Unique Challenges of Opioid Use Disorders in Older Adults
Addressing the increasing issue of opioid use disorders in older adults, this educational lecture highlights the differences in presentation, evaluation, and treatment. It explores the complexities of co-occurring medical, neurological, and psychiatric conditions and focuses on raising awareness for safe patient care across various care settings.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Opioid Use Disorders in Older Adults Paul B Hill MD Spring 2023
Disclosures I am a paid educator for Myriad Genetics for Genesight Psychopharmacogenetic Testing
Goals and objectives Highlight the differences in presentation, evaluation and treatment of Opioid use disorder in Older Adults Explore Co Occurring Medical, Neurological and Psychiatric disorders that complicate the treatment Raise awareness of safely treating patients in a variety of levels of care
Introduction This lecture will address the unique issues related to Opioid Use Disorders in the Older Adult in the US This is an increasing issue over the years seeing a 50% increase There is knowledge gap among Physicians in recognition and interventions to treat and prevent disorder and death
Recognition Falls Accidents Poor health Cognitive Decline Mood and Anxiety symptoms Multiple controlled substances Multiple providers CSMD verification Intoxication and withdrawal Continued use of opioids beyond the timeframe of expected recovery Staph infections
Substance Induced Disorders from Opioids Neurocognitive Disorders Delirium Depression and anxious distress(Hyperkatifeia) Hyperalgesia
Special problems in recognition in older adults Isolation Retirement Bias Normalizing the drug use behavior Reduction in tolerance and amount used to cause impairment Acceptance that chronic opioid therapy is safe and effective for persistent pain
Barriers for Older Adults Lack of centers that can support the needs of patients with mobility and medical issues Lack of Addiction trained Physicians Medicare Coverage for needed services may be insufficient to cover the costs of tests, drug screening, and medications Patient s unwillingness to enter group settings Transportation issues
The Complex Older Adult Polypharmacy and multiple addictive substances Medical, Neurological, Psychiatric and Addiction History Drug to drug interactions, Drug to illness interaction, and drug to disease interaction Level of care needed to address safe detoxification Support systems that have various attitudes toward recovery from addiction Acceptance of Medical assisted therapies, relapse prevention and harm reduction techniques
Polysubstance use and dependence Many medications cannot be abruptly stopped in an outpatient setting. Communication with other physicians/patients/families must occur to ensure safety. Every Physician shares the responsibility of safe and proper care and education of the patient about risk Physicians are not required to continue medications that are inappropriate or risky. There are specialty clinics to address polysubstance use
Opioids and Benzodiazepine Higher level of care is needed for detox and transition Long-acting opioids and long-acting benzodiazepines are carrying the most risk in the older adult( 20% mortality risk per year) There are alternate medications to address anxiety symptoms and pain. There needs to be coordination between the pain specialist, addiction specialist and psychiatrist to ensure safety.
Evaluation of the Older Adult with Opioid Addiction Complete Psychiatric, Addiction, Medical, Surgical, and Neurological sequential history Collaborative History Family History Social, educational, occupation, and legal history Medical record review Substance use history including prescribed Opioids Longest period of remission and recovery method
Motivated Behavioral Perspective Interplay between Choice, Physiological Drive and Conditioned Learning Choice Physiological Conditioned Drive Learning Suicide &Hysteria are behaviors with complex Genetic, Social, and Illness factors. The Addiction Neurocircuitry can be included in another lecture
Opioids Codeine Fentanyl Heroin Hydrocodone Hydromorphone Meperidine Methadone Morphine Opium Oxycodone Oxymorphone Tramadol Tapentadol Buprenorphine butorphanol nalbuphine hydrochloride Kratom
Opioid use for Non-Cancer pain Questionnaires that assess risk of aberrant drug-related behaviors Screener and Opioid Assessment for Patients with Pain (SOAPP) Version 1, the revised SOAPP (SOAPP-R)-Self Reporting Opioid Risk Tool (ORT)-Self reporting Diagnosis, Intractability, Risk, Efficacy (DIRE)-Clinician administered questionnaires that assess risk of aberrant drug- related behaviors.
Intervention Physicians will need to refer patients for detoxication or referral to for Medication Assisted Therapy The medically compromised patient may need hospitalization Patients without support may need to be referred to an appropriate residential treatment center and continued care in IOP and PHP Opioid and non opioid method may be choses for both safety and effectiveness
Levels of Care for Detoxification and MAT Office using scales, drug screens, group, and individual therapies IOP and PHP Residential treatment Inpatient and detoxification units. Commitment may be needed for life threatening use. Medical Hospital settings for medically complex and polysubstance use patients
Medical Assisted Therapies Buprenorphine-Multiple formulations and delivery mechanisms. Methadone Naltrexone by mouth and monthly injection
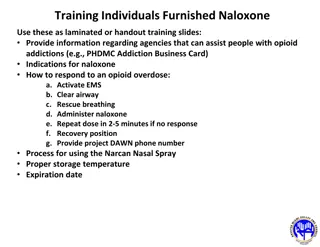
Multimodal Relapse Prevention Strategy Environment change Openness with all physicians, family, and peers Group supports- AA, NA, Dual Recovery, Celebrate recovery Medications for MAT, harm reduction, and relapse prevention
Resources Geriatrics at your Fingertips 24thEdition 2022 Textbook of Geriatric Neuropsychiatry 3rdEdition by Coffey and Cummings The Perspectives of Psychiatry 2ndEdition by McHugh and Slavney CASA Columbia National Advisory Commission on Addiction Treatment 2012 2020 National Survey on Drug use and Health
Conclusion Questions and Comments