Understanding Statements of Reasons Process for MHRT Requests
Learn about the administrative process and requirements for Statements of Reasons (SOR) requests at MHRT. Understand who is entitled to receive SOR and the steps involved in writing and reviewing SOR. Get insights into the decision-making process and panel collaboration for preparing SOR effectively.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
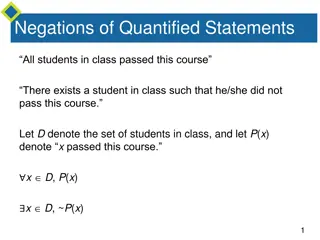
Presentation Transcript
Statements of Reasons Presenter: Virginia Ryan, Deputy President For MHRT Member training only. June, 2022
Topics The administrative process for SOR requests What must be included in an SOR Tips for how to go about writing an SOR Double checking your SOR Examples 2
SOR Requests Tribunal must, on request, give a person written reasons for the Tribunal s decision (s756). Persons entitled to receive reasons: people who are entitled to receive notice of the decision (s755) effectively, those persons entitled to receive notice. This will vary depending on the nature of the hearing e.g. patient, Administrator, Chief Psychiatrist/Director of Forensic Disability or Attorney-General. In some circumstances, the person who is entitled to receive SOR may have delegated their authority to make the request to another person. E.g. Administrator may have delegated to another person at the AMHS. 4
SOR Requests Attendance at hearing Attendance at a hearing is not linked to an entitlement to an SOR. A person who receives notice under s287 an NSP, personal guardian or attorney: no automatic right to attend the hearing. can request an SOR. A family member/carer/support person, may in some specific circumstances, receive a notice under s287: no automatic right to attend the hearing. can request an SOR if notice received. 5
Process MHRT prefers written requests for SORs, but not required by the Act. If the request is verbal, a file note will be made. On receipt of request, MHRT staff will check the requestor is entitled to an SOR. The Presiding Member, who is usually a Legal Member, will be asked to prepare the SOR. If not available, another panel member will be asked. Members receive the request via email to MHRT email account. Request will include: the written request where one is made documents that were before the panel the written request for SOR ROP, MD and decision confirmation of the date the SOR is due No need to claim payment for preparation of the SOR fee included in the next pay cycle. 6
Panels decision One member of the panel writes the SOR, but it represents the panel s decision - should be circulated to other panel members to review. Collaboration should be undertaken before the SOR is returned to the MHRT. Dissenting view: you may wish to liaise with that member about whether to address this in the SOR. You may wish to: only provide the reasons for the ultimate decision; or note that there was a dissenting view and how the decision was reached (e.g. majority s752(3)). If a panel member is not responsive or unavailable (e.g. on leave), it is not necessary to have their feedback before submitting the SOR. Please factor this into your timing when preparing an SOR. 7
Timing Requests will be processed as soon as possible to give members maximum time. The Tribunal must comply within 21 days of receipt of the request. When an SOR is received from a member, it is reviewed by a staff member to check for obvious errors and see if it generally meets the requirements of an SOR (we will come to that shortly). The SOR is delivered by email where possible, otherwise by post. The time to check and deliver the SOR should be taken into account; it is challenging when an SOR is received the afternoon of the day that it is due. The MHRT is required to monitor its compliance with the Act, including distribution of SORs in the required timeframe, and to report on this quarterly to the Office of the Chief Psychiatrist. 8
Confidential information Sometimes there will be information/documents that were not made available to the patient due to a CO or a VIS. Please prepare two versions of the SOR one which contains the confidential information and one which does not. For the patient version, you may wish to note that there was confidential information which was taken into account but that it will not be referred to in the SOR. Please label the file names accordingly and put a note on the top of the cover page of the document containing the confidential information Confidential Not to be disclosed to the patient . 9
Legal requirements Section 756 only specifies written reasons . Section 27B of the Acts Interpretation Act 1954: If an Act requires a tribunal, authority, body or person making a decision to give written reasons for the decision (whether the expression reasons , grounds or another expression is used), the instrument giving the reasons must also: (a) set out the findings on material questions of fact; and (b) refer to the evidence or other material on which those findings were based. So written reasons must include: relevant evidence, material findings of fact, reasons for the decision. 11
Findings on material questions of fact We will consider what this is by looking at what is meant by: 1. questions of fact 2. material 3. findings What are questions of fact? In law we distinguish between a question of fact and one of law. A question of fact: requires an interpretation of circumstances or context surrounding the specific matter, or issue. In criminal law, it is something a jury decides. Example: Does the patient have capacity? Contrast with a question of law: involves the interpretation of principles that are potentially applicable to other cases. Example: Which test of capacity the panel should be applying. 12
