Understanding Viral Infections and Their Impact on the Body
Explore the diverse range of viral infections affecting different organ systems in the body, including respiratory, digestive, skin, and central nervous system viruses. Learn about acute transient infections and the pathogenesis of measles virus, a leading cause of vaccine-preventable illness globally.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Organ System Species Disease Respiratory Adenovirus Rhinovirus Influenza viruses A, B Respiratory syncytial virus Upper and lower respiratory tract infections, conjunctivitis, diarrhea Upper respiratory tract infection Influenza Bronchiolitis, pneumonia Digestive Mumps virus Rotavirus Norovirus Hepatitis A virus Hepatitis B virus Hepatitis D virus Hepatitis C virus Hepatitis E virus Mumps, pancreatitis, orchitis Childhood gastroenteritis Gastroenteritis Acute viral hepatitis Acute or chronic hepatitis With HBV, acute or chronic hepatitis Acute or chronic hepatitis Enterically transmitted hepatitis Systemic with Skin Eruptions Measles virus Rubella virus Varicella-zoster virus Herpes simplex virus 1 Herpes simplex virus 2 Measles (rubeola) German measles (rubella) Chickenpox, shingles Oral herpes ( cold sore ) Genital herpes Systemic with Hematopoietic Disorders Cytomegalovirus Epstein-Barr virus HIV-1 and HIV-2 Cytomegalic inclusion disease Infectious mononucleosis AIDS Arboviral and Hemorrhagic Fevers Dengue virus 1 4 Yellow fever virus Dengue hemorrhagic fever Yellow fever Skin/Genital Warts Papillomavirus Condyloma; cervical carcinoma Central Nervous System Poliovirus JC virus Poliomyelitis Progressive multifocal leukoencephalopathy (opportunistic)
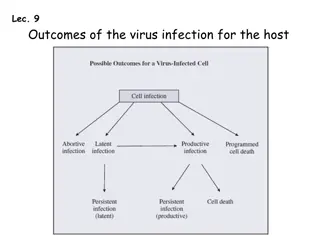
ACUTE (TRANSIENT) INFECTIONS The viruses that cause transient infections are structurally heterogeneous, but each elicits an effective immune response that eliminates the organism and may or may not confer lifelong protection. The immune response to some transient viruses wanes with time, allowing even the same serotype of virus to infect repeatedly (respiratory syncytial virus)
Measles Measles (rubeola) virus is a leading cause of vaccine-preventable death and illness worldwide. More than 20 million people are affected by measles each year. Epidemics of measles occur among unvaccinated individuals. Measles can produce severe disease in people with defects in cellular immunity. The diagnosis is usually made clinically, or by serology or detection of viral antigen in nasal exudate or urinary sediment
Pathogenesis Measles virus is a single-stranded RNA virus of the paramyxovirus family that includes mumps, respiratory syncytial virus, parainfluenza virus, and human metapneumovirus. There is only one serotype of measles virus. Measles virus is transmitted by respiratory droplets. The virus initially multiplies within upper respiratory epithelial cells and then spreads to local lymphoid tissue. Replication of the virus in lymphatic tissue is followed by viremia and systemic dissemination of the virus to many tissues. Measles may cause croup, pneumonia, diarrhea with protein-losing enteropathy, keratitis with scarring and blindness, encephalitis, and hemorrhagic rashes ( black measles ) in malnourished children with poor medical care.
Morphology The blotchy, reddish brown rash of measles virus infection on the face, trunk, and proximal extremities is produced by dilated skin vessels, edema, and a moderate, mononuclear perivascular infiltrate. Ulcerated mucosal lesions in the oral cavity - the pathognomonic Koplik spots. The lymphoid organs typically have marked follicular hyperplasia, large germinal centers.
Mumps Mumps virus is a member of the paramyxovirus family. Highly contagious Mumps virus has two types of surface glycoproteins, one with hemagglutinin and neuraminidase activities and the other with cell fusion and cytolytic activities. Mumps viruses enter the upper respiratory tract through inhalation of respiratory droplets, spread to draining lymph nodes where they replicate in lymphocytes, and then spread through the blood to the salivary and other glands. Mumps virus infects salivary gland ductal epithelial cells, resulting in desquamation of involved cells, edema, and inflammation that leads to the classic salivary gland pain and swelling of mumps. Mumps virus also can spread to other sites, including the CNS, testis and ovary, and pancreas.
