Uterine Leiomyoma: Prevalence, Clinical Picture, Types, Diagnosis, Treatment, and Risks
This article provides comprehensive information on uterine leiomyomas (fibroids), including prevalence, clinical presentation, types, diagnostic methods, treatment options (medical and surgical), and potential malignant changes. Learn about intramural, subserosal, and submucosal fibroids, symptoms like heavy bleeding and pelvic pressure, diagnostic tests like ultrasounds and MRI, and management strategies such as embolization and myomectomy.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
LEIOMYOMA (Fibroid) Case + Video 433OBGYNteam@gmail.com
Objectives Identify the prevalence of leiomyomas. Describe the clinical picture of patient with leiomyoma. List the different types of uterine leiomyoma. Describe the diagnostic methods to confirm uterine leiomyoma. Discuss the treatment options for leiomyoma (medical and surgical) Identify the risk of malignant changes that might occur in leiomyom Video : https://www.youtube.com/watch?v=2aHCVGeHV1M
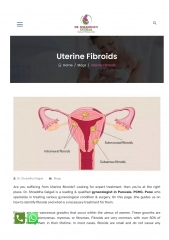
Uterine leiomyoma -Uterine leiomyoma (fibroids) : benign proliferation of smooth muscle cells Types of fibroids: 1. Intrmural fibroids (Within the wall of uterus). 2. Subserosal fibroid (beneath serosa or peritoneum). 3. Submucosal fibroid (beneath the endometrium).
1 out 4 white woman , 1 out 2 African American Woman -Most Common indication for hysterectomy (30%) -hormonal (estrogen) responsive so it is common in pregnancy. and menopause will cause Atrophy (Low oestrogen level)
-Symptoms: Commonly asymptomatic Or 3 classical symptoms: 1. But mostly bleeding or heavy menstruation (due to invasion the endometrium). 2. Pelvic pressure or mass. 3. Dysmenorrhea. -Physical findings: Depends on its number and sizes. Large: palpable abdominally -Note: to comment for size of uterus use word week size uterus this differentiate it from the pregnant uterus or beneath umbilicus Intramural : Cant be felt and usually asymptomatic , unless its enlarges Submucosal: Intermenstrual bleeding (Abnormal Vaginal Bleeding ) SubSerosal : Pressure symptom , Lumpy bumpy (Irregular)
Diagnostic test: by physical examination and imaging studies 1. Pelvic ultrasounds: to quantify the fibroids sizes and numbers. 2. Sonohysterogram. 3. MRI: for location and size -Diagnostic test: 1. Pelvic ultrasounds: to quantify the fibroids sizes and numbers. 2. Sonohysterogram. 3. MRI: for location and size. Treatment: Mostly women not needed for intervention especially if it is found small or incidentally (Observation ) - Medical management: o Oral contraceptive (to reduce bleeding): contraindicated for women over 35 of age, smoke, HTN or with migraine. o Progestin (for bleeding). o Prostaglandin synthase inhibitors (NSAID) (for dysmenorrhea). o GnRH agonist ( to suppress HPO axis) > can be use for pre surgical Shrinkage or for premenopausal woman ( until they reach the menopause )
- Uterine artery embolisation : Catheter is inserted to femoral artery > uterine artery > block the vessels ( fibroid devascularization causing ischemia of myoma) - Surgical options: o Myomectomy ( to maintain fertility ): abdominally, hysteroscopically o Hysterectomy: abdominally or vaginally.
CASE: A 42-year-old G3P3 woman presents with a history of abnormal bleeding and pelvic pain. She was well until approximately age 35, when she began developing dysmenorrhea and progressive menorrhagia. The dysmenorrhea was not fully relieved by NSAIDs. Over the next several years, the dysmenorrhea and menorrhagia became more severe. She then developed intermenstrual bleeding and spotting, as well as pelvic pain, which she describes as a constant feeling of pressure. She also complains of urinary frequency. Past gynecological history is otherwise noncontributory. She delivered three children by Caesarean delivery, the last with a tubal ligation at age 30. Her past medical history is unremarkable.
