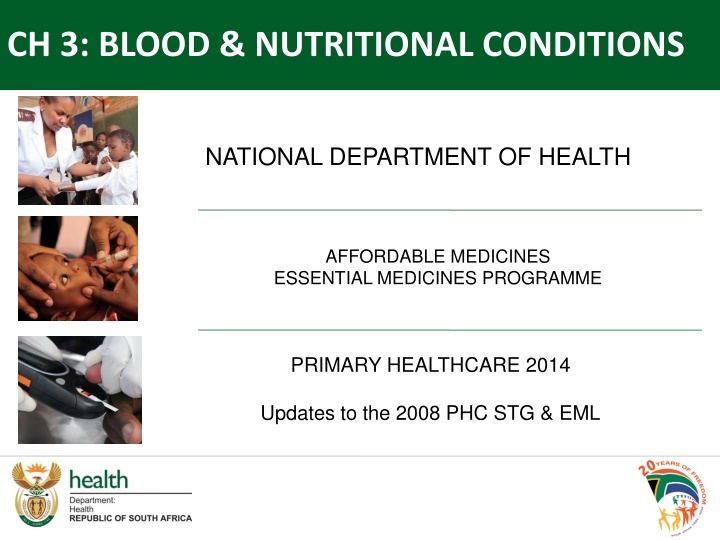
Updates in Blood & Nutritional Conditions: Anaemia Management Guidelines
The National Department of Health's Affordable Medicines Essential Medicines Programme in 2014 introduced updated guidelines for managing anaemia, focusing on oral iron dosing regimens for adults and children, iron supplementation, follow-up protocols, and the management of macrocytic or megaloblastic anaemia. The guidelines provide insights into dosing frequencies, medication options, and follow-up strategies backed by varying levels of evidence to improve primary healthcare services in the field of blood and nutritional conditions.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
CH 3: BLOOD & NUTRITIONAL CONDITIONS NATIONAL DEPARTMENT OF HEALTH AFFORDABLE MEDICINES ESSENTIAL MEDICINES PROGRAMME PRIMARY HEALTHCARE 2014 Updates to the 2008 PHC STG & EML
3.1.1 ANAEMIA, IRON DEFICIENCY Dose frequency of oral iron in adults & children retained as: Three times daily treatment. Once daily prophylaxis. There is a paucity of evidence comparing thrice daily vs. once daily dosing of iron, orally: ADULTS The Adult Hospital level Expert Review Committee (2012) reviewed the evidence pertaining to dosing regimens in pregnancy. But, the Saving Mothers Report had indicated that maternal anaemia was a risk factor for maternal deaths caused by obstetric haemorrhages. Cochrane systematic review: Menstruating women receiving intermittent vs. daily iron supplementation developed anaemia more frequently (RR 1.26; 95% CI 1.04 to 1.51, six trials), despite achieving similar haemoglobin concentrations on average (MD -0.15 g/L; 95% CI -2.20 to 1.91, eight trials). However, the review did not describe the daily dose as once or thrice daily. CHILDREN Studies in paediatrics (6-24 months & 9-12 years) of single vs. thrice daily dose of ferrous sulfate drops over 1-2 months resulted in a similar rate of increase in Hb, with minimal side effects. But, iron administered two to three times a day was better tolerated. Level of Evidence: I Systematic review, RCT PRIMARY HEALTHCARE IMPLEMENTATION SLIDES 2014: BLOOD & NUTRITIONAL 2
3.1.1 ANAEMIA, IRON DEFICIENCY ADULTS Ferrous sulphate compound BPC, oral: amended Ferrous fumarate, oral: added Iron sucrose, IV: not added Iron polymaltose, IM: not added Blood transfusions: not added Ferrous fumarate is available on the current tender. Medicine interaction of iron tablets with calcium tablets was described in the text of the STG, aligned with the SAMF 10th edition, 2012. Iron sucrose, IV; iron polymatose IM blood transfusions not considered pragmatic for primary level of care. Level of Evidence: III Guideline, Expert opinion PRIMARY HEALTHCARE IMPLEMENTATION SLIDES 2014: BLOOD & NUTRITIONAL 3
3.1.1 ANAEMIA, IRON DEFICIENCY CHILDREN Follow up Hb after 14 days. The following text was amended, as children with uncomplicated anaemia could be followed up a month later rather than 14 days later, if there is a response to oral iron therapy. If same or higher continue treatment and repeat after another 14 28 days. Level of Evidence: III Expert opinion PRIMARY HEALTHCARE IMPLEMENTATION SLIDES 2014: BLOOD & NUTRITIONAL 4