Morphology In mumps parotitis (bilateral in 70%) affected glands are enlarged, have a doughy consistency, and are moist, glistening, and reddish brown on cross-section. On microscopic examination the gland interstitium is edematous and diffusely infiltrated by imflammation cells, which compress acini and ducts. Because the testis is tightly contained within the tunica albuginea, parenchymal swelling may compromise the blood supply and cause areas of infarction. Sterility is caused by scars and atrophy of the testis after resolution of viral infection. In the enzyme-rich pancreas, lesions may be destructive, causing parenchymal and fat necrosis and neutrophil-rich inflammation. Mumps encephalitis causes perivenous demyelination and perivascular mononuclear cuffing.
Poliovirus Infection Poliovirus is a spherical, unencapsulated RNA virus of the enterovirus genus. There are three major strains of poliovirus, each of which is included in the Salk formalin-fixed (killed) vaccine and the Sabin oral, attenuated (live) vaccine. Poliovirus is transmitted by the fecal-oral route. It first infects tissues in the oropharynx, then is secreted into the saliva and swallowed, and subsequently multiplies in the intestinal mucosa and lymph nodes, causing a transient viremia and fever. The virus infects only humans. Most polio infections are asymptomatic, in about 1 of 100 infected persons poliovirus invades the CNS and replicates in motor neurons of the spinal cord (spinal poliomyelitis) or brain stem (bulbar poliomyelitis). The diagnosis can be made by viral culture of throat secretions or stool, or by serology
West Nile Virus West Nile virus is an arthropod-borne virus of the flavivirus group, which also includes viruses that cause dengue fever and yellow fever. West Nile virus is transmitted by mosquitoes to birds and to mammals. Wild birds develop prolonged viremia and are the major reservoir for the virus. Humans are usually incidental hosts. West Nile virus has been transmitted by blood transfusion, transplanted organs, breast milk, and transplacentally. After inoculation by a mosquito, West Nile virus replicates in skin dendritic cells, which then migrate to lymph nodes, where virus replicates further, enters the bloodstream. In the CNS the virus infects neurons.
West Nile Virus West Nile virus infection is usually asymptomatic, but in 20% of infected individuals it gives rise to a mild, short-lived febrile illness associated with headache and myalgia. A maculopapular rash is seen in approximately half the cases. CNS complications (meningitis, encephalitis, meningoencephalitis) are not frequent. There is a mortality of about 10% in people with meningoencephalitis and long-term cognitive and neurologic impairment in many survivors.
Viral Hemorrhagic Fevers Viral hemorrhagic fevers (VHFs) are systemic infections. They are caused by enveloped RNA viruses in four different families: arenaviruses, filoviruses, bunyaviruses, and flaviviruses. Viruses all depend on an animal or insect host for survival and transmission. VHF viruses are restricted geographically to areas in which their hosts reside. Viruses that cause hemorrhagic fever (Ebola, Marburg, Lassa) also can spread from person to person. VHF viruses produce a spectrum of illnesses, ranging from relatively mild acute disease characterized by fever, headache, myalgia, rash, neutropenia, and thrombocytopenia to severe, life- threatening disease in which there is sudden hemodynamic deterioration and shock. Potential biologic weapons.
Viral Hemorrhagic Fevers The pathogenesis of viral hemorrhagic fevers is not well understood. The hemorrhagic manifestations are due to thrombocytopenia or severe platelet or endothelial dysfunction. Typically there is increased vascular permeability. There may be necrosis and hemorrhage in many organs, particularly the liver. Most disease manifestations are related to activation of innate immune responses.
CHRONIC LATENT INFECTIONS (HERPESVIRUS INFECTIONS) Herpesviruses are large encapsulated viruses that have a double- stranded DNA genome that encodes approximately 70 proteins. Herpesviruses cause acute infection followed by latent infection in which the viruses persist in a noninfectious form with periodic reactivation and shedding of infectious virus. Latency is operationally defined as the inability to recover infectious particles from cells that harbor the virus.
Herpes Simplex Virus (HSV) HSV-1 and HSV-2 differ serologically but are genetically similar and cause a similar set of primary and recurrent infections. Replicate in the skin and the mucous membranes at the site of entrance of the virus (oropharynx or genitals), where they produce infectious virions and cause vesicular lesions of the epidermis. The viruses spread to sensory neurons that innervate these primary sites of replication. Viral nucleocapsids are transported along axons to the neuronal cell bodies, where the viruses establish latent infection.
