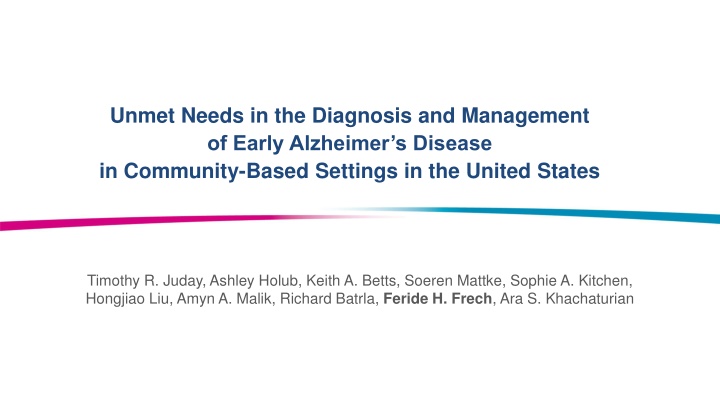
Unmet Needs in Early Alzheimer's Disease Diagnosis and Management
Explore the challenges in diagnosing and managing early Alzheimer's disease in community-based settings in the United States. The study highlights the low diagnosis rates for mild cognitive impairment and Alzheimer's, along with disparities in diagnosis among racial and ethnic minority groups. Understanding these issues is crucial for improving care delivery, especially with the introduction of new treatments.
Uploaded on | 0 Views
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Unmet Needs in the Diagnosis and Management of Early Alzheimer s Disease in Community-Based Settings in the United States Timothy R. Juday, Ashley Holub, Keith A. Betts, Soeren Mattke, Sophie A. Kitchen, Hongjiao Liu, Amyn A. Malik, Richard Batrla, Feride H. Frech, Ara S. Khachaturian
Acknowledgments and Disclosures Timothy R. Juday and Feride H Frech are employees of Eisai. Richard Batrla is a former employee of Eisai. Ashley Holub, Keith A. Betts, Sophie A. Kitchen, and Hongjiao Liu are employees of Analysis Group, Inc, which received support for consulting services from Eisai. Amyn A. is a former employee of Analysis Group. Soeren Mattke has received consulting and speaker fees from Biogen, C2N, Eisai, Eli Lilly, Novartis, Novo Nordisk and Roche/Genentech Ara S. Khachaturian, Ph.D. is an officer and director of the Campaign to Prevent Alzheimer s Disease/Brain Watch Coalition (PAD 20/20) and has received consulting and speaker fees from Alzheimer s Association, Acadia Pharmaceuticals, Alzheon, Biogen, Eisai, Eli Lilly & Company, High Lantern Group, RELX Plc, and Serdi Publishing 2
Background and Objective While mild cognitive impairment (MCI) due to Alzheimer s disease (AD) and mild AD have been highlighted as focal points for intervention, studies show that only 8% of patients with MCI receive a diagnosis1,2 Challenges to a timely diagnosis include a lack of uniform guidelines, difficulties disentangling symptoms from aging, differences in provider training, and limited access to diagnostic tools3 o Racial and ethnic minority groups are less likely to receive a timely and accurate diagnosis of AD Racial minorities are more likely to have a missed or delayed diagnosis of dementia, and more commonly receive a diagnosis at a more advanced stage of AD4 o An increased understanding of the diagnosis and management processes for early AD in community-based settings, where most patients are seen, can help identify problems in care delivery This is especially important given the introduction of monoclonal antibody treatments targeted at early AD patients o This study assessed the impact of demographic characteristics on the diagnosis and management of early AD patients in community-based settings [1] Liss, JL., et al. Practical recommendations for timely, accurate diagnosis of symptomatic Alzheimer's disease (MCI and dementia) in primary care: a review and synthesis. J Intern Med. 2021; 290(2) [2] Mattke, S., et al. Expected and diagnosed rates of mild cognitive impairment and dementia in the U.S. medicare population: observational analysis. Alzheimers Res Ther. 2023; 15(128) [3] Porsteinsson, AP., et al. Diagnosis of early Alzheimer s disease: clinical practice in 2021. J Prev Alzheimers Dis. 2021; 8(371) [4] Gilligan, AM., et al. Health disparities in cost of care in patients with Alzheimer s disease: an analysis across 4 state Medicaid populations. Am J Alzheimers Dis Other Demen. 2013; 28(1) 3
Study Design Retrospective chart review study in community-based primary care & neurology practices recruited from a verified physician panel with broad geographic representation across the US Site Selection Criteria Primary care physician (PCP) or neurologist whose primary practice setting was identified as community-based Had seen at least 15 patients with MCI or mild AD in the past 12 months Had at least 3 years in practice (inclusive of residency/fellowship) Did not consider MCI and mild AD to be interchangeable diagnoses Patient Inclusion Criteria (for Patient Chart Data) Received a diagnosis of MCI due to AD or mild AD within the past 2 years Had a clinic visit within 12 months prior to the date of chart abstraction Aged 50-89 years old, on the date of diagnosis 4
