Urea in Blood: Functions and Measurement
Urea, the major nitrogen compound in blood, is a vital excretory product of protein metabolism. Learn about its formation in the liver, role in renal function, measurement methods, and implications of abnormal levels.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
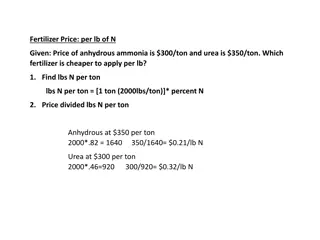
The Nitrogens compound present in highest concentration in the blood is urea. Urea is the major excretory product of protein metabolism. It is formed in the liver from amino groups (-NH2) and/or free ammonia generated during protein catabolism. Since historic assays for urea were based on measurement of nitrogen, the term blood urea nitrogen (BUN)has been used to refer to urea determination. Urea nitrogen (urea N) is a more appropriate term.
Protein metabolism produces amino acids that can be oxidized to produce energy or stored as fat and glycogen. These processes release nitrogen, which is converted to urea and excreted as a waste product. Following synthesis in the liver, urea is carried in the blood to the kidney, where it is readily filtered from the plasma by the glomerulus. Most of the urea in the glomerular filtrate is excreted in the urine, The concentration of urea in the plasma is determined by renal function and perfusion, the protein content of the diet, and the rate of protein catabolism
In the International System of Units (SI), urea is reported in units of millimoles per liter. Urea nitrogen concentration expressed in milligrams per deciliter (mg/dL) may be converted to urea concentration in millimoles per liter by multiplying by 0.357
Urea concentration may be measured in plasma, serum, or urine. Although the protein content of the diet influences urea concentration, the effect of a single protein-containing meal is minimal and a fasting sample is not required usually. A nonhemolyzed sample is recommended. Urea is susceptible to bacterial decomposition, so samples (particularly urine) that cannot be analyzed within a few hours should be refrigerated. Timed urine samples should be refrigerated during the collection period.
ADULT Plasma or serum 15 45 mg/dL (2.1-7.1 mmol urea/day) Urine, 24-h 12-20 g/day (0.43-0.71 mol urea/day)
An elevated concentration of urea in the blood is called azotemia. Very high plasma urea concentration accompanied by renal failure is called uremia, or the uremic syndrome. This condition is eventually fatal if not treated by dialysis or transplantation. Conditions causing increased plasma urea are classified according to cause into three main categories: prerenal, renal, and postrenal.
Prerenal azotemia: is caused by reduced renal blood flow. Less blood is delivered to the kidney; consequently, less urea is filtered. Causative factors include congestive heart failure, shock, hemorrhage, dehydration, and other factors resulting in a significant decrease in blood volume. The amount of protein metabolism also induces prerenal changes in blood urea concentration.
Renal: Decreased renal function causes an increase in plasma urea concentration as a result of compromised urea excretion. Renal causes of elevated urea include acute and chronic renal failure, glomerular nephritis, tubular necrosis, and other intrinsic renal disease. Postrenal azotemia: can be due to obstruction of urine flow anywhere in the urinary tract by renal calculi, tumors of the bladder or prostate, or severe infection.
INCREASED CONCENTRATION Prerenal Congestive heart failure Shock, hemorrhage Dehydration Increased protein catabolism High-protein diet Renal Acute and chronic renal failure Renal disease, including glomerular nephritis, tubular necrosis Postrenal Urinary tract obstruction DECREASED CONCENTRATION Low protein intake Severe vomiting and diarrhea Liver disease Pregnancy