Material Essential, vital, key, influential in relation to the decision. Material: Whether the treatment criteria are met. Immaterial: Whether the patient is likeable. Not all information before the Tribunal is material. Requires consideration of what is relevant to your decision- making and what is not. Be selective because taking into account an irrelevant consideration (one which should not be considered) makes a decision unlawful. Can include: Patient s views, wishes and preferences. Legal representative submissions. Recommendations of experts (treating team, ARMC etc). 13
Findings of questions of fact A determination/conclusion made by a decision-maker as to a factual issue based on the evidence. Examples: That the patient does not have capacity. That there would be an unacceptable risk if the patient were permitted to live in the community. You will need to not only state your findings but will give reasons for why you made that finding, including by reference to the relevant evidence. 14
Reasons for the decision By specifying the material questions of fact, the Tribunal s findings/conclusions on those material questions of fact and the evidence used to make those findings you will essentially be giving your reasons. Some ways of thinking about what reasons are include: What did you have regard to, what did you conclude about that information and what did those conclusions mean for your decision? How would you justify your decision? How would you explain your decision-making to someone else? 15
Focus on why Example: where there is evidence of ongoing substance use the Tribunal may determine the risk arising from the patient living in the community is too high. But what is the link between the two? The treating team s evidence was that cannabis use causes a deterioration in the patient s mental state. This has been observed historically in this individual and is also consistent for people with the specific mental illness. Cannabis use impacts the person s ability to make good decisions, including ceasing prescribed medication mental state deteriorates increased risk of paranoid thoughts. Historically, paranoid thoughts have resulted in the person taking action in response to those thoughts which has on multiple occasions included violence against people in the community (e.g. neighbours). Therefore, the ongoing use of cannabis, increases the risk of medication non-compliance, mental state deterioration and in turn the risk of violence/aggressive behaviour to others. That risk is an unacceptable risk. 16
How to go about writing an SOR These are suggestions only. You may have your own way. Recommended you use the templates on the members website. Each template has an accompanying guide. Can also refer to the SOR Style Guide and deidentified examples. On receipt of a request: Review the materials that were before the Tribunal to refresh on the matter. Read the ROP and MD. 18
Language considerations Consider your audience. The same SOR is provided to all requestors for the same hearing most common to have only one request. Particularly for the individual keep language and concepts simple. Not all readers will be lawyers. The SOR may include content that is difficult for person to read cannot change that but something to be mindful of. Consider referring to the person by name rather than using the Patient . 19
Step by step 1. Identify relevant information Having regard to the earlier information on findings on material questions of fact, identify in the ROP, MD and written evidence the information you want to include. Consider highlighting that information. You can use different colours for different questions of fact (e.g. a different colour for each of the treatment criteria). 2. Complete the first page of the SOR template. This is formatted as a table. Delete the rows you don t need. 3. Complete the factual information in the body of the SOR template: signature block, clinical report paragraph, decision made. 20
Step by step cont. 4. Include information about the findings on material questions of fact (using the highlighting you did earlier) under the relevant headings in the SOR. Specify the evidence that the Tribunal relied upon to reach those findings. Set out the submissions made by representatives (e.g. patient s representative/legal representative and Attorney-General s representative), and your conclusions about those submissions. Prepare an introductory paragraph address any preliminary issues, previous adjournments, summary about the patient s circumstances at this point. Summarise the decision of the panel and the reasoning/conclusion of the panel. Review the SOR draft. 5. 6. 7. 8. 9. 21
Review the draft 1. Is it a clear summary of the material facts, relevant evidence, findings, decision? 2. Is it as easy to read as it could be: Can you be more succinct? Is there repetition? Can you do more to synthesise and summarise? 3. Are there typographical or formatting errors? All SORs are checked by the MHRT office before distribution but it is not intended that MHRT staff will provide administrative support in relation to SOR preparation. For assistance: refer to the document formatting tips information sheet. 22
Double checking your SOR Front page table: Delete the rows you aren t using (e.g. if you only have 3 members, delete the line for the 4th). Where you specify the decision, don t just copy paste: CONFIRMED does not need to be capitalised. Conditions as attached does not specify what conditions are attached to. Keep your dates consistent throughout 02/02/2022 or 2 February 2022. 24