3.1.2 ANAEMIA, MACROCYTIC OR MEGALOBLASTIC Vitamin B12, IM: not added Vitamin B12 deficiency is diagnosed and managed at secondary level. Level of Evidence: III Guidelines PRIMARY HEALTHCARE IMPLEMENTATION SLIDES 2014: BLOOD & NUTRITIONAL 5
3.2.1.2 UNCOMPLICATED SEVERE ACUTE MALNUTRITION Vitamin A (retinol), oral: added Multivitamin, oral: added Mebendazole, oral: added The STG was aligned with the Paediatric Hospital level STG, the NDoH Nutrition SAM policy and the IMCI Guidelines. Level of Evidence: III Guidelines PRIMARY HEALTHCARE IMPLEMENTATION SLIDES 2014: BLOOD & NUTRITIONAL 6
3.4 VITAMIN B DEFICIENCIES The description of the various vitamin B deficiencies were described as follows: Vitamin B3/Nicotinic acid deficiency (Pellagra). Vitamin B6/Pyridoxine deficiency. Vitamin B1/Thiamine deficiency (Wernicke encephalopathy and beriberi). PRIMARY HEALTHCARE IMPLEMENTATION SLIDES 2014: BLOOD & NUTRITIONAL 7
3.4 VITAMIN B DEFICIENCIES Vitamin B complex, oral: amended (indicated for all forms of vitamin B deficiencies). As vitamin B deficiencies often co-exist, comprehensive treatment in the form of vitamin B complex was preferred compared to with individual vitamin B components. Level of Evidence: III Expert opinion PRIMARY HEALTHCARE IMPLEMENTATION SLIDES 2014: BLOOD & NUTRITIONAL 8
3.4.1 VITAMIN B3/NICOTINIC ACID DEFICIENCY (PELLAGRA) Nicotinamide: dose amended Nicotinamide doses were delineated to manage severe and mild B3 deficiency in adults and children. Level of Evidence: III Guideline PRIMARY HEALTHCARE IMPLEMENTATION SLIDES 2014: BLOOD & NUTRITIONAL 9
3.4.2 PYRIDOXINE (VITAMIN B6) DEFICIENCY Pyridoxine: dose amended Dose aligned with SAMF 10th edition, 2012. Supportive evidence of pyridoxine supplementation with INH is of poor quality. There is no RCT data, but the recommendation is included in most guidelines. Level of Evidence: III Guidelines PRIMARY HEALTHCARE IMPLEMENTATION SLIDES 2014: BLOOD & NUTRITIONAL 10
3.4.3 VITAMIN B1/THIAMINE DEFICIENCY (WERNICKE ENCEPHALOPATHY & BERIBERI) Thiamine, IM, 100 mg: deleted Dextrose 5 %, IV: deleted Wernicke s encephalopathy is not a common condition. Patients that present with encephalopathy, eye muscle paralysis or cardiac failure require referral to secondary level facilities. Diagnosis and management is done at secondary level, and thus patients are down referred. The irrational use of parenteral B12 and B1 was a concern at primary level. Level of Evidence: III Expert opinion PRIMARY HEALTHCARE IMPLEMENTATION SLIDES 2014: BLOOD & NUTRITIONAL 11
Slide Ref # Reference 3.1 ANAEMIA 2 1 IRON Pe a-Rosas JP, De-Regil LM, Dowswell T, Viteri FE. Intermittent oral iron supplementation during pregnancy. Cochrane Database of Systematic Reviews 2012, Issue 7. Art. No.: CD009997. Beard JL. Effectiveness and strategies of iron supplementation during pregnancy. Am J Clin Nutr 2000;71(suppl):1288S 94S. Ridwan E, Schultink W, Dillon D, and Gross R. Effects of weekly iron supplementation on pregnant Indonesian women are similar to those of daily supplementation. Am J Clin Nutr 1996;63:884-90. Yakoob MY, Bhutta ZA. Effect of routine iron supplementation with or without folic acid on anemia during pregnancy. BMC Public Health 2011, 11(Suppl 3):S21 Pavord S, Myers B, Robinson S, Allard S, Strong J, Oppenheimer C for