Morphology HSV-infected cells contain large, pink to purple intranuclear inclusions (Cowdry type A) that consist of intact and disrupted virions. HSV-1 and HSV-2 cause lesions ranging from self-limited cold sores and gingivostomatitis to life-threatening disseminated visceral infections and encephalitis. Intraepithelial vesicles by HSV-1 (blisters - intracellular edema and ballooning degeneration of epidermal cells), burst and crust over. Genital herpes is more often caused by HSV-2. It is characterized by vesicles on the genital mucous membranes as well as on the external genitalia that are converted into superficial ulcerations. HSV-2 infection in the neonate may be mild, but more commonly it is fulminating with generalized lymphadenopathy, splenomegaly, and necrotic foci throughout the lungs, liver, adrenals, and CNS. Two forms of corneal lesions are caused by HSV. Disseminated skin and visceral herpes infections are usually encountered in hospitalized patients with some form of underlying cancer or immunosuppression. Kaposi varicelliform eruption is a generalized vesiculating involvement of the skin, whereas eczema herpeticum is characterized by confluent, pustular, or hemorrhagic blisters.
Varicella-Zoster Virus (VZV) Two conditions chickenpox and shingles. Acute infection with VZV causes chickenpox; reactivation of latent VZV causes shingles (also called herpes zoster). Chickenpox is mild in children but more severe in adults and in immunocompromised people. VZV infects mucous membranes, skin, and neurons and causes a self-limited primary infection in immunocompetent individuals. VZV evades immune responses and establishes a latent infection in sensory ganglia. VZV is transmitted in epidemic fashion by aerosols, disseminates hematogenously, and causes widespread vesicular skin lesions. Most people do not have a recurrence of VZV.
Morphology The chickenpox rash occurs approximately 2 weeks after respiratory infection. Lesions appear in multiple waves centrifugally from the torso to the head and extremities. Each lesion progresses rapidly from a macule to a vesicle, which resembles a dewdrop on a rose petal. After a few days most chickenpox vesicles rupture, crust over, and heal by regeneration, leaving no scars. Bacterial superinfection of vesicles that are ruptured by trauma may lead to destruction of the basal epidermal layer and residual scarring. Shingles occurs when VZV that has long remained latent in the dorsal root ganglia after a previous chickenpox infection is reactivated and infects sensory nerves that carry it to one or more dermatomes. There, the virus infects keratinocytes and causes vesicular lesions, which, unlike chickenpox, are often associated with intense itching, burning, or sharp pain because of the simultaneous radiculoneuritis. This pain is especially severe when the trigeminal nerves are involved.
Cytomegalovirus (CMV) Cytomegalovirus (CMV), a -group herpesvirus, can produce a variety of disease manifestations, depending on the age of the host, and on the host s immune status. CMV latently infects monocytes and their bone marrow progenitors and can be reactivated when cellular immunity is depressed. CMV causes an asymptomatic or mononucleosis- like infection in healthy individuals but devastating systemic infections in neonates and in immunocompromised people. As its name implies, CMV-infected cells exhibit gigantism of both the entire cell and its nucleus. Within the nucleus is a large inclusion surrounded by a clear halo (owl s eye).
Cytomegalovirus (CMV) Transmission of CMV can occur by several mechanisms, depending on the age group affected: - Transplacental transmission can occur from a newly acquired or primary infection in a mother ( congenital CMV ). - Neonatal transmission can occur through cervical or vaginal secretions at birth or, later, through breast milk ( perinatal CMV ). - Transmission can occur through saliva during preschool years, especially in day care centers. - Transmission by the venereal route is the dominant mode after about 15 years of age, but spread may also occur via respiratory secretions and the fecal-oral route. - Iatrogenic transmission can occur at any age through organ transplants or blood transfusions. Acute CMV infection induces transient but severe immunosuppression. CMV can infect dendritic cells and impair their maturation and ability to stimulate T cells. CMV can both hide from immune defenses and actively suppress immune responses.
Morphology The characteristic enlargement of infected cells. In the glandular organs, the parenchymal epithelial cells are affected; in the brain, the neurons; in the lungs, the alveolar macrophages and epithelial and endothelial cells; and in the kidneys, the tubular epithelial and glomerular endothelial cells. Disseminated CMV causes focal necrosis with minimal inflammation in virtually any organ
Congenital CMV Infections Infection acquired in utero may take many forms. In approximately 95% of cases it is asymptomatic. Affected infants may suffer intrauterine growth retardation, be profoundly ill, and manifest jaundice, hepatosplenomegaly, anemia, bleeding due to thrombocytopenia, and encephalitis. In fatal cases the brain is often smaller than normal (microcephaly) and may show foci of calcification. The infants who survive usually have permanent deficits, including mental retardation, hearing loss, and other neurologic impairments. Most infants with this milder form of cytomegalic inclusion disease recover.