Double checking your SOR Defined terms Define an acronym the first time you use it: Assessment and Risk Management Committee (ARMC) , with the acronym in bold this first time. Once defined, always use the defined term. If you are only referring to that phrase/name once, you don t need a defined term. Note: Mental Health Act 2016 is defined up near the top in the templates, you can simply say Act throughout. 25
Double checking your SOR Capitals: Defined terms. If you haven t defined it, consider if it needs a capital. The following are often capitalised but don t need to be: hearing, clinical report, treating team. Names of orders/authorities (e.g. treatment authority) don t need capitals. If you want to use capitals, be consistent throughout. Recommend you use Tribunal with a capital. Do a spell check. Check z hasn t replaced your s automatically. 26
Double checking your SOR Formatting (see Information Sheet Document formatting tips for guidance on how to do these): Single line spacing with no spaces above and below rows. All paragraphs with the same indent spacing. All paragraphs fully justified or left justified. Treat lists consistently: do you need a capital at the start of each item and do you punctuation at the end of each item? Can you combine some sentences to form a paragraph. We often see a lot of single sentence paragraphs. Don t need to double space between sentences. 27
Introductory paragraph Mr C was made subject to a forensic order (mental health) by the Mental Health Court on 28 May 2011. The events leading to the charges occurred in 2007. The charges were of the most serious nature and some constituted prescribed offences under the Mental Health Act 2016. The Tribunal revoked the forensic order on 3 September 2019 and made a treatment support order. The hearing was adjourned on 14 February 2022 in order that Mr C obtain an independent opinion. He had not been able to do so by the date of the adjourned hearing and wished to proceed. 29
Introductory paragraph This hearing represented the third periodic review of the treatment authority that was made on 13 June 2020. Mr F was a community patient at the time of the hearing, and he attended along with his case manager, Ms S, his treating psychiatrist, Dr G, and his registrar, Dr T. At the time of the hearing, it had been about eight months since Mr F had been discharged from hospital and moved to the Community Care Unit. Mr F told the Tribunal that he would like the treatment authority to be revoked. He said he would like to choose to not have any treatment and said that there would not be any risk to him if he was to have no treatment. By this, the Tribunal understood that he would like to stop having his anti-depressant medication. At the time of the hearing, it had been over six months since he had been prescribed anti-psychotic medication. Mr F also told the Tribunal he did not socialise with anyone but did go out with his support worker for grocery shopping. 30
Addressing preliminary issues Mr M received the clinical report on 29 July 2021. He received the report that is dated 29 July 2021. That is the report that the Tribunal had regard to. The treating team confirmed that a later signed report was not materially different to the one given to Mr M. On that basis, the Tribunal proceeded to review the treatment authority with reference to the version of the clinical report given to the Mr M, and without regard to the other later signed report. 31
Addressing preliminary issues The Tribunal were informed that Mr C could not attend the hearing because he was presently intubated in the Intensive Care Unit of the Brisbane Hospital. The treating team advised that it was unclear whether Mr C would become fit to attend the hearing within the next 28 days even if the Tribunal were minded to adjourn the hearing. Therefore, the Tribunal decided to proceed with the hearing in the absence of Mr C in accordance with section 747(2) given he was unfit to appear and it was appropriate and expedient to have the hearing in his absence. 32
Summarising evidence Mr G s psychiatric history is set out in detail in the clinical report. His first mental health concerns were identified when he presented to his general practitioner in 1999 with depression. After using illegal drugs in 2005, he had a one week admission with mania and was diagnosed with bipolar affective disorder. Mr G had a number of admissions between 2005 and 2010 with stability of mental state in between admissions. His admissions were often in the context of non-compliance with prescribed medication. His mental state was stable until April 2015 when he experienced a depressive phase, most likely triggered by family conflict. He responded well to anti-depressant medication and although prolonged, he did not require hospitalisation. Mr G has undertaken extensive psychoeducation and he is now able to identify his early warning signs and triggers. Over the past two years, Mr G has also been able to manage stressful life events and coped well. Since 2016, there have been no relapses, he has been compliant with all aspects of treatment and there are no concerns regarding substance use. 33
Particular points of note Mr K s lengthy admission was a matter of careful consideration by the Tribunal. The treating team appeared to be doing everything within its control to facilitate a safe and successful discharge to the community. Despite this, those attempts had been consistently unsuccessful. They had resulted in, or been foiled by, severe fluctuations in Mr K s mental state. The Tribunal was satisfied that in the absence of continued involuntary treatment, Mr K would likely decide to leave the hospital and experience a severe relapse of his mental illness due to a lack of adequate support for him in the community. 34
