Vaccine Efficacy for People Living with HIV: Practical Implications
In the field of HIV research, understanding vaccine efficacy among individuals living with HIV is crucial. Insights from the 6th Workshop on Healthy Living with HIV in 2021 shed light on the practical implications of this topic. The presentation by Simon Collins delves into the significance of vaccine efficacy for this specific population, addressing concerns such as access, data inclusivity, and impact on transmission and clinical outcomes. Additionally, the intersection of HIV and COVID-19 responses is explored, highlighting the need for information, access to results, and considerations for vaccine prioritization.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Vaccine efficacy for people living with HIV: what does it mean in practice? 6th Workshop on Healthy Living with HIV 2021: 1 2 October 2021 (slides: 1 Sep 21) Simon Collins i-Base.info
Disclosure I have no personal financial conflicts of interest.
HIV community needs (conclusion) Data: information about everything. To be included in all research studies as participants and in their design and running. Timely access to results. Impact of low CD4, detectable viral load, age, sex, comorbidities, occupational risk. To inform how we stay safe: efficacy for transmission vs clinical endpoints. Also, that other groups are asking similar questions... also excluded from phase 3 studies
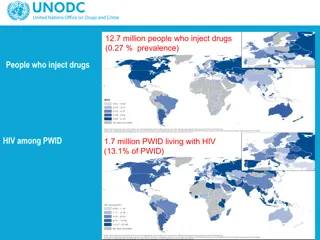
COVID-19: Information... The first HIV community responses to COVID-19 were to want information to stay safe and reduce risk. Impact of HIV on risk of transmission? Similar or worse outcomes including mortality? Easy with electronic records? HIV mortality in UK: good but overlapping cohorts still no single national data.[1, 2, 3] Reluctance to test for HIV - even though in ICU protocol. Case studies, small studies, single-centre results and then increasingly large cohorts - and with HIV data. 1. Mang et al. Geretti et al. BMJ https://i-base.info/htb/38369. 2. ISARIC and OpenSAFELY databases https://i-base.info/htb/38726. 3. Croxford S et al. PHE. https://i-base.info/htb/40508.
Largest US national cohort 1.5 million COVID-19 cases. 8,200 HIV+ and 11,300 solid organ recipients (and 267 with both). Comprehensive HIV history. Increased hospitalisation (aOR: 1.28), intubation (aOR: 1.43) and mortality (aOR: 1.20). CD4<350 - mortality aOR: 7.6 (3.9 to 14.9) VL >1000 c/mL - mortality aOR: 7.3 (2.1 to 25.7) Sun J et al. COVID-19 disease severity among people with HIV infection or solid organ transplant in the united states: a nationally- representative, multicenter, observational cohort study. medRxiv 2021.07.26.21261028; doi: 10.1101/2021.07.26.21261028. (28 July 2021). https://www.medrxiv.org/content/10.1101/2021.07.26.21261028v1.full
Vaccines: Data - and access Similar questions for vaccines? Will efficacy be similar to HIV-negative? Are there more concerns about side effects? UK decided that higher COVID-19 risk supported priority access to vaccines. Still need for information to cover diversity: low CD4, CD4 nadir, CD4:CD8, high viral load. Most HIV positive people globally still need access.
Vaccines: history Remember timeline: We are at least 12-18 months away from a vaccine we could use March 2020. [1] Phase 2/3 vaccine studies excluded HIV positive people. Risk that exclusion from FDA indication would limit access. Studies made no allowance for being on stable ART. Caution from lower HIV+ response to natural COVID-19. [2] Rapid community response from US activists. 1. https://www.cidrap.umn.edu/news-perspective/2020/03/fauci-vaccine-least-year-away-covid-19-death-toll-rises-9- seattle (March 2020). Spinelli MA et al. Lancet HIV, April 2021 and linked editorial. https://i-base.info/htb/40694 2.
Vaccines Decision overturned thanks to coalition of US activists including Lynda Dee, Jeff Taylor, Nelson Vergel, ATAC, pozhealth list etc. https://www.positivelyaware.com https://www.nbcnews.com https://www.poz.com https://i-base.info/htb/38863
Vaccines protocol changes 5 August: Moderna to include people living with controlled HIV who are not otherwise immunosuppressed in phase 3 study. 7 August: Pfizer is now seeking to amend its protocol to allow people living with HIV to participate in its phase II/III trial, along with people successfully treated for HBV and HCV. Small numbers for HIV cohorts with late reporting. Underpowered for clinical efficacy. Generally reported comparable results but for high CD4 (>500) and undetectable viral load (<50 c/mL)
Vaccines results in HIV+ and data gap... Largely with high CD4 and undetectable viral load. Single case had no vaccine response. 1. Frater et al. https://i-base.info/htb/40465. 2. Mahdi et al. https://i-base.info/htb/40465. 3. Shinde V et al. https://i-base.info/htb/40618. 4. Touizer E et al. https://i-base.info/htb/40779. 5. Woldemeskel BA et al. https://i-base.info/htb/41022. 6. Ruddy J et al. https://i- base.info/htb/40677.
June/July 2021: real world data Low immune responses in other groups excluded from phase 3. Older than 80 years. [1] Recipients of solid organs or bone marrow transplants. [2, 3, 4] Use on immunosuppressant medicines. [5, 6] Current or recent chemotherapy. [7] Autoimmune conditions. Advanced HIV? Use of third vaccines in some countries for equity of protection. [6, 7] 1. M ller et al. https://i-base.info/htb/40502. 2. Boyarsky BJ at al. https://i-base.info/htb/40465. 3.. Werbel et al. https://i-base.info/htb/40843. 4. Ali et al. 5. Benotmane et al. https://i-base.info/htb/41022. 6. KamarJ et al. https://i-base.info/htb/40812. 7. https://i-base.info/htb/40634.
HIV and isolation concerns 1. Isolation and remedies for this. 2. Safety in health monitoring. 3. Vaccine hesitancy (avoidance) still an issue. The hope that two vaccines would be enough. Many HIV+ still avoid hospitals and normal life. Infection is still possible, with some having lower response. Limit access to normal activities to those vaccinated. Will some people need four doses? We want health workers to be vaccinated!
UK-CAB web survey 6 Sep 2021 (n=40) Vaccines for health workers Q1: Do you want your doctor, nurse and other health workers that you see you have been vaccinated? Q2: Are you worried about visiting your clinic if some staff are not vaccinated? Definite yes 35.0% Probably yes 17.5% Don't mind 25.0% No 22.5% Definite yes 57.5% Probably yes 22.5% Don't mind 17.5% No 2.5% >50% still worry about COVID-19.
Vaccines: outstanding Qs Need for third dose - now agreed in UK - need for boosters? [1] Impact of variants. HIV+ vs HIV children: greater need for protection? Biomarkers for efficacy & thresholds for antibody levels. CD4 cut-off for protective responses: <50, <100, <200? Impact of detectable viral load and threshold (if any)? Duration of efficacy for HIV+ , including third dose? Age: serious COVID in younger HIV+? Vaccines? 1. UK JCVI 1 September 2021. https://i-base.info/qa/17427.
Conclusion Very lucky that vaccine results look similar for people on stable ART with good CD4 counts. We still need data on everyone else. Access: Of >5.6 billion doses globally, less than 2% of population in low income countries are covered. Data on low response groups is just as important in countries with delayed access to vaccines.
Thanks Angelina Namiba. Ben Cromarty Chris Sandford. Christina Antoniadi. Memory Sachikonye. UK-CAB discussion forum.