British Committee for Standards in Haematology. July 2011. UK guidelines on the management of iron deficiency in pregnancy. Haidar J, Omwega AM, Muroki NM and Ayana G. Daily versus weekly iron supplementation and prevention of iron deficiency anaemia in lactating women. East African Medical Journal. January 2003;80(1):11-16. Fern ndez-Gaxiola AC, De-Regil LM. Intermittent iron supplementation for reducing anaemia and its associated impairments in menstruating women. Cochrane Database of Systematic Reviews 2011, Issue 12. Art. No.: CD009218. Zlotkin S, Arthur P, Antwi KY, Yeung G. Randomized, controlled trial of single versus 3-times-daily ferrous sulfate drops for treatment of anemia. Pediatrics.2001 Sep;108(3):613-6. Gunadi D, Rosdiana N, Lubis B. Comparison of once a day and three times a day iron treatment in 9-12 year old elementary school children with iron deficiency anemia. Paediatrica Indonesiana March 2009;49(2):104-107. SAMF, 2012 edition. 3 2 FERROUS SULPHATE COMPUND BPC Contract circular HP09-2014SD 3 2 FERROUS FUMARATE Contract circular HP09-2014SD 5 3 VITAMIN B12 Adult Hospital level STG, 2012 and Paediatric STG, 2013. 3.2 CHILDHOOD MALNUTRITION, INCLUDING NOT GROWING WELL 6 4 VITAMIN A (RETINOL) Paediatric Hospital level STG, 2013. National Department of Health. IMCI Guidelines,2014. National Department of Health Nutrition: Severe Acute Malnutrition policy. 3.2 CHILDHOOD MALNUTRITION, INCLUDING NOT GROWING WELL 6 4 MULTIVITAMIN Paediatric Hospital level STG, 2013. National Department of Health. IMCI Guidelines,2014. National Department of Health Nutrition: Severe Acute Malnutrition policy. 12
Slide Ref # Reference 3.2 CHILDHOOD MALNUTRITION, INCLUDING NOT GROWING WELL 6 4 MEBENDAZOLE Paediatric Hospital level STG, 2013. National Department of Health. IMCI Guidelines,2014. National Department of Health Nutrition: Severe Acute Malnutrition policy. 3.4 VITAMIN B DEFICIENCIES 9 5 NICOTINAMIDE SAMF 10th edition, 2012. 10 6 PYRIDOXINE SAMF 10th edition, 2012. Snider DE Jr. Pyridoxine supplementation during isoniazid therapy.Tubercle.1980 Dec;61(4):191-6. ii. Carlson HB, Anthony EM, Russell WF jr, MiddlebrookG. Prophylaxis of isoniazid neuropathy with pyridoxine. N Engl J Med. 1956 Jul 19;255(3):119-22. Zilber LA, Bajdakova ZL, Gardasjan AN, Konovalov NV, Bunina TL, Barabadze EM. The prevention and treatment of isoniazid toxicity in the therapy of pulmonary tuberculosis. 2. An assessment of the prophylactic effect of pyridoxine in low dosage. Bull World Health Organ. 1963;29:457-81. American Thoracic Society, CDC, and Infectious Diseases Society of America. Treatment of Tuberculosis. Morbidity and Mortality Weekly Report. June 20, 2003 / Vol. 52 / No. RR-11. WHO. Treatment of Tuberculosis guidelines, 4th edition, 2010. Available at: http://www.who.int/tb/publications/2010/9789241547833/en/ Center for Disease Control and Prevention. Latent Tuberculosis Infection: A guide for primary healthcare providers, 2013.[Online] [Cited November 2014] Available at: http://www.cdc.gov/TB/publications/LTBI/default.htm 13







![Enhancing Patient Blood Management in Pregnancy at [INSERT LOCAL HOSPITAL NAME]](/thumb/143207/enhancing-patient-blood-management-in-pregnancy-at-insert-local-hospital-name.jpg)