Relevant circumstances Mr A was diagnosed with depressive disorder with psychotic features and alcohol withdrawal syndrome at the time of the index offence. He was identified as having an acquired brain injury from 1970 in the report of Dr P to the MHC. He now has an additional diagnosis of mild dementia, of mixed aetiology, which emerged in 2017. His memory and volition are impaired, as is his capacity to make decisions about his health care and financial management. The Public Trustee has been appointed since 2018 for financial management. Mr A s children are the children of he and his deceased wife and are the stepchildren of his present wife. An application is underway to the Queensland Civil and Administrative Tribunal (QCAT) for his children to be appointed as financial decision-makers. Mr A s last depot medication was administered in 2016 and he has had no medication since then, with no recurrence of depressive mood or psychosis. He has returned to live with his wife and there have been no further incidents of aggression. His physical and mental states are declining in keeping with the dementia diagnosis. He has been co-operative with the treating team. He is supported by the non-government organisation, Local Community, and attends the local church. He has some phone contact with his two children residing in Malaysia. 35
Considering evidence The Tribunal notes that a CFOS report was provided in 2020. The Tribunal had particular regard to the following aspects of the risk assessment: [insert dot points]. The Tribunal considers these conclusions to be of relevance because they highlight concerns regarding Mr D s limited coping strategies and the impact of illicit substances on his risk profile. 36
Positive statements The Tribunal noted Ms P s psychiatric history, which very recently involved a relapse and admission to hospital for treatment. The Tribunal considered that Ms P was presently doing well and was gainfully employed. Ms P lives with her supportive adult son. _______ In any event, the Tribunal is satisfied that although Ms L s family are great supports to her, they would be unable to ensure that appropriate treatment and care is provided. The Tribunal agreed with Dr R s evidence that requiring a family member to enforce treatment which Ms L did not want would only put enormous pressure on the relationship. 37
Not accepting submissions The Tribunal carefully considered the evidence and the submissions of the legal representatives. While the factors noted by Ms Y are relevant, the Tribunal was unconvinced that they collectively meant that a forensic order was required to protect the safety of the community. Issues regarding Mr O s move to a residential aged care facility, loss of NDIS and possible future clozapine titration were thoroughly explored in evidence and as noted above, have not resulted in any mental state deterioration, or an increase in risk to the community. In fact, the change of accommodation has largely decreased Mr O s risk to the community given the strong evidence that he has completely settled into this accommodation and his medication compliance and monitoring is now assured. Ultimately, the Tribunal accepted the evidence and recommendations of Dr S and agreed that Mr O s risk to the community was significantly reduced since his move to residential aged care. The Tribunal noted that the major risks to the community were associated with the possibility that Mr O would suffer a relapse, which is possible should he become non- compliant with his medication. However, with his present living circumstances, extended period of passive compliance with treatment and ongoing monitoring by his nursing staff and the treating team, the Tribunal concluded that the risk to the community was low. 38
Evaluating evidence Ms S s evidence at hearing was consistent with her written application insofar as she advised that she did not suffer from a mental illness and that she had only suffered discrete episodes of drug induced psychosis, which had long since resolved. The Tribunal considered Ms S s views, however, determined that she presently suffers from a mental illness, the psychotic symptoms of which were under control via treatment. The Tribunal were persuaded by the fact that Ms S has had numerous admissions since 2018 on the basis of psychotic episodes which resolved through the use of anti-psychotic medications. She has relapsed in the absence of compliance with that antipsychotic medication. Further, Dr W, Dr R and Dr C have all diagnosed Ms S with schizophrenia. 39
Balancing factors Ultimately, the Tribunal acknowledged that Mr N has numerous positive factors which weigh in favour of a step down of his forensic order, such as [insert]. However, the Tribunal were persuaded that the evidence supports that Mr N s risk profile is still elevated particularly in light of illicit substance use. The Tribunal are mindful of the serious consequences that potentially follow from a relapse such as was seen in 2017 and in the index offences. The potential for relapse is inherent in continuing substance use, as noted in the above confidential evidence and the ARMC minutes. 40
Findings The risk of further malnutrition causing serious medical complications and death was a significant concern held by the Tribunal at the hearing. The Tribunal found that in the absence of involuntary treatment, Ms N was unlikely to remain compliant with medication. The medical evidence was that this would lead to a serious deterioration of her mental state which had, among other things, historically caused Ms N to restrict her oral intake. Therefore, the Tribunal was also satisfied that the absence of continued involuntary treatment would be likely to result in Ms N suffering serious physical deterioration, including death. 41