Perinatal Infections Infection acquired during passage through the birth canal or from breast milk is asymptomatic in the vast majority of cases, but infants may develop an interstitial pneumonitis, failure to thrive, skin rash, or hepatitis. These children have acquired maternal antibodies against CMV, which reduce the severity of disease.
Cytomegalovirus Mononucleosis In healthy young children and adults the disease is nearly always asymptomatic. The most common clinical manifestation of CMV infection in immunocompetent hosts beyond the neonatal period is an infectious mononucleosis like illness, with fever, atypical lymphocytosis, lymphadenopathy, and hepatomegaly accompanied by abnormal liver function test results, suggesting mild hepatitis. Most people recover without any sequelae. Once infected a person becomes seropositive for life. The virus remains latent within leukocytes.
CMV in Immunosuppressed Individuals. Immunocompromised individuals are susceptible to severe CMV infection. CMV is the most common opportunistic viral pathogen in AIDS. Serious, life-threatening disseminated CMV infections primarily affect the lungs (pneumonitis) and gastrointestinal tract (colitis). The pneumonitis can progress to full-blown acute respiratory distress syndrome. Intestinal necrosis and ulceration can develop and be extensive, leading to the formation of pseudomembranes and debilitating diarrhea.
TRANSFORMING INFECTIONS This group includes several viruses that have been implicated in the causation of human cancer: EBV, HPV, HBV, HTLV-1.
Epstein-Barr Virus (EBV) EBV causes infectious mononucleosis, a benign, self-limited lymphoproliferative disorder, and is associated with the development of a number of neoplasms, most notably certain lymphomas and nasopharyngeal carcinoma. Infectious mononucleosis is characterized by fever, generalized lymphadenopathy, splenomegaly, sore throat, and the appearance in the blood of atypical activated T lymphocytes (mononucleosis cells).
Pathogenesis EBV is transmitted by close human contact, frequently with the saliva during kissing. The viral infection begins in nasopharyngeal and oropharyngeal lymphoid tissues. EBV gains access to submucosal lymphoid tissues. Here, infection of B cells may take one of two forms. In a minority of B cells there is productive infection with lysis of infected cells and release of virions, which may infect other B cells. In most B cells, EBV establishes latent infection. The symptoms of infectious mononucleosis appear upon initiation of the host immune response. In hosts with acquired defects in cellular immunity this proliferation can progress through a multistep process to EBV-associated B-cell lymphomas.
Morphology The major alterations involve the blood, lymph nodes, spleen, liver, CNS, and, occasionally, other organs. The peripheral blood shows absolute lymphocytosis. The lymph nodes are typically discrete and enlarged throughout the body, principally in the posterior cervical, axillary, and groin regions. Occasionally, EBV-infected B cells resembling Reed-Sternberg cells may be found. B-cell areas (follicles) may also be hyperplastic, but this is usually mild. The spleen is enlarged in most cases, weighing between 300 and 500 gm. It is usually soft and fleshy, with a hyperemic cut surface. These spleens are especially vulnerable to rupture, possibly in part because the rapid increase in size produces a tense, fragile splenic capsule
Clinical Features Infectious mononucleosis classically presents with fever, sore throat, lymphadenitis. However, atypical presentations are common, and include malaise, fatigue, and lymphadenopathy, raising the specter of leukemia or lymphoma. The diagnosis depends on the following findings: (1) lymphocytosis with the characteristic atypical lymphocytes in the peripheral blood, (2) a positive heterophile antibody reaction (monospot test), (3) specific antibodies for EBV antigens (viral capsid antigens, early antigens, or Epstein-Barr nuclear antigen). In most patients, infectious mononucleosis resolves within 4 to 6 weeks. The failure to control EBV infection leads to chronic infectious mononucleosis, agammaglobulinemia, and B-cell lymphoma, each of which proves fatal in about a third of patients.
HIV and AIDs AIDS is a disease caused by the retrovirus human immunodeficiency virus (HIV) and characterized by profound immunosuppression that leads to opportunistic infections, secondary neoplasms, and neurologic manifestations.
