Vortex Keratopathy: Symptoms, Causes, and Toxic Effects
Vortex keratopathy, also known as cornea verticillata, is characterized by whorl-like corneal epithelial deposits. This condition presents with specific signs, such as bilateral opacities, arborizing lines, and a distinct pattern originating from below the pupil. Common causes include antimalarials, amiodarone, chlorpromazine, and chrysotherapy with gold compounds. Each cause has unique toxic effects on the cornea. Diagnosis involves recognizing the characteristic patterns and associations with medication use. Management typically includes discontinuation of the offending medication.
Uploaded on Apr 16, 2025 | 1 Views
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
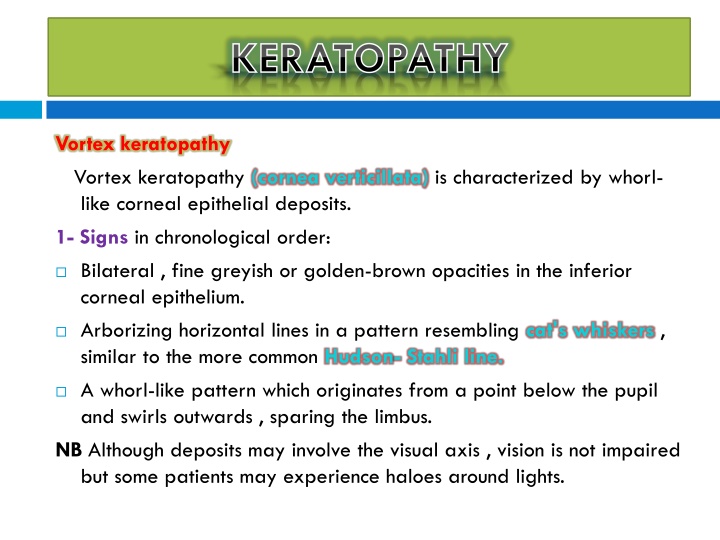
KERATOPATHY Vortex keratopathy Vortex keratopathy (cornea verticillata) is characterized by whorl- like corneal epithelial deposits. 1- Signs in chronological order: Bilateral , fine greyish or golden-brown opacities in the inferior corneal epithelium. Arborizing horizontal lines in a pattern resembling cat's whiskers , similar to the more common Hudson- Stahli line. A whorl-like pattern which originates from a point below the pupil and swirls outwards , sparing the limbus. NB Although deposits may involve the visual axis , vision is not impaired but some patients may experience haloes around lights.
KERATOPATHY KERATOPATHY Vortex keratopathy
KERATOPATHY KERATOPATHY 2- Causes A- Antimalarials (chloroquine and hydroxychloroquine) are common causes. Unlike retinopathy , keratopathy bears no relationship to dosage or duration of treatment. The changes are usually reversible on cessation of therapy , although they may clear despite continued administration. B- Amiodarone. Virtually all patients develop keratopathy which is reversible on discontinuation of medication. In general the higher the dose and the longer the duration of administration the more advanced the corneal deposits. Other toxic effects are anterior subcapsular lens deposits and optic neuropathy.
KERATOPATHY KERATOPATHY Chlorpromazine Chlorpromazine (Largactil) is used as a sedative and to treat psychotic illnesses. Some patients on long-term therapy may develop innocuous , subtle , diffuse , yellowish-brown granular deposits in the endothelium and deep stroma. Other toxic effects are anterior lens capsule deposits and retinopathy. Argyrosis Argyrosis is a discolouration of ocular tissues secondary to silver deposits which may be iatrogenic or from occupational exposure. Keratopathy is characterized by greyish-brown , granular deposits in Descemet membrane. The conjunctiva may also be affected.
KERATOPATHY KERATOPATHY chlorpromazine argyrosis
KERATOPATHY KERATOPATHY Chrysiasis Chrysiasis is the deposition of gold in living tissue , occurring after prolonged administration of gold , usually in the treatment of rheumatoid arthritis. Virtually all patients on continuous chrysotherapy who have received a total dose of gold compound exceeding 1000 mg develop corneal deposits. Corneal chrysiasis is characterized by dust -like or glittering purple granules throughout the corneal stroma , more concentrated in the deep layers and the periphery. These findings are innocuous and therefore not an indication for cessation of therapy. Other toxic effects are innocuous lens deposits and occasionally marginal keratitis.
