Understanding the Biomechanics of Nerves in the Peripheral Nervous System
Explore the intricate anatomy, physiology, and biomechanical behavior of nerves in the peripheral nervous system, crucial for sensory perception and motor function. Learn about nerve fibers, root compression, and more in this comprehensive guide presented by Dr. Santosh C. Metgud.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
BIOMECHANICS OF NERVES DR. SANTOSH C METGUD MPT, PhD, FIAP VICE PRINCIPAL DEPARTMENT OF ORTHOPEDIC MANUAL THERAPY
CONTENTS 1. Introduction 2. Anatomy and physiology of peripheral nerve 3. Anatomy and physiology of nerve root 4. Biomechanical behavior of peripheral nerve 5. Biomechanical behavior of nerve root 6. Multiple level nerve root compression
INTRODUCTION The nervous system serves as the body s control center and communication network. It can be divided into two parts: 1. Central nervous system 2. Peripheral nervous system Role of nervous system: 1. Sense change in the body and external environment 2. Interprets these changes 3. Respond to this interpretation by initiating actions such as muscle contraction or gland secretion.
Peripheral nervous system include 12 pairs of cranial nerves with their branches and 31 pairs of spinal nerves with their branches. Peripheral nerves are unique type of inert tissues, non-contractile in nature and necessary for the normal functioning of voluntary muscle. Each spinal nerve is connected to the spinal cord through a posterior (dorsal) root and Anterior (ventral) root at Intervertebral foramen. Posterior root contain fibers of sensory neuron and anterior root contain fibers from motor neurons. Shortly after spinal nerve leave intervertebral foramina, it divide into two main branches: Dorsal Rami and Ventral Rami
The nerves posses some special anatomic properties that may serve to protect the nerve from mechanical damage like tension (stretching) and compression.
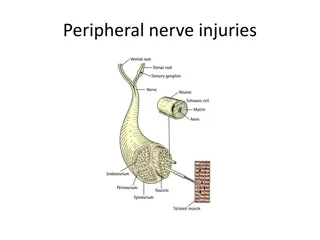
ANATOMY AND PHYSIOLOGY OF PERIPHERAL NERVE The peripheral nerves are the complex structures consisting of nerve fibers, connective tissue and blood vessels Because of these three tissue elements the nerve react to trauma in different ways and each play distinct role in functional deterioration of the nerve after injury.
A. NERVE FIBRES Nerve fibers not only transmit impulses but also serves as a anatomical connection between nerve cell body and end organs. The nerve fiber of sensory neuron conduct impulses from skin, skeletal muscles and joints to central nervous system. The nerve fibers of motor neurons convey impulses from the central nervous system to skeletal muscles, causing muscle contraction. This connection is maintained by axonal transport system which takes place at speeds that vary from 1 to 400 mm per day.
Axons are surrounded by multilayered, segmented covering known as myelin sheath which are produced by flattening cells called as Schwann cells. Unmyelinated gaps called nodes of Ranvier lie between segments of myelin sheath at approximately 1 to 2mm apart Myelin sheath increases the speed of conduction, insulate and maintain the axon. Impulse jump at higher speed from one node of Ranvier to next called as Saltatory conduction . The conduction velocity is directly proportional to diameter of the fibers
Nerve fibers are packed closely in fascicles, which are further arrange into bundles that make up the nerve itself.
B. CONNECTIVE TISSUE Successive layers of connective tissue surrounds the nerve fibers, namely endoneurium, perineurium and epineurium. These layers protect the continuity of nerve fibers.
1. Epineurium: Epineurium is a outermost layer located between fascicles and superficially in the nerve. Role of epineurium- a. Serves as a cushion during movements of the nerve, protecting the fascicles from external trauma b. Maintaining the oxygen supply system via the epineural blood vessels
2. Perineurium: Perineurium is a lamellar sheath that encompasses each fascicle. This sheath has great mechanical biomechanical barrier. Role of Perineurium: a. Chemically isolates the nerve fibers from their surroundings b. Preserve an ionic environment of the interior of the fascicles strength and specific
3. Endoneurium: The endoneurium the connective tissue inside the fascicles Composed principally of fibroblasts and collagen. It is a layer of delicate connective tissue around myelin sheath of each myelinated nerve fibers.
