Understanding Vascular Disorders and Hypertension
Explore the pathology of vessels, cardiovascular diseases, and the impact of vascular disorders on human health. Learn about the causes, types, and pathogenesis of hypertension, a prevalent medical condition affecting millions worldwide.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Pathology of vessels Cardiovascular pathology 4
Plan Arterial diseases - Systemic hypertension - Degenerative diseases - Aneurisms - Aorta dissection - Vasculitides Venous diseases - Varices - Vein thrombosis and thrombophlebitis Lymphatics diseases
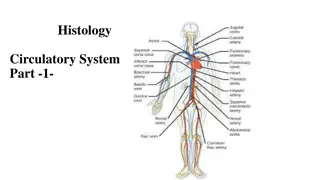
Vascular disorders Vascular disorders are responsible for more morbidity and mortality than any other category of human disease. two types of them arterial and venous diseases. two principal mechanisms: Narrowing (stenosis) or complete obstruction of vessel lumens Weakening of vessel walls, leading to dilation or rupture
Hypertension Increase of blood pressure can be systemic or local (lung or portal) Systemic hypertension is big medical problem a sustained diastolic pressure greater than 89 mm Hg, or a sustained systolic pressure in excess of 139 mm Hg. Both blood pressures are important in determining cardiovascular risk. 25% of individuals in the general population are hypertensive.
Etiology Etiology of primary hypertension is unknown Usually we use termin multifactorial reasons Risk factors are obesity, age, salt consumption, diabetes, smoking, physical inactivity and etc.
Types and Causes of Hypertension ESSENTIAL HYPERTENSION (90% TO 95% OF CASES) SECONDARY HYPERTENSION Renal (Acute glomerulonephritis, Chronic renal disease, Polycystic disease, Renal artery stenosis, Renal vasculitis, Renin-producing tumors) Cardiovascular (Coarctation of aorta, Polyarteritis nodosa, Increased intravascular volume, Increased cardiac output) Neurologic (Psychogenic, Increased intracranial pressure)
Pathogenesis of Secondary Hypertension Primary hyperaldosteronism is one of the most common causes of secondary hypertension renal artery stenosis causes decreased glomerular flow and pressure in the afferent arteriole of the glomerulus. induces renin secretion, initiating angiotensin II mediated vasoconstriction and increased peripheral resistance, increases sodium reabsorption and blood volume through the aldosterone mechanism.
VASCULAR PATHOLOGY IN HYPERTENSION Hyaline Arteriolosclerosis. homogeneous, pink hyaline thickening with luminal narrowing chronic hemodynamic stress Hyperplastic Arteriolosclerosis. severe (malignant) hypertension onion-skin lesions - concentric, laminated thickening of the walls and luminal narrowing plasma protein leakage across injured endothelial cells accompanied by fibrinoid deposits and vessel wall necrosis (necrotizing arteriolitis) increased smooth muscle cell matrix synthesis diffuse impairment of renal blood supply glomerular scarring
Arteriosclerosis hardening of the arteries - a generic term reflecting arterial wall thickening and loss of elasticity. three general patterns: Arteriolosclerosis M nckeberg medial sclerosis Atherosclerosis Atherosclerosis is characterized by intimal lesions called atheromas
Major Risk Factors for Atherosclerosis NONMODIFIABLE Increasing age Male gender Family history Genetic abnormalities MODIFIABLE Hyperlipidemia Hypertension Cigarette smoking Diabetes C-reactive protein
An atheromatous plaque consists of a raised lesion with a soft, yellow, core of lipid covered by a white fibrous cap.
Morphology Fatty Streaks Fatty streaks are the earliest lesions in atherosclerosis. yellow spots, composed of lipid-filled foamy macrophages. do not cause any flow disturbance. not all fatty streaks are destined to become advanced lesions.
Morphology Atherosclerotic Plaque. The key processes in atherosclerosis are intimal thickening and lipid accumulation. grossly appear white to yellow; superimposed thrombus over ulcerated plaques is red-brown. Plaques vary from 0.3 to 1.5 cm in diameter but can coalesce to form larger masses.