Data Collection An electronic case report form (eCRF) was developed to standardize data collection Data elements were determined based on a literature review and expert input Each physician was required to abstract data for at least 2 MCI and 1 mild AD patient chart(s), up to a maximum of 5 patient charts The following patient data were abstracted: Patient demographic information and comorbidities Information about the diagnostic process, including neurocognitive assessments, biomarker and imaging assessments, and laboratory testing Referral information Pharmacological treatments o o o o 5
Statistical Methods To assess differences by patient demographic characteristics, results were stratified by: o Patient age at diagnosis (<65 vs 65 years) o Patient race (White race vs Other race) o Patient sex (Male vs Female) o Patient location of residence (Urban/suburban vs. Rural) Continuous data was reported as mean and standard deviation (SD); t-tests were used to compare means Categorical data was reported using frequency counts and percentages; chi-squared tests or Fisher s exact tests were used to compare categories 6
Patient Demographics Overall Sample Strengths Limitations Patient demographics overall Overall (N=1,284) 70.2 7.9 Mean age at diagnosis SD 817 (63.6%) Diagnosis of MCI due to AD 724 (56.4%) Male sex Race1 863 (67.2%) White 218 (17.0%) Black or African American 129 (10.0%) Asian 56 (4.4%) Other2 25 (1.9%) Unknown 1,039 (80.9%) Suburban/urban residence Insurance type1 955 (74.4%) Medicare 292 (22.7%) Private health insurance 136 (10.6%) Other/Unknown3 [1] Response allowed for selection of multiple races and multiple insurance types. [2] Other races include American Indian or Alaska Native, Native Hawaiian or Other Pacific Islander, and Other races (unspecified). [3] Other insurance types include Medicaid and Other insurance types (unspecified). 7
Patient Demographics Stratified Strengths Limitations Patient demographics were similar across strata, with the exception of Medicare payer status by age Overall (N=1,284) < 65 years (N=275) 65 years (N=1,009) Patient demographics by age at diagnosis 70.2 7.9 59.0 4.0 73.3 5.6 Mean age at diagnosis SD 817 (63.6%) 186 (67.6%) 631 (62.5%) Diagnosis of MCI due to AD 724 (56.4%) 153 (55.6%) 571 (56.6%) Male sex 863 (67.2%) 185 (67.3%) 678 (67.2%) White race1 1,039 (80.9%) 231 (84.0%) 808 (80.1%) Suburban/urban residence 955 (74.4%) 88 (32.0%) 867 (85.9%) Medicare insurance type1 Overall (N=1,259) White race (N=857) Other race (N=402) Patient characteristics by race2 70.3 7.9 70.4 7.9 69.9 7.9 Mean age at diagnosis SD 803 (63.8%) 548 (63.9%) 255 (63.4%) Diagnosis of MCI due to AD 709 (56.4%) 471 (55.0%) 238 (59.4%) Male sex 1,021 (81.1%) 668 (77.9%) 353 (87.8%) Suburban/urban residence 944 (75.0%) 657 (76.7%) 287 (71.4%) Medicare insurance type1 [1] Response allowed for selection of multiple races and multiple insurance types. [2] For purposes of the race stratification analysis, patients who indicated White race and other race were categorized as other race. A total of 6 patients indicated White race and one other race. 8
Patient Demographics Stratified Patient demographics were similar across strata, with the exception of race by location of residence Overall (N=1,278) Male (N=724) Female (N=554) Patient demographics by sex 70.2 7.9 70.1 7.7 70.4 8.2 Mean age at diagnosis SD 813 (63.6%) 471 (65.1%) 342 (61.7%) Diagnosis of MCI due to AD 862 (67.4%) 475 (65.6%) 387 (69.9%) White race1 1,037 (81.1%) 592 (81.8%) 445 (80.3%) Suburban/urban residence 952 (74.5%) 537 (74.2%) 415 (74.9%) Medicare insurance type1 Overall (N=1,255) Urban/suburban (N=1,039) Rural (N=216) Patient characteristics by location of residence 70.2 7.9 70.0 8.0 71.4 7.6 Mean age at diagnosis SD 800 (63.7%) 673 (64.8%) 127 (58.8%) Diagnosis of MCI due to AD 709 (56.7%) 592 (57.1%) 117 (54.9%) Male sex 847 (67.5%) 673 (64.8%) 174 (80.6%) White race1 939 (74.8%) 761 (73.2%) 178 (82.4%) Medicare insurance type1 [1] Response allowed for selection of multiple races and multiple insurance types. 9