KERATOPATHY KERATOPATHY chrysiasis (left), marginal keratitis (right)
CATARACT Steroids Steroids , both systemic and topical , are cataractogenic. The lens opacities are initially posterior subcapsular and later the anterior subcapsular region becomes affected. The relationship between weekly systemic dose , duration of administration , total dose and cataract formation is unclear. It is thought that patients on less than I0 mg prednisolone (or equivalent), or treated for less than 4 years may be immune. Although it is believed that children may be more susceptible to the cataractogenic effects of systemic steroids , individual (genetic) susceptibility may also be of relevance.
CATARACT It has therefore been suggested that the concept of a safe dose be abandoned. Patients who develop lens changes should have their dosage reduced to a minimum consistent with control of the underlying disease , and if possible be considered for alternate day therapy. Early opacities may regress if therapy is discontinued; alternatively progression may occur despite withdrawal and warrant surgical intervention.
CATARACT Steroid-induced posterior subcapsular cataract
CATARACT Other drugs 1- Chlorpromazine may cause the deposition of innocuous , fine , stellate , yellowish-brown granules on the anterior lens capsule within the pupillary area. 2- Busulphan (Myleran), used in the treatment of chronic myeloid leukaemia , may occasionally cause lens opacities. 3- Gold, used in the treatment of rheumatoid arthritis, causes innocuous anterior capsular deposits in about 50% of patients on treatment for longer than 3 years. 4- Allopurinol, used in the treatment of hyperuricaemia and chronic gout, increases the risk of cataract formation in elderly patients, if the cumulative dose exceeds 400g or duration of administration exceeds 3 years.
CATARACT Anterior capsular deposits due to chlorpromazine
UVEITIS Rifabutin Rifabutin is used mainly in the management and prophylaxis of Mycobacterium avium complex infections in AIDS patients with low CD4 counts. It is also used to treat tuberculosis with other drugs in immunocompetent patients. 1- Acute anterior uveitis is typically unilateral and frequently associated with hypopyon; associated vitritis may be mistaken for endophthalmitis. 2- Treatment involves withdrawal of the drug or reduction of dose. NB Drugs that inhibit metabolism of rifabutin through cytochrome p- 450 pathway, such as clarithromycin and fluconazole , will increase the risk of uveitis.
UVEITIS Cidofovir Cidofovir is used in the management of cytomegalovirus retinitis in AIDS patients. 1- Acute anterior uveitis with few cells but a marked fibrinous exudate may develop following several intravenous infusions. Vitritis is common and hypopyon may occur with long term administration. 2- Treatment with topical steroids and mydriatics is usually successful , avoiding the need to discontinue therapy. NB Intravitreal injection of cidofovir should be used with caution because it carries a high risk of hypotony.
RETINOPATHY Antimalarials Drugs Chloroqine (Nivaquine, Avlocor) and hydroxychloroquine (Plaquenil) are quinolone antimalarial drugs used in the prophylaxis and treatment of malaria as well as in the treatment of certain rheumatological disorders (e.g. rheumatoid arthritis, juvenile idiopathic arthritis , systemic lupus erythematosus). The use of chloroquine has also been advocated in the treatment of calcium abnormalities associated with sarcoidosis.
RETINOPATHY Antimalarials are excreted from the body very slowly and are melanotropic drugs that become concentrated in melanin-containing structures of the eye such as the retinal pigment epithelium (RPE) and choroid.
RETINOPATHY 1- Chloroquine Retinotoxicity is related to the total cumulative dose. The normal daily dose is 250 mg; a cumulative dose of less than 100 g or treatment duration under 1 year is rarely associated with retinal damage. The risk of toxicity increases significantly when the cumulative dose exceeds 300g (i.e. 250mg daily for 3 years). However , there have been reports of patients receiving cumulative doses exceeding 1000 g who did not develop retinotoxicity. If possible, chloroquine should be used only if other agents are ineffective.
RETINOPATHY 2- Hydroxychloroquine Is much safer than chloroquine and if the daily dose does not exceed 400 mg the risk of retinotoxicity is negligible. Physicians should therefore be encouraged to use hydroxychloroquine instead of chloroquine whenever possible. The risk of toxicity is increased if a daily dose is over 6.5mg/kg is administered for longer than 5 years, although even then the risk is still very small.