Findings The forensic order clearly remains necessary, because of Mr T s mental condition, to protect the safety of the community. The offence that led to the forensic order was serious. A long period of time has elapsed since that offending. However, there continues to be a risk of aggression and sexual violence towards others. Dr L provided a detailed independent risk assessment in 2019. He concluded then that Mr T remained a very high risk of reoffending. He thought there was a high risk of violence to others (noting the risk to staff, co-consumers and Mr T s mother). He also thought that the risk of future sexual violence was high. Dr A describes Mr T s continued poor impulse control and limited frustration tolerance, and some recent incidents of aggression and violence towards others. He also thought that the risk of future sexual violence was high. 42
Dont forget to explain reasoning regarding conditions The Tribunal considered the accommodation and treatment conditions were necessary to ensure the treating team knew where Mr X lived, that he was supervised, that he received treatment for his mental illness and to mitigate the risks of relapse and consequent harm to others. Given the deleterious effect of alcohol and illicit substances, the Tribunal considered those conditions were required to manage the risk of harm to others. Given the index offence involved a weapon and the severity of Mr X s illness and chronic psychotic disturbances, the Tribunal considered a prohibition on use of weapons condition was required to manage the risk of harm to others. 43
Conditions cont. The treating team said that whilst assessments to date had not indicated Mr X had paedophilic inclinations, specialised assessment by Dr B was required prior to recommending removing any conditions. Together with Mr X s reticence to discuss his sexual interests and the identified need for a more detailed psychosexual history, the Tribunal considered the conditions on the forensic order continue to be appropriate in order to manage risks there may be to children and to recognise the victim s concerns as disclosed in the victim impact statement. The Tribunal considered Dr A s evidence that Mr X consumed alcohol infrequently and in a controlled way and that there had been no incidents associated with alcohol use. The Tribunal did not consider a condition relating to alcohol was necessary at this time. 44
Human rights The Tribunal had regard to the Human Rights Act 2019 and considered that certain human rights under that Act were potentially engaged and limited by the decision of the Tribunal including Mr J s right to freedom of liberty and movement. The limitations are imposed for the important purpose of protecting the community. Forensic orders protect the community if persons diverted from the criminal justice system are at risk of harming others. Mr J was charged with a serious offence. He was diverted from the criminal justice system and there continues to be a risk to the safety of the community because of his mental condition. The limitations on his human rights are lawful and there is no less restrictive way of protecting the community. The limitations appropriately balance the restrictions on his human rights with the purpose of the limitations on his rights. 45
Human rights The Tribunal acknowledges the Human Rights Act 2019. Mr P received his clinical report within the statutory requirements and he attended the hearing. The Tribunal allocated adequate time to hear Mr P s review and considered his evidence. The Tribunal was satisfied Mr P was afforded a fair hearing. The human rights related to movement, disclosure of personal information and administering medical treatment in the absence of a person s free and full consent, amongst others, are potentially engaged and limited by the process and/or decision of the Tribunal. However, the Tribunal was satisfied that any limitations placed on Mr P s human rights are lawful, proportionate to his circumstances and compatible with the Human Rights Act. The Tribunal reached this decision because the human rights engaged have been balanced against the significant likelihood of Mr P s mental health deteriorating if he did not receive treatment and care under the treatment authority. 46
Human rights specific right s19. Freedom of Movement: The Tribunal accepts that Mr F s freedom of movement is currently limited by virtue of his placement on the Forensic Order. Such restrictions include requiring him to attend appointments at certain times, reside at an approved residence and not to travel without approval from the consultant psychiatrist. The Tribunal is satisfied that this limitation on Mr F s movement is lawful, proportionate to the circumstances and compatible with the Human Rights Act. The Tribunal reached this decision because, as demonstrated by the commission of the index offences, when he has been unwell historically, his behaviour has endangered the safety of the community. Because of the risk associated with Mr F s behaviour when unwell, the restriction on his human right to freedom of movement is balanced against the risk he may pose to other persons should he not receive treatment and care under the order. Therefore, the limitation on his freedom of movement is a limit necessary to ensure the safety of the community when he becomes unwell. 47