Physical examination: reveals a well-developed, well-nourished woman in no distress. Vital signs and general physical exam are unremarkable. Abdominal examination reveals an irregular-sized mass extending halfway between the pubic symphysis and umbilicus and to the right of the midline. Pelvic exam reveals a normal appearing vagina and cervix. The uterus is markedly enlarged and irregular, especially on the right side where it appears to reach the lateral pelvic side- walls. The adnexae are not palpable given the size of the mass. Beta HCG is negative. CBC reveals hemoglobin of 10.3 and hematocrit of 31.2%. Indices are hypochromic, microcytic. Serum ferritin confirms mild iron deficiency anemia. Pap test is reported negative for malignancy, adequate for evaluation. Ultrasound shows multiple large intramural fibroids, filling the pelvis and extending into the lower abdomen. Themass does extend into the right side of the pelvis. There is mild hydronephrosis on that side. The ovaries are not visual- ized. Endometrial biopsy reveals proliferative endometrium.
Q1: What are the likely causes of the mass prior to imaging? The most common cause of a large irregular uterine mass is uterine leiomyomata. The clinical picture is typical of a patient with fibroids. The physician must be sure that the patient does not have ovarian neo- plasia. Usually this is accomplished when the ultrasound confirms the diagnosis of fibroids. The differential diagnosis for a pelvic mass includes : physiologic cysts, infection (tubo-ovarian abscess), benign and malignant neoplasms, adenomyosis, endometriosis, and masses related to other ab- dominal/pelvic organ systems.
Q2. What is the prevalence of leiomyoma in different populations of women? Uterine leiomyomas are very common Prevalence is high, with up to 70% of Caucasian women and greater than 80% of African American wom-
Q3:Describe the pathological changes of leiomyomata. Well-circumscribed, non-encapsulated myometrium confirms the diagnosis of fibroids. It is a benign neoplasm. A leiomyosarcoma will have at least 10 abnormal mitoses per high power field, and is diagnosed histologically typically after surgical removal by way of hysterectomy/myomectomy. Fibroids are common; leiomyosarcoma is very rare Pathological diagnosis is made for a patient who undergoes surgery. Biopsy for fibroids is not indicated.
Q4. Discuss the appropriate management of women with fibroids. Expectant management is acceptable if intervention is not warranted by the symptoms. No intervention is needed for women with asymptomatic fibroids. Many women with fibroids are asymptomatic. Provider should discuss patient s desire for fertility when planning treatment. The most frequent presenting symptoms of uterine fibroids are : bleeding ,pressure symptoms,pain, and urinary complaints.
Fibroids can be : subserosal,intramuralorsubmucosal. Submucosal fibroids are frequently associated with bleeding. Pregnancies in women with fibroids are usually uneventful. Fibroids can grow during pregnancy, which may impact fetal growth and mode of delivery. Fibroids are rarely a cause of infertility. There are specific criteria for the use of myomectomy in infertile patients. Oral contraceptives or progestins may be utilized to control bleeding. GNRH agonists may be utilized preoperatively. A levonorgestrel containing intrauterine device can be effective for pain and bleeding in a uterus up to 10 weeks size. Hysteroscopic resection Uterine ablation Uterine artery embolization Myomectomy Hysterectomy
Q5: What are the indications for hysterectomy in women with fibroids? Failure of prior conservative therapies to relieve symptoms When her symptoms have an impact on daily activities Excessive uterine bleeding Profuse bleeding,clots or periods>8days Symptomatic anemia due to the blood loss Pelvic pain caused by the fibroids Acute and severe Chronic lower abdominal or back pressure Bladder pressure causing urinary frequency
Done by: Nouf AlBalla Revised by: Razan AlDhahri