RETINOPATHY Retinopathy Chloroquine retinopathy can be divided into the following stages: 1- Premaculopathy Is characterized by normal visual acuity and a scotoma to a red target located between 4 and 9 from fixation. Amsler grid testing may also show a defect. If the drug is discontinued, visual function usually returns to normal.
RETINOPATHY 2- Early maculopathy Is the next stage, if treatment is not discontinued. It is characterized by a modest reduction of visual acuity (6/9- 6/12). Fundus examination shows a subtle 'bull's eye' macular lesion characterized by central foveolar island of pigment surrounded by a depigmented zone of RPE atrophy which is itself encircled by a hyperpigmented ring. The lesion may be more obvious on FA than ophthalmoscopy because the RPE atrophy gives rise to a RPE 'window' defect. This stage may progress even if the drug is stopped.
RETINOPATHY Early maculopathy
RETINOPATHY 3- Moderate maculopathy is characterized by moderate reduction of visual acuity (6/1 8-6/24) and an obvious 'bull's eye' macular lesion. 4- Severe maculopathy is characterized by marked reduction of visual acuity (6/36-6/60) with widespread RPE atrophy surrounding the fovea. 5- End-stage maculopathy is characterized by severe reduction of visual acuity and marked atrophy of the RPE with unmasking of the larger choroidal blood vessels. The retinal arterioles may also become attenuated and pigment clumps develop in the peripheral retina.
RETINOPATHY Moderate maculopathy Severe maculopathy
RETINOPATHY End-stage maculopathy
RETINOPATHY Screening Screening of patients on hydroxychloroquine is unnecessary although some have recommended annual screening if the patient has been on medication for over 6 years. In clinical practice chloroquine can also be given safely to patients without the need for repetitive routine examinations by ophthalmologists or the use of complicated tests. Recording of visual acuity and ophthalmoscopy by the prescribing doctor is all that is required. The patient can be given an Amsler grid to use once a week.
RETINOPATHY If symptoms occur or an abnormality is found, then the opinion of an ophthalmologist should be sought. The ophthalmologist can , if necessary, perform more sophisticated tests such as visual fields, macular threshold, colour vision testing, contrast sensitivity , FA and electro-oculography. Recent reports suggest that multifocal electroretinography may be useful in detecting early toxicity.
OPTIC NEUROPATHY Ethambutol Ethambutol (Myambutol , Mynah) is used in combination with isoniazid and rifampicin in the treatment of tuberculosis. Ocular toxic effects include optic neuritis , colour vision abnormalities and visual field defects. Toxicity is dose and duration dependent , the incidence is up to 6% at a daily dose of 25 mg/kg and rare with a daily dose not exceeding 15 mg/kg. Toxicity typically occurs between 3 and 6 months of starting treatment. NB Isoniazid may also rarely cause toxic optic neuropathy , particularly in combination with ethambutol.
OPTIC NEUROPATHY 1- Presentation of optic neuritis is with abrupt visual impairment. 2- Signs include normal or slightly swollen optic discs with splinter- shaped haemorrhages. 3- Visual field defects usually consist of central or centrocaecal scotomas although bitemporal or peripheral constriction may occur. 4- Prognosis is good following cessation of treatment although recovery may take up to 12 months. A minority of patients develop permanent visual impairment as a result of optic atrophy. 5- Screening should be every 4 weeks when the dose is more than 15 mg/kg and every 3-6 months for lower doses. The drug should be stopped immediately if symptoms develop.
OPTIC NEUROPATHY Vigabatrin Vigabatrin is used as a second-line antiepileptic drug for the treatment of uncontrolled complex partial seizures and as first-line monotherapy for infantile spasms (West syndrome). Some patients develop bilateral concentric or binasal visual field defects , often asymptomatic , months or years after starting treatment. The defects persist if treatment is stopped but do not progress if medication is continued. This suggests that toxicity is idiosyncratic rather than a dose-related effect.
OPTIC NEUROPATHY Ophthalmoscopy is usually normal although a small percentage of patients may show a variety of changes including nasal (inverse) optic disc atrophy , arteriolar narrowing , abnormal macular reflexes and surface wrinkling. Baseline visual field examination is recommended prior to starting treatment. Reassessment is made thereafter every 11 months for 3 years and then annually if no abnormality is detected.