Wessex Cancer Alliance: Cancer Support Worker Case for Change
This report by Catherine Neck, Clinical Programme Services Lead, delves into connecting health and care for cancer patients. Exploring the gaps in support services, the report provides a compelling case for change in cancer care delivery. By emphasizing the importance of collaboration across health sectors, it highlights opportunities for enhancing patient outcomes and long-term well-being. Join the discussion on transforming cancer support services today.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Wessex Cancer Alliance: Cancer Support Worker Case for Change Report Catherine Neck, Clinical Programme Services Lead: Cancer and Long-Term Conditions Joining the dots across health and care Joining the dots across health and care
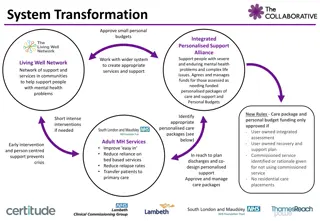
Background and Context The NHS Long Term Plan says the NHS service model will change so People will get more control over their own health, and more personalised care when they need it. This means that: By 2021, where appropriate every person diagnosed with cancer will have access to personalised care, including needs assessment, a care plan and health and wellbeing information and support. By 2023, stratified, follow-up pathways for people who are worried their cancer may have recurred. These will be in place for all clinically appropriate cancers. Across Wessex there was a need to build a case for sustainably commissioning the expected elements of personalised care for cancer and PSFU and have a specific focus on the Cancer Support Worker roles Joining the dots across health and care
Methodology Currently CSW s are based in secondary care and resource not sufficient to support all cancer patients Mostly short-term funded roles Sustainable funding is required in order to fully realise the benefits the role offers and build a solid foundation for future development What we did: Used the CSW role in providing personalised care and facilitating PSFU Outpatient release data for breast, colorectal and prostate was used with application of financial reference costs to create a cost-effective case for sustaining the CSW roles Produce a case for change report related to the CSW roles across Wessex Joining the dots across health and care
Benefits Realisation Outcome Benefit Output Increased patient confidence to interact appropriately and in a timely way with Reduced requirements for complex CNS contacts during and Improved patient outcomes cancer team following treatment and experience Patients prepared for outcomes of cancer treatment resulting in earlier Reduced outpatient appointments over follow-up period e.g. 5 years recognition of treatment effects and signs of recurrence Reduced demand on inpatient, outpatient and GP services Personalised Care interventions offered throughout the patient pathway. Early identification of patient needs - referrals to community Includes practical, emotional and social support services/ social prescribing Support for carers Reduction in travel (time/costs), time off work etc Patients feel more engaged and in control of their care Attendance only at necessary outpatient appointments Clinician and CNS time saving Increased capacