocardium Special type of muscle tissue The biggest part of the heart The most common disorders are outcomes of ischemia Second common group of disorders is cardiomyopathy and inflammation
Ischemic Heart Disease The group of diseases where ischemia of myocardium is the common feature Imbalance of oxygen income and myocardial requirments can occur due to: - Increased need of myocardium because of increased workload tachycardia, cor hypertroficum - Decrease of oxygen in blood heart malformations, shock, anemia, CO poisoning - Atherosclerosis of coronary arteries is the most common
Ischemic Heart Disease The outcome of oxygen deprivation relies on lenghts of this condition: - Acute forms of ICHD sudden cardiac death and acute coronary syndrome with ST elevation in EKG (Q infarction) and without ST elevation in EKG (non-Q infarction and unstable angina pectoris) - Chronic forms of ICHD stabile angina pectoris, ICHS connected to postinfarction, to arrythmias and etc. - Special ICHD forms variant/vasospastic Prinzmetal angina pectoris
Epidemiology Leading cause of death in industrial world Risk factors are the same as for atherosclerosis Men have higher risk than women, but after menopausal age the gap is narrowing 30% decline in last 30 years
Pathogenesis The dominant cause is insufficient coronary perfusion relative to myocardial demand, due to chronic, progressive atherosclerotic narrowing of the epicardial coronary arteries, and variable degrees of superimposed acute plaque change, thrombosis, and vasospasm. The worst stenosis we obderve in first 2cm of RIA and RC
MYOCARDIAL INFARCTION (MI) MI, also known as heart attack, is the acuteischemic necrosis of cardiac muscle (coagulative character) due to prolonged severe ischemia. It is by far the most important form of ICHD. Acute coronary syndrome clinical presentation From 1970s decrease in mortality from 17% to 4% Before-hospital mortality is still 50%
MYOCARDIAL INFARCTION (MI). Etiopathogenesis The basis is rupture of aterosclerotic plaque of coronary artery with occurence of obturating thrombosis To necrosis it gets after 20 min Etiology may lay in embolism from endocardium vegetations, dissection of aorta, rarely coronary vasculitis. MI can be transmural and non-transmural
Transmural MI (Q infarction or STEMI) Should be at least 25mm, affect of wall Necrosis starts from endocardium to epicardium, from centrum to periphery of ischemic zone Process starts in 20 min and prolongues to 4-12 hours.
Non-transmural infarction (nonQ infarction or NSTEMI) Affects inner 1/3 up to half of wall Happens in appearance of collaterals or short time ischemia. Can happen without artery obturation in people with critical coronary artery stenosis during hemodynamic alterations
Pathology of MI MI can be microscopical (focally), small (min than 10%), middle (10- 30%) and big (more than 30%) When ramus intraventricularis is closed (40-50% of cases) anterior infarctions occur (peripheral part of RIA apical infarction) Ramus circumflexus (15-20% of cases) affects lateral and part of posterior part of LV lateral infarction Arteria coronaria dextra (30-40%) posterior or diaphragmatic infarction posterior part of LV, posterior part of septum and sometimes RV
Pathology of MI Micro changes appear after 2-4 hours In 4-8 hours we can observe edema of interstitium and later we see changes in cardiomyocytes (eosinophilic cytoplasm, nuclei become pale and disappear) In 24 hours at the periphery of focus we can see neutrophils 2-3 or 3-5 day dead cells start to decoy and nectoric tissue starts to be substituted with granulation tissue After 10-14 days up to 6 weeks granulation tissue is substituted with scar.
closure of arteria Clinical picture in 10-15 sec lactate accumulation 50% are numb ischemia dyspnoea, weakness or syncope Cardio enzymes - troponin T and I, MB fraction of creatinkinase (CK-MB), isoenzyme of lactate dehydrogenase (LD1), myoglobine. regional systolic and diastolic disorder (ECG changes in 30-120 sec) in 2-5 min chest pain In 5-20 min elevated cardioenzymes in 2-4 hours classical ECG changes
Classification of MI Type 1 spontaneus MI due to intramural thrombus Type 2 MI due to ischemic imbalance not due to ICHD(coronar spasm, hypotension) Type 3 cardia death due to MI Type 4 MI connected to revascularization by stent Type 5 - MI connected to revascularization by aortocoronar bypass
Complications of myocardial infarction Can be anatomical and functional Anatomical: -Pericarditis episternocardiaca (inflammation of pericardium above MI focus) -Aneurism of LV wall (acute and chronic, wall thrombi above MI focus) -Rupture of myocardium (leads to heart tamponade) -Rupture of papillary muscle (leads to acute mitral insufficiency) Functional: - Heart rhythms disorders (extrasystoles, fibrillation) - Hemodynamic disorders (hypotension and cardiac shock)
Angina pectoris is characterized by paroxysmal and usually recurrent attacks of substernal or precordial chest discomfort (variously described as constricting, squeezing, choking, or knifelike) caused by transient (15 seconds to 15 minutes) myocardial ischemia
Angina pectoris - stenocardia Can be stable and unstable Stable pain after stress or physical activity Unstable pain in calmness Variant Prinzmetal type of unstable angina pectoris, pain anytime Incomplete occlusion and role of vasoconstriction Thromboembolus to cause microinfarction
Chronic ICHD Mostly old patients with anamnesis of of angina pectoris, myofibrosis and closure of all branches of coronary arteries Patients are endangered with sudden cardiac death, arrytmia and heart failure
Sudden cardiac death Occurs typically due to malignant arrytmia, which usually manifests in chronic ICHD The most common form of cardiac death sudden death due to cardiac reasons which appears upto 1 hour from first signs or asymptomatically 2/3 of cases in myocardium we observe scar after MI. Most commonly men are affected.
Heart Failure Heart failure (congestive heart failure), is a common, usually progressive condition with a poor prognosis. The Frank-Starling mechanism - increased filling volumes dilate the heart and increase functional cross-bridge formation within the sarcomeres, enhancing contractility. Myocardial adaptations, including hypertrophy with or without cardiac chamber dilation. The collective molecular, cellular, and structural changes that occur as a response to injury or changes in loading conditions are called ventricular remodeling. This can culminate in impaired cardiac function. Activation of neurohumoral systems, especially (1) release of norepinephrine (increases heart rate and augments myocardial contractility and vascular resistance); (2) activation of the renin-angiotensin-aldosterone system; (3) release of atrial natriuretic peptide.
LEFT LEFT- -SIDED HEART FAILURE SIDED HEART FAILURE Left-sided heart failure is most often caused by (1) ischemic heart disease (2) hypertension (3) aortic and mitral valvular diseases (4) myocardial diseases The morphologic and clinical effects of left-sided CHF primarily result from congestion of the pulmonary circulation, stasis of blood in the left-sided chambers, and hypoperfusion of tissues leading to organ dysfunction.
RIGHT RIGHT- -SIDED HEART FAILURE SIDED HEART FAILURE Most commonly, right-sided heart failure is caused by left-sided heart failure, as any increase in pressure in the pulmonary circulation incidental to left-sided failure inevitably burdens the right side of the heart. Pure right-sided heart failure is infrequent and usually occurs in patients with any one of a variety of disorders affecting the lungs; it is referred to as cor pulmonale.