Understanding Oral Ulcerations: Causes, Types, and Treatments
Learn about oral ulcerations, including their causes such as infections, autoimmune conditions, trauma, and more. Explore the types of oral ulcerations like candidiasis and their manifestations. Discover the insights shared by Prof. Iftikhar Ahmad on oral health concerns.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
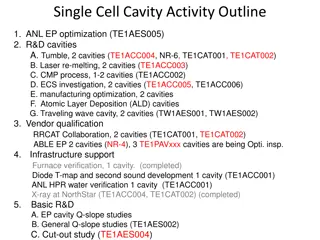
Oral Ulcerations PROF. IFTIKHAR AHMAD MBBS,MCPS,DLO,FVMA,FACHARZT,FRCS(UK) HOD ENT, PIMC/PIMS
INTRODUCTION: INTRODUCTION: - In Latin language ULCUS means break in the skin. - Oral ulceration is a break in the oral epithelium, exposing nerve endings in the underlying connective tissue. - It results in pain or soreness of the mouth especially with spicy food and citrus fruits.
Causes of Oral Ulceration Infection: Herpes, Vincent s infection, Candidiasis, T.B. Auto-immune: Aphthous ulcer, Behcet s syndrome Trauma: cheek bite, jagged tooth, ill-fitting denture chemical burn, thermal burn Inflammatory Skin & mouth disorder: Lichen planus, erythema multiforme Blood disorder: Leukemia, agranulocytosis, pancytopenia, sickle cell anemia Drug allergy: mouth wash, toothpaste Neoplasm: Leukoplakia, malignant Others: Radiation, chemotherapy, diabetes, uremia
ORAL CANDIDIASIS ( Moniliasis, Oral thrush or Oromycosis)
Etiology: Infection with Candida Albicans Predisposing factors: 1. Chronic ill-health 2. Uncontrolled diabetes mellitus 3. Acquired immune deficiency syndrome(AIDS) 4. Prolonged use of steroids 5. Prolonged antibiotic therapy 6. Immuno-suppressant therapy (cyclosporine) 7. Anti-cancer chemotherapy
Types of oral candidiasis Chronic hyperplastic: white plaques, cannot be removed by scraping ( Candidal Leukoplakia ) Pseudo-membranous: loosely adherent white lesions, can be scraped off leaving red patches Erythematous (atrophic): smooth, red patches Angular Cheilitis: white lesions on angle of mouth
Diagnosis 1. Microscopic exam of wet smear for Fungus. 2. Culture for fungus. Treatment 1. Clotrimazole paint, Nystatin mouthwash 2. Systemic Fluconazole: for chronic cases 3. Excision of hyperplastic plaque 4. Correction of underlying cause
Esophageal candidiasis Esophageal candidiasis is an opportunistic infection of the esophagus by Candida albicans. The disease usually occurs in patients in immmunocompromised states, including post-chemotherapy, diabetes and in AIDS.
Symptoms White lesion on the lining of esophagus that may look like cheese and may bleed if they are scraped. Pain or discomfort when swallowing. Dry mouth. Nausea. Vomoting. Weight loss. Chest pain.
Diagnosis Diagnosis of esophageal candidiasis is usually made during upper endoscopy. To confirm diagnosis, biopsies can be performed showing the presence of yeasts and pseudohyphae invading into mucosal cells. Culture reveal Candida, but are usually not necessary for diagnosis.
Complications Once the Candida fungus migrates past the gastrointestinal tract , it can become established in other major organs such as the lungs and kidneys. Left untreated, it can even cause death.
Treatment Candida esophagitis is treated with an oral anti-fungal drug fluconazole 200 to 400 mg per day for 14 to 21 days. For patient who may not be able to tolerate oral medication, the alternative is 400mg of fluconazole intravenously daily. In patients with fluconazole-refractory mucosal candidiasis, treatment options now include itraconazole solution, voriconazole, posaconazole, and the newer echinocandins (caspofungin, micafungin, and anidulafungin)
Introduction Recurrent, superficial ulcers, with necrotic centre + red margin, Involves movable mucosa of inner surface of lips, cheeks, tongue & soft palate No fever, malaise or lymph node enlargement
Etiology Deficiency: vitamin B complex, iron, folic acid, zinc Stress: emotional & physical Hormonal imbalance: changing progesterone level Autoimmunity: it may be an autoimmune process
Types 1. Minor aphthous ulcer: 2 10 mm in size, multiple, heal with no scar in 1 - 2 weeks 2. Major aphthous ulcer: 2 4 cm in size, usually single, heal with scar over months 3. Herpetiform aphthous ulcer: < 1 mm in size, multiple, heal with no scar in 1 week
Minor aphthous ulcer Aphthous ulceration
Major aphthous ulcer Rule out malignancy
1. Avoid Etiological factors 2. Supplement: vitamin B complex + folic acid + iron 3. Topical gel combination: a. steroid: triamcinolone b. antiseptic : chlorhexidine, benzalkonium, cetalkonium, tannic acid c. analgesic: benzydamine, choline salicylate d. anesthetic: lignocaine, benzocaine 4. Mouth rinse: betamethasone, tetracycline 5. Immuno-modulator: thalidomide 50 -100 mg daily