Understanding Vascular Flow Disorders and Hemodynamic Abnormalities
Explore the complexities of vascular flow disorders, thrombosis, embolism, and hemodynamic abnormalities affecting local and general circulation. Learn about the etiology, signs, and outcomes of these critical conditions, including thrombus formation, arterial and venous thrombi, and the fate of thrombi in different cardiac chambers. Gain insights into the impact of embolism on various body tissues and systems. Enhance your understanding of the mechanisms underlying these disorders for better diagnosis and management.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
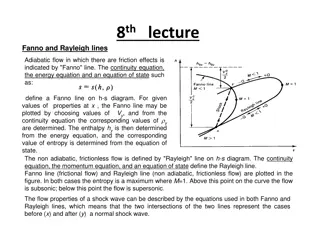
Disorders of vascular flow General disorders
Plan Local hemodynamic disorders - Thrombosis - General hemodynamic disorders Embolia - Etiology and signs - Right heart failure - Disorders of tissue perfusion Left heart failure - Hyperemia - Hemorrhagia - Ischemia - Disorders of liquids homeostasis Infarction - Edema - Shock Dehydratation
Local hemodynamic disorders. Thrombosis intravital intravascular blood clotting 1. endothelial injury physical hypertension, turbulence chemical hypercholesterolemia, smoking, vasculitis Virchow triad 2. alteration of blood flow stasis immobilization, cardiac chamber dilation 3. hypercoagulability primary (genetic) x secondary factor V mutation (Leiden) x neoplasms, drugs
Thrombosis 1. Arterial thrombi occlusive coronary + cerebral + femoral arterias AS plaque + bifurcation Grossly: gray-white, friable Micro: PLT + fibrin, RBC + WBC
Thrombosis 2. Venous thrombi (phlebothrombosis) occlusive deep veins of LL + pelvic plexus Grossly: firm, red, attached to wall Micro: RBC + fibrin asymptomatic (50%) !!! X postmortal clots (not attached to wall, gelatinous red centre + fat supernatant)
Thrombosis 3. Cardiac chambers, atrial auricles upon infarction + dilated cardiomyopathy mural 4. Valve cusps infective endocarditis (vegetations) non-bacterial thrombotic endocarditis (sterile) Libman-Sacks endocarditis systemic lupus
Thrombosis fate of thrombus 1. propagation 2. embolization 3. dissolution fibrinolysis (recent thrombi) 4. organization endothelial cells, smooth muscle cells, fibroblasts, capillaries 5. recanalization new small lumina
Embolism detached i.v. solid, liguid or gaseous mass carried by blood to distant site from point of origin 1. thrombembolism (99%) pulmonary x systemic infarction 2. cellular - amniotic fluid, tumor cells 3. subcellular - AS debries, BM bits 4. fat 5. air 6. foreign bodies paradoxical retrograde
Pulmonary thrombembolism source - deep veins of lower extremities + pelvic plexus v. cava inf. right heart a. pulmonalis paradoxical embolism systemic emboli + left heart failure pulmonary infarction large - sudden death (acute right heart failure) bifurcation saddle embolus 60% pulmonary circulation obstructed small (60-80%) - pulmonary hypertension branching arterioles fibrinolysis bridging web
Systemic thrombembolism source: intracardial thrombi (80%) aortic AS plaques infarctions Lower extremities (75%) + brain (10%) bowel + kidney + spleen
Fat embolism source: fractures of bones with fatty BM + soft tissue trauma + burns 1. stage (after 1-3 days) veins lungs respiratory insufficiency 2. stage lungs systemic circulation neurologic symtoms + thrombocytopenia 10% fatal Mi: fat droplets in lung, brain, kidney capillaries
Air embolism 1. systemic veins lungs obstetric procedures, goiter operation, chest wall injury 2. pulmonary veins systemic circulation cardiosurgery 100mL of air symptoms (dyspnea) air bubbles physical vessel obstruction Decompression sickness deep sea divers (nitrogen) chronic form caisson disease bone necrosis
Amniotic fluid embolism source: abruptio placentae retroplacental hematoma a.f. infusion into maternal circulation uterine veins lungs dyspnea, cyanosis, hypotensive shock, seizures, coma + lung edema + DIC Micro: pulmonary capillaries (mother) - squamous cells + lanugo hair + fat
Stasis significant slowing or stopping flow of blood in vessels in an organ or tissue. Causes of stasis: Ischemia and venous congestion.