C.MICROVASCULAR SYSTEM Peripheral nerves are well vascularized structure, because both impulse propagation and axonal transport depend on local oxygen supply the microvascular system has large reserve capacity. Large vessels approaching nerve segmentally Divide into ascending and descending branches Run longitudinally and anastomose with vessels in perineurium and endoneurium
Within each fascicle lies longitudinally oriented capillary plexus with loop formation. These capillary plexus penetrate the perineurial membrane and run an oblique course through perineurium. Because of this peculiarity they are easily closed like valves when the tissue pressure in the fascicle increases. The built-in safety system of longitudinal anastomoses provides a wide margin of safety if an regional segmental vessels are transected.
ANATOMY AND PHYSIOLOGY OF SPINAL NERVE ROOT Two types of nerve roots are found in peripheral nerves, the ventral/motor roots and dorsal/ sensory roots. The motor or ventral nerve root leaves spinal cord from ventral aspect. The cell bodies of the motor axons are located in the anterior horns of the gray matter in the spinal cord. The other type of nerve root is the sensory or dorsal root. The cell bodies of the sensory axons are located in a swelling of the most caudal part of the respective dorsal nerve root, called the dorsal root ganglion. The dorsal root ganglia are located in or close to the intervertebral foramen.
Anatomy of spinal nerve roots There are two regions of nerve root 1. Central glial segment 2. Non glial segment Coverings of spinal nerve roots The axons in endoneurium are separated from cerebrospinal fluid by a thin layer of connective tissue called as root sheath. Root sheath covers the spinal cord, it has 2 to 5 cellular layers. The proximal part of root sheath is similar to pia cells and distal part are similar to arachnoid cells
The inner layer is a diffuse barrier, relatively weak and may prevent only passage of macromolecules. Spinal dura encloses the nerve root and CSF. When two layers of cranial dura enter the spinal canal, the outer layer blends with the periosteum of laminae of cervical vertebrae and inner layer join the arachnoid and become spinal dura. Spinal dura is an effective diffusion barrier.
MICROVASCULAR SYSTEM OF SPINAL NERVE ROOT A branch of segmental artery, intermediate branch joins the nerve root at the level of the dorsal root ganglion. There are usually three branches from this vessel: one to the ventral root, one to the dorsal root, and one to the vasa corona of the spinal cord. The vasculature of the nerve roots is formed by branches from the intermediate branch of the segmental artery distally and by branches from the vasa corona of the spinal cord proximally. This is known as intrinsic vascular system. To compensate for elongation of the nerve roots, the arteries are coiled longitudinally.
(1) extrinsic vascular system,(2) intrinsic vascular system. (2a) superficial intrinsic arterioles (3). From the superficial intrinsic arterioles are branches that continue almost at right angles down between the fascicles. These vessels often run in a spiraling course, thus forming vascular coils . (2b) When reaching a specific fascicle they branch in a T-like manner, with one branch running cranially and one caudally, forming interfascicular arterioles. (2c) From these interfascicular arterioles are small branches that enter the fascicles, where they supply the endoneurial capillary networks (4) spinal dura (5) root sheath.
BIOMECHANICAL BEHAVIOR OF PERIPHERAL NERVE External trauma to nerve may produce mechanical deformation of peripheral nerves. If mechanical trauma exceeds a certain degree the nerve s built-in mechanisms of protection may not be sufficient resulting in change in nerve structure and function. Common modes of nerve injury are stretching (rapid extension) and compression (crushing)
1. STRETCHING INJURY Nerves are strong structure with considerable tensile strength Elasticity and biomechanical properties of nerves is complicated by the fact that nerves are not homogenous isotropic materials but instead composite structure biomechanical properties. When tension is applied to nerve, initial elongation of nerve under small load followed by an interval in which stress and elongation show linear relationship characteristic of elastic material. with component having own
As limit of linear region is reached nerve start to disrupt inside endoneurium and intact perineurium. Perineurium sheath rupture at approximately 25% to 30% elongation and nerve start to behave like a plastic material. Maximum elongation is approximately at 25% and complete structural failure seems to occur at maximum elongation of 25% to 30%. Stretching injuries are associated with severe accidents, such as high energy tension with birth related injury, high speed vehicular collision or after a fall. The outcome of the injury depend upon which tissue components of nerve are damage and extent of injury.
2. COMPRESSION INJURY Compression at the nerve can induce symptoms such as numbness, pain and muscle weakness. Even mild compression was observed to induce structural and functional changes. At critical pressure level disturbances occur in intraneural blood flow, axonal transport and nerve function. Duration of the compression also influences the development of the changes. At 30mm Hg of local compression, upto 4 tp 6 hours will lead to functional changes such as change in axonal transport may occur and its viability may be jeopardized
TITLE Median nerve compression in the carpal tunnel-Functional response to experimentally induced controlled pressure AUTHOR Goran Lundborg, Richard H. Gelbennan, Martha Minteer-Convery METHOD Corresponding pressure levels were recorded close to the median nerve in the carpal tunnel in patients with carpal tunnel syndrome and in a group of control. RESULT Corresponding pressure levels (approximately 32 mm Hg) were recorded close to the median nerve in the carpal tunnel in patients with carpal tunnel syndrome, whereas in a group of control subjects the pressure in the carpal tunnel averaged only 2 mm Hg. Long-standing or intermittent compression at low pressure levels may induce intraneural edema, which in turn may become organized into a fibrotic scar in the nerve
Such block in axonal transport may cause axon to be more susceptible to additional compression distally, so called double crush syndrome. Slightly higher pressure (80 mm hg) causes complete cessation of intraneural blood flow, yet after two hours or more hours of compression, blood flow is rapidly restored when the pressure is released. With slightly higher pressure around 200-400 mm Hg for shorter period of time lead to incomplete recovery. Hence, the magnitude of the applied pressure and severity of induced compression lesion appear to be co-related.
The mode of pressure application is also important, Direct compression of nerve at 400 mm hg by means of small inflatable cuff around the nerve induces more severe injury than does the indirect compression of nerve at 1000 mm Hg. The nerve lesion is more severe probably because direct compression causes more pronounced deformation of nerve. two basic types of pressure applications are generally encountered in experimental settings and in pathologic conditions.
Radial compression: uniform pressure applied around the entire circumference of longitudinal segment of a nerve. This is the kind of purely radial pressure that is applied by the common pneumatic tourniquet. The cross-section of the nerve tends to remain circular but decreases in diameter in the loaded region. This radial compression requires a squeezing out of the tissue under the tourniquet, moving it outward from the centerline toward each of the free edges. This region sustains both the maximum pressure gradient and the maximum displacement.
Lateral compression: This is the kind of deformation that occurs if a nerve is placed between two parallel flat rigid surfaces that are then moved toward each other, squeezing the nerve or extremity. This type of deformation occurs if a sudden blow by a rigid object squeezes a nerve against the surface of an underlying bone. The cross-section changes from nearly circular to more elliptical The degree of compression can be measured by the maximum extension ratio (l), which is defined as the maximum diameter divided by the initial diameter of the nerve.
the nerve must be extended. This extension is illustrated by the movement of point G to G during compression. At the same time point A moves to A , indicating shortening or compression, in the direction of loading.
BIOMECHANICAL BEHAVIOR OF SPINAL NERVE ROOT The mechanical properties of human spinal nerve roots are different for any given nerve root at its location in the central spinal canal and in the lateral intervertebral foramina. The values for ultimate load are approximately five times higher for the foraminal segment of the spinal nerve roots than for the intrathecal portion of the same nerve roots under tensile loading. Roots seemed to be more susceptible to compression than did peripheral nerves.
A model was presented to evaluate effects of compression of the cauda equina nerve root in pigs, the cauda equina was compressed by an inflatable balloon that was fixed to the spine. The experiment was designed in a way that the pressure in the compression balloon was increased by 5 mm Hg every 20 seconds. The average occlusion pressure for the arterioles was found to be slightly below the systolic blood pressure and the blood flow in the capillary networks was dependent on the blood flow of the adjacent venules. This corroborates the assumption that venular stasis may induce capillary stasis and thus changes in the microcirculation of the nerve tissue
A compression-induced impairment of the vasculature may thus be one mechanism for nerve root dysfunction Compression may also induce an increase in the vascular permeability, leading to an Intraneural edema formation which increase the endoneurial fluid pressure, which may impair the capillary blood flow and jeopardize the nutrition of the nerve root Because the edema usually persists for some time after the removal of a compressive agent. Edema may negatively affect the nerve root for longer period than the compression itself.
50 to 75 mm Hg compression for two hours reduces muscle action potential amplitude and higher pressure 100 to 200 mm Hg may induce total conduction block. the sensory fibres are slightly more susceptible to compression than are the motor fibers. Also, the nerve roots are more susceptible to compression injury if the blood pressure is lowered pharmacologically.
Onset rate of compression- rapid-onset rate has been found to induce more pronounced effects on edema formation, methyl- glucose transport and impulse propagation than the slow-onset rate For the rapid-onset compression, which is likely to be more closely related to spine trauma or disc herniation than to spinal stenosis, a pressure of 600 mm Hg maintained for only 1 second is sufficient to induce a gradual impairment of nerve conduction.
MULTIPLE LEVEL NERVE ROOT COMPRESSION Patients with double or multiple levels of spinal stenosis seem to have more pronounced symptoms than do patients with stenosis only at one level. The mechanism for the difference between single and double compression may not simply be based on the fact that the nerve impulses have to pass more than one compression zone at double- level compression. There may also be a mechanism based on the local vascular anatomy of the nerve roots.
Unlike for peripheral nerves, there are no regional nutritive arteries from the surrounding structures to the intraneural vascular system in spinal nerve roots. Compression at two levels might therefore induce a nutritionally impaired region between the two compression sites.
TITLE Spinal nerve root compression. Nutrition and function of the porcine cauda equina compressed in vivo. AUTHOR METHODS Olmarker and Rydevik Experiment was done using two balloons at two adjacent disc levels. Which resulted in a 10- mm uncompressed nerve segment between the balloons. Induced a much more pronounced impairment of nerve impulse conduction. RESULT For instance a pressure of 10 mm Hg in two balloons induced a 60% reduction of nerve impulse amplitude during 2 hours of Compression, whereas 50 mm Hg in one balloon showed no reduction. The results showed that 64% reduction of total blood in the uncompressed nerve segment was induced when both balloons were inflated to 10 mm Hg. At a pressure close to the systemic blood pressure there was complete ischemia in the nerve segment. CONCLUSI ON Thus, experimental evidence shows that the blood supply to the nerve segment located between two compression sites in nerve roots is severely impaired although this nerve segment itself is uncompressed.
Regarding nerve conduction, the effects were much enhanced if the distance between the compression balloons was increased from one vertebral segment to two vertebral segments. This indicates that the functional impairment may be directly related to the distance between the two compression sites.
REFERENCES Nordin M, Frankel VH, editors. Basic biomechanics of the musculoskeletal system. Lippincott Williams & Wilkins; 2001. Magee DJ. Orthopedic physical assessment. Elsevier Health Sciences; 2014 Mar 25. Feinberg JG, Feinberg JH, Spielholz NI. Peripheral nerve injuries in the athlete. Human Kinetics; 2003. Lundborg G, Gelberman RH, Minteer-Convery M, Lee YF, HargensAR. Median nerve compression in the carpal tunnel functional response to experimentally induced controlled pressure. The Journal of hand surgery. 1982 May 1;7(3):252-9. Premakumari sathyavan. Essentials of neuroanatomy, 1stedition. Olmarker, K. (1991). Spinal nerve root compression. Nutrition and function of the porcine cauda equina compressed in vivo. Acta Orthop Scand Suppl, 242, 1 27.