Complication Rupture, ulceration, or erosion of the intimal surface of atheromatous plaques Hemorrhage into a plaque. Rupture of the overlying fibrous cap, or of the thin-walled vessels in the areas of neovascularization, can cause intra-plaque hemorrhage; a contained hematoma may expand the plaque or induce plaque rupture. Atheroembolism. Plaque rupture can discharge atherosclerotic debris into the bloodstream, producing microemboli. Aneurysm formation. Atherosclerosis-induced pressure or ischemic atrophy of the underlying media, with loss of elastic tissue, causes weakness resulting in aneurysmal dilation and potential rupture.
Aneurysms and dissection Aneurysm is a localized abnormal dilation of a blood vessel or the heart it can be congenital or acquired Aneurysms can occur when the structure or function of the connective tissue within the vascular wall is compromised.
Etiology The two most important disorders that predispose to aortic aneurysms are atherosclerosis and hypertension; atherosclerosis is a greater factor in abdominal aortic aneurysms, while hypertension is the most common condition associated with aneurysms of the ascending aorta. Other conditions that weaken vessel walls and lead to aneurysms include trauma, vasculitis , congenital defects, and infections (mycotic aneurysms).
True and False Types of Aneurisms True aneurysm Wall of artery forms the aneurysm At least one vessel layer still intact Fusiform-Circumferential, relatively uniform in shape Saccular Pouchlike with narrow neck connecting bulge to one side of arterial wall
Types of aneursyms False aneurysm (also called pseudoaneurysm) Not an aneurysm Disruption of all layers of arterial wall Results in bleeding contained by surrounding structures
Clinical manifestations May mimic pain associated with abdominal or back disorders Pain correlates to the size May spontaneously embolize Causing blue toe syndrome patchy mottling of feet/toes with presence of palpable pedal pulses It can rupture causing shock and death in 5O% of rupture cases
Abdominal aneurysm Atherosclerotic plaque in the intima compresses the underlying media The media therefore undergoes degeneration and necrosis that results in arterial wall weakness and consequent thinning Abdominal aortic aneurysms occur more frequently in men and in smokers, and rarely develop before age 50
Thoracic aneurysm Thoracic aortic aneurysms are most commonly associated with hypertension, but other causes such as Marfan and Loeys Dietz syndromes are increasingly recognized. May have substernal, neck, back pain Swelling (edema) in the neck or arms Myocardial infarction
Complications Rupture Anterior rupture Massive hemorrhage Most do not survive long enough to get to the hospital Posterior rupture Bleeding may be tamponaded by surrounding structures, thus preventing exsanguination and death Severe pain May/may not have back/flank ecchymosis
Aortic dissection Aortic dissection occurs when blood splays apart the laminar planes of the media to form a blood-filled channel within the aortic wall; Aortic dissection occurs in two groups: men aged 40 to 60, with antecedent hypertension (more than 90% of cases of dissection); younger patients with systemic or localized abnormalities of connective tissue affecting the aorta (Marfan syndrome). Dissections can also be iatrogenic. Rarely, for unknown reasons, dissection of the aorta or other branches, including the coronary arteries, occurs during or after pregnancy. Clinical features - the sudden onset of excruciating pain, may mimic myocardial infarction
Vasculitis Vasculitis is a general term for vessel wall inflammation It depends a lot of what type of vessels are affected Clinical mafestations typically include constitutional signs and symptoms such as fever, myalgias, arthralgias, and malaise Vasculitis can be divided into three big groups Small vessels vasculitis Medium vessel vasculitis Large vessel vasculitis