General hemodynamic disorders Causes of hemodynamic insufficiency: - Diseases of heart (myocard, endocard, pericardial bag, disorders of rhytm, congenital heart disorders, infections and etc .) - Diseases of vessels (systemic and lung hypertension and etc ) - Diseases of blood (diorders of volume, coagulation and etc )
Hemodynamic insufficiency in heart Acute start = acute heart insufficiency dilatation of heart compartments Chronic changes = adaptation of heart muscle hypertrophy We distinguish hypertrophy into concentric and excentric
Signs of hemodynamic insufficiency We can distinguish right and left hear failure right hear failure: mostly manifests as venostatis in organs (liver, spleen, brain and kidneys) left hear failure: involvement of lungs Heart insufficiency leads to disorders of tissue perfusion
Disorders of tissue perfusion Hyperemia and Congestion Hemorrhage Ischemia / Infarction
Hyperemia and Congestion = increased blood volume in particular tissue hyperemia active (arteriolar dilation) red color striated muscle exercise congestion passive (impaired venous return) systemic x local blue-red color (cyanosis), edema event. hypoxemic necrosis (bowel) accumulation of deoxygenated Hb chronic chronic hypoxia regressive changes + small hemorrhages siderophages
HYPEREMIA Congestion: a passive process resulting from impaired venous return out of a tissue It may occur: systemically, as in cardiac failure locally, resulting from an isolated venous obstruction The tissue has a blue-red color (cyanosis): as worsening congestion accumulation of deoxygenated hemoglobin in the affected tissues Chronic passive congestion: Is a long-standing congestion The stasis of poorly oxygenated blood causes: Chronic hypoxia degeneration or death of parenchymal cells subsequent tissue fibrosis Capillary rupture small foci of hemorrhage phagocytosis and catabolism of the erythrocyte debris accumulations of hemosiderin-laden macrophages
HYPEREMIA acute pulmonary congestion chronic pulmonary congestion acute hepatic congestion chronic passive congestion of the liver
HYPEREMIA Lung acute pulmonary congestion: alveolar capillaries engorged with blood may also be associated with alveolar septal edema and/or focal minute intra- alveolar hemorrhage chronic pulmonary congestion: the septa become thickened and fibrotic the alveolar spaces may contain numerous hemosiderin-laden macrophages ("heart failure cells")
HYPEREMIA Liver acute hepatic congestion: the central vein and sinusoids are distended with blood there may even be central hepatocyte degeneration the periportal hepatocytes, better oxygenated because of their proximity to hepatic arterioles, undergo less severe hypoxia and may develop only fatty change chronic passive congestion of the liver: the central regions of the hepatic lobules are grossly red-brown and slightly depressed (because of a loss of cells) and are accentuated against the surrounding zones of uncongested tan, sometimes fatty, liver ("nutmeg liver ) microscopically, there is centrilobular necrosis with hepatocyte drop- out hemorrhage, and hemosiderin-laden macrophages In long-standing, severe hepatic congestion (most commonly associated with heart failure), hepatic fibrosis ("cardiac cirrhosis") can develop
Kidney congestion Kidney: dystrophy of canaliculi epithelium Spleen: atrophy of follicles
Hemorrhage extravasation of blood from blood vessels external (+ in hollow organs) internal: within tissue hematoma hemorrhagic diatheses insignificant injury vasculopathies trombocytopenia + -patia coagulopathy
Hemorrhage 1. Petechiae (1-2 mm) - skin + mucosa intravascular pressure, platelets 2. Purpuras (3-5 mm) trauma, vasculitis, vascular fragility 3. Ecchymosis (1-2 cm) = hematoma (bruise) RBC phagocytosis by macrophages Hb (red-blue) bilirubin (blue-green) hemosiderin (golden-brown) 4. Cavities hemothorax, hemopericardium, hemoperitoneum hemarthros
Hemorrhage arterial + venous + capillary H. per rhexin injury - brain H. per diabrosin erosion peptic ulcer H. per diapedesin transmigration of RBC (no damage of capillaries) toxic injury + stasis
Hemorrhage - outcome 1. loss volume > 20% hemorrhagic shock 2. loss rate acute hemorrhagic shock chronic (peptic ulcer, metrorhagia, colonic adenoCa) iron deficiency anemia
Ischemia / Infarction = ischemic necrosis due to occlusion of arterial supply (or venous drainage?) causes: thrombotic or embolic events (99%) vasospasm, hemorrhage in AS plaque external compression (tumor) twisting (testicular + ovarian torsion, bowel volvulus)
Infarction - determinants 1. nature of blood supply dual lung + liver end-arterial kidney + spleen 2. rate of occlusion acute infarction chronic collateral circulation, interart. anastomoses 3. vulnerability to hypoxia neurons 3-4 min cardiomyocytes - 20-30 min fibroblasts - hours 4. oxygen blood content heart failure, anemia
Infarction - morphology 1. red infarcts venous occlusion loose tissue (lung) blood collection dual circulation lung + bowel previously congested organs reperfusion (angioplasty, drug-induced thrombolysis) 2. white infarcts arterial occlusion solid organs heart (yellow), spleen, kidney wedge shape apex to occluded artery base to organ periphery + fibrinous exudate (pleuritis, pericarditis epistenocardiaca)
Infarction - morphology ischemic coagulative necrosis 3 zones 1. total necrosis - centre loss of nuclei, eosinophilia of cytoplasm, architecture is preserved 2. partial necrosis some cells survive inflammation (neutrophils) 1-2 day degradation of dead tissue 3. hyperemic rim
Infarction - morphology healing granulation tissue (5-7 day) fibrous scar (6-8 weeks) brain liquefactive necrosis pseudocyst !
Infarction septic infarctions source infective endocarditis (vegetations) suppurative thrombophlebitis infarction abscess granulation tissue scar
Myocardial infarction Myocardial infarction - (atherosclerosis, thromboembolism, vascular spasm) occurs because of coronary artery obstruction in case of insufficient function of collaterals, as well as non-compliance increased functional load level of blood supply of organ. Grossly myocardial infarction has an irregular shape, and refers to type of white infarction with hemorrhagic rim. Localization release: transmural, intramural, subendocardial and subepicardial.
Infarction of brain necrosis of nervous tissue develops as a result of persistent cessation of blood flow to this area. Causes of infarct are atherosclerosis, arterial spasm or obstruction of vessel with thrombus, embolus. In gross examination by method of forming cerebral infarction are divided into white (anemic) and red (hemorrhagic) stroke.
Lung infarction In lungs infarcts of hemorrhagic type develops usually. The main factors contributing to emergence of hemorrhagic infarction is dual blood supply of lungs and venous stasis.
Kidney infarction Frequently observed in the renal artery thromboembolia. It refers to renal ischemic infarct with hemorrhagic rim, it has a conical shape with a base facing to kidney capsule, and with an edge to renal pelvis.
Spleen infarction Most often it can be seen in septic endocarditis, hypertension, leukemia. Spleen infarct ussualy has ischemic type (white), it has a conical shape with a base facing to capsule.