Diagnostic, Referral, and Treatment Patterns, by Age and Race Diagnostic Process Referral Patterns Pharmacological Treatment Patterns A memory complaint from a caregiver triggered the diagnostic process more frequently for patients 65 years compared to patients <65 years (69.5% vs 58.9%; p<0.01) No differences in the receipt of any treatment by age or race were observed No differences in the receipt of referrals by age or race were observed Patients aged <65 years were more likely to wait 4 months from referral to visit than patients aged 65 years (54.4% vs 20.9%; p<0.001) Patients aged 65 years had fewer visits between the initial visit and diagnosis compared to patients aged <65 years (2.6 vs 3.0; p<0.001) Patients aged <65 years were more likely to receive monoclonal antibody agents than those aged 65 years (15.6% vs 3.0%; p<0.001) Patients of other races had a longer time to diagnosis (mean: 5.5 4.9 months) relative to patients of White race (mean: 4.6 4.4 months) (p<0.01) 10
Neurocognitive Assessments and Biomarker/Imaging Tests, by Age Key Findings by Age Patients aged <65 years were less likely to have a neurocognitive assessment & a biomarker/imaging test compared to patients aged 65 years Patients aged <65 years were more likely to receive an AD specific biomarker assessment (including a CSF test, tau PET scan, or amyloid PET scan) 11
Neurocognitive Assessments and Biomarking/Imaging Tests, by Race Key Findings by Race Patients of White race were more likely to receive a neurocognitive assessment than patients of other races; nearly 20% of patients of other race did not receive a neurocognitive assessment 12
Diagnostic, Referral, and Treatment Patterns, by Sex and Location Diagnostic Process Referral Patterns Pharmacological Treatment Patterns Female patients were more likely to have a family member or caregiver trigger the diagnostic process due to a memory complaint (70.8% vs 64.9%; p<0.05) Females and males received a similar proportion of referrals. Among those who received a referral, the time to referral was also similar No differences in the receipt of any treatment by sex or the patient s location of residence were observed No differences in the use of neurocognitive assessments by sex or patient s location of residence were observed Urban/suburban patients were more likely to be prescribed monoclonal antibody agents targeting beta- amyloid (6.5% vs. 2.3%; p <0.05) No difference in the receipt of a referral by the patient s location of residence was observed No differences in the receipt of biomarker/imaging tests by sex were observed Patients residing in urban/suburban locations were more likely to receive specialized imaging tests, including an fMRI FDG-PET, or DTI imaging test compared to patients in rural locations 13
Key Differences By Age: Patients aged 65 years had a faster time to referral visit with only 20.9% seen 4 months compared to 54.4% of patients aged <65 years By Race: Patients of White race were more likely to receive a neurocognitive assessment compared to patients of other races By Sex: Female patients were more likely to have a family member trigger the diagnostic process By Location: Rural patients were less likely to be prescribed monoclonal antibody agents targeting beta-amyloid 14
Limitations and Conclusions Limitations The data presented relied on the reporting accuracy of each physician who conducted chart abstractions Selection bias, particularly of physicians with greater awareness of the diagnosis and management of early AD may have resulted from the panel design Conclusions As neurocognitive assessments are recommended as diagnostic tools are by various professional organizations, more work is needed to close gaps in their use, particularly with regards to race Likewise, use of biomarker/imaging tests appeared to be impacted by patient location of residence, suggesting unmet needs related to access As early detection and treatment are critical to optimizing outcomes, more effort needs to be focused on reducing care disparities 15