Epidemiology The epidemiology of AIDS is quite different in children under age 13. Close to 2% of all AIDS cases occur in this pediatric population, and worldwide over 500,000 new cases and almost 400,000 deaths were reported in children in the year 2006. The three major routes of transmission are sexual contact, parenteral inoculation, and passage of the virus from infected mothers to their newborns
Etiology: The Properties of HIV AIDS is caused by HIV, a nontransforming human retrovirus belonging to the lentivirus family. Two genetically different but related forms of HIV, called HIV-1 and HIV-2, have been isolated from patients with AIDS. HIV-1 is the most common type associated with AIDS in the United States, Europe, and Central Africa, whereas HIV-2 causes a similar disease principally in West Africa and India. Specific tests for HIV-2 are available, and blood collected for transfusion is routinely screened for both HIV-1 and HIV-2 seropositivity.
Pathogenesis of HIV Infection and AIDS While HIV can infect many tissues, there are two major targets of HIV infection: the immune system and the central nervous system Profound immune deficiency, primarily affecting cell-mediated immunity, is the hallmark of AIDS. Severe loss of CD4+ T cells and impairment in the function of surviving helper T cells HIV enters the body through mucosal tissues and blood and first infects T cells as well as dendritic cells and macrophages. The infection becomes established in lymphoid tissues, where the virus may remain latent for long periods. Active viral replication is associated with more infection of cells and progression to AIDS
Mechanism of T-Cell Immunodeficiency in HIV Infection Loss of CD4+ T cells is mainly because of infection of the cells and the direct cytopathic effects of the replicating virus Approximately 100 billion new viral particles are produced every day, and 1 to 2 billion CD4+ T cells die each day HIV colonizes lymphoid organs (spleen, lymph nodes, tonsils) and may cause progressive destruction of the architecture and cellular composition of lymphoid tissues. Chronic activation of uninfected cells, responding to HIV or to infections that are common in individuals with AIDS, leads to apoptosis of these cells by the process of activation-induced cell death Fusion of infected and uninfected cells with formation of syncytia (giant cells) can occur Apoptosis of uninfected CD4+ T cells by binding of soluble gp120 to the CD4 molecule, followed by activation through the T-cell receptor by antigens.
HIV Infection of Non-T Cells HIV-1 can infect and multiply in terminally differentiated nondividing macrophages. This property of HIV-1 is dependent on the HIV-1 vpr gene. Infected macrophages bud relatively small amounts of virus from the cell surface, but these cells contain large numbers of virus particles located in intracellular vacuoles. Macrophages may be reservoirs of infection, whose output remains largely protected from host defenses. In late stages of HIV infection, when CD4+ T-cell numbers decline greatly, macrophages may be an important site of continued viral replication. Macrophages act as gatekeepers of infection. Recall that in more than 90% of cases acute HIV infection is characterized by predominantly circulating Mtropic strains.
Pathogenesis of Central Nervous System Involvement the nervous system is a major target of HIV infection. Macrophages and microglia are the predominant cell types in the brain that are infected with HIV. HIV is carried into the brain by infected monocytes. HIV isolates from the brain are almost exclusively M-tropic. The mechanism of HIV-induced damage of the brain, however, remains obscure. Neurologic deficit is caused indirectly by viral products and by soluble factors produced by infected microglia (IL-1, TNF, and IL-6).
Primary Infection, Virus Dissemination, and the Acute Retroviral Syndrome. Acute (early) infection is characterized by infection of memory CD4+ T cells in mucosal lymphoid tissues, and death of many infected cells. Dendritic cells capture the virus and then migrate into the lymph nodes. The virus disseminates, the individual mounts antiviral humoral and cell- mediated immune responses. There is a drop in viremia to low levels by about 12 weeks after the primary exposure. The acute retroviral syndrome is the clinical presentation of the initial spread of the virus and the host response. Clinically = self-limited acute illness with nonspecific symptoms, resembling a flu-like syndrome.
Chronic Infection: Phase of Clinical Latency. In chronic phase of the disease, lymph nodes and the spleen are sites of continuous HIV replication and cell destruction. During this period few or no clinical manifestations of the HIV infection are present. Over a period of years, the continuous cycle of virus infection, T-cell death, and new infection leads to a steady decline in the number of CD4+ T cells in the lymphoid tissues and the circulation. The final phase is progression to AIDS, characterized by a breakdown of host defense, a dramatic increase in plasma virus, and severe, life- threatening clinical disease. Typically the patient presents with long-lasting fever (>1 month), fatigue, weight loss, and diarrhea.
Clinical Features of AIDS