Vasculitis Type Examples Description LARGE-VESSEL VASCULITIS Aorta and large branches to extremities, head, and neck Giant-cell (temporal) arteritis Granulomatous inflammation; involves the temporal artery. Usually occurs in patients older than age 50 and is associated with polymyalgia rheumatica. Granulomatous inflammation usually occurring in patients younger than age 50 Takayasu arteritis MEDIUM-VESSEL VASCULITIS Main visceral arteries and their branches Polyarteritis nodosa Necrotizing inflammation typically involving renal arteries but sparing pulmonary vessels Kawasaki disease Arteritis with mucocutaneous lymph node syndrome; usually occurs in children. Coronary arteries can be involved with aneurysm formation and/or thrombosis. SMALL-VESSEL VASCULITIS Arterioles, venules, capillaries, and occasionally small arteries Wegener granulomatosis Granulomatous inflammation involving the respiratory tract and necrotizing vasculitis affecting small vessels, including glomerular vessels. Associated with PR3-ANCAs. Eosinophil-rich granulomatous inflammation involving the respiratory tract and necrotizing vasculitis affecting small vessels. Associated with asthma and blood eosinophilia. Associated with MPO-ANCAs. Churg-Strauss syndrome Necrotizing small-vessel vasculitis with few or no immune deposits; necrotizing arteritis of small and medium-sized arteries can occur. Necrotizing glomerulonephritis and pulmonary capillaritis are common. Associated with MPO- ANCAs Microscopic polyangiitis
Giant-cell temporal arteriitis the most common form of vasculitis among elderly individuals. It is a chronic, granulomatous inflammation of large to small-sized arteries that affects principally the arteries in the head, but also the vertebral and ophthalmic arteries Symptoms fever, fatigue, weight loss also include facial pain or headache Ophthalmic arterial involvement can lead to permanent blindness; medical emergency Lesions also occur in other arteries, including the aorta (giant-cell aortitis) Etiology and pathogenesis are unknown
Takayasu arteriitis granulomatous vasculitis of medium and larger arteries characterized principally by ocular disturbances and marked weakening of the pulses in the upper extremities (pulseless disease). transmural fibrous thickening of the aorta the aortic arch and great vessels and severe luminal narrowing of the major branch vessels Those over 50 years of age are designated as having giant-cell aortitis, while those under 50 have Takayasu aortitis.
Polyarteritis nodosa a systemic vasculitis of small or medium-sized muscular arteries, typically involving renal and visceral vessels but sparing the pulmonary circulation. There is no association with ANCAs the cause remains unknown in the majority of cases
Kawasaki disease The leading cause of acquired heart disease in children is an acute febrile, usually self-limited illness of infancy and childhood (80% are younger than 4 years) associated with an arteritis affecting large to medium-sized, and even small, vessels. a predilection for coronary artery involvement; such coronary arteritis can cause aneurysms that rupture or thrombose, resulting in acute myocardial infarctions IN CHILDREN. The etiology is unknown
Microscopic polyangitis Necrotizing vasculitis that generally affects capillaries Hypersensitivity vasculitis or leukocytoclastic vasculitis. necrotizing glomerulonephritis (90% of patients) and pulmonary capillaritis are particularly common an antibody response to antigens such as drugs, microorganisms, heterologous proteins, or tumor proteins has been implicated; can either result in immune complex deposition or may trigger secondary immune responses (development of p-ANCAs).
CHURG-STRAUSS SYNDROME Churg-Strauss syndrome (also called allergic granulomatosis andangiitis) is a relatively rare small-vessel necrotizing vasculitis classically associated with asthma, allergic rhinitis, lung infiltrates, peripheral hypereosinophilia, and extravascular necrotizing granulomas. ANCAs are present Cutaneous involvement (palpable purpura), gastrointestinal tract bleeding, and renal disease (primarily as focal and segmental glomerulosclerosis) Myocardial infiltrates of eosinophils are implicated in the Churg-Strauss cardiomyopathy the heart is involved in 60% of patients, and accounts for almost half of the deaths in the syndrome. The etiology remains obscure
WEGENER GRANULOMATOSIS Granulomatosis with polyangitis a necrotizing vasculitis characterized by Acute necrotizing granulomas of the upper respiratory tract (ear, nose, sinuses, throat) or the lower respiratory tract (lung) or both Necrotizing or granulomatous vasculitis affecting small to medium-sized vessels, most prominent in the lungs and upper airways Renal disease in the form of focal necrotizing, often crescentic, glomerulonephritis PR3-ANCAs are present in up to 95% of cases;
THROMBOANGIITIS OBLITERANS (BUERGER DISEASE