Understanding Typhoid Fever: Causes, Symptoms, and Complications
Explore the world of typhoid fever caused by Salmonella Typhi, including its transmission, pathogenesis, virulence factors, and progression through different stages. Learn about the symptoms, complications, and treatment of this serious bacterial infection.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Bacterial food Bacterial food- -borne infections infections borne 28/10/1446 1
Enterica Food poisoning Cholera Brucellosis Diarrheal diseases 28/10/1446 2
Enteric Fevers (Enterica) Typhoid and Paratyphoid 28/10/1446 3
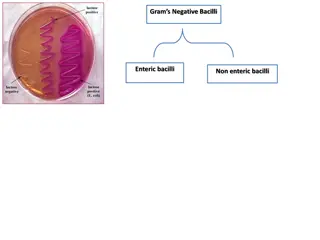
Causative agent: Salmonella Typhi Gram-negative facultative anaerobe Bacilli 28/10/1446 4
Modes of transmission: 1.Ingestion of food (vegetables , fish & shellfish)or water contaminated by a. Handling : feces or urine of cases and carriers (Food Handlers). b. Vector: flies-cockraoches c. Dust: food exposed to contaminated dust 2. Direct hand to mouth infection. 28/10/1446 5
Pathogenesis of typhoid The bacteria enter human digestive tract, penetrate intestinal mucosa and multiply in mesenteric lymph nodes, passes into blood Bacteriaemia usually within the first week. The Bacteriaemia is temporary and the organism finally lodging in the gall bladder. Organisms are shed into the intestine for some weeks.
Virulence factors Release of endotoxin and exotoxins. Salmonella strains may produce a thermolabile enterotoxin.
Classic untreated cases (1)Prodromal (invasion) stage: (1 week). -Fever (stepladder rise) &gradual onset sustained fever is usually higher in the evening. -Pulse: bradycardia (slow relative to fever). -Constitutional manifestation: malaise, headache, body aches, anorexia , sore throat and cough. -Rash appears on 6th day. 28/10/1446 8
(2)Advance stage: (2 weeks). -Continued high fever. -Worse physical and mental condition. -Abdominal distension with diarrhea or constipation. 28/10/1446 9
Complications (advance stage): 1-Ulceration of payers patches 2.Intestinal hemorrhage: 2nd or 3rd week. 3-Intestinal perforation: 3rd week. 4-Cholecystitis,meningitis osteomyelitis thrombophlebitis 4-Bronchitis and pneumonia. 5-Thrombophelibitis (femoral vein). 6-Myocarditis. 7-Osteomyelitis, bone abscess, spondylitis and non-suppurative arthritis. 8-Others: nephritis, meningitis, mental dullness, slight deafness and parotitis. 28/10/1446 10
(3)Decline stage or convalescence: (4th week) Uncomplicated cases gradually improves -Temperature decreases . -Abdominal manifestations disappear with satisfactory general condition. (4)Relapse : in 10% of untreated cases It occurs 1-2 weeks after return of temperature to normal. 28/10/1446 11
Management of chronic carriers: Ampicillin 1 gm every 6 hours for 1-3 months or quinolone is found to be effective. - If failed: surgical treatment of the pathological lesion (UB lesions in shistosomiasis, cholecystectomy). -Should not be released from supervision and restriction until 3 consecutive ve cultures 1month apart &at least 48 hrs after antimicrobial therapy has stopped - Patients are probably cured if relapse does not occur within 2 years. 28/10/1446 A 12
Laboratory diagnosis: 1st week : blood cultures. Positive blood culture is conclusive (ve +75%)but not exclusive 2nd& 3rd week : Widal test and stool & urine cultures. Bone marrow culture: the best bacteriologic confirmation (90-95%) even in patients received antibiotics. 28/10/1446 13
Differential diagnosis: Brucellosis. T.B. Malaria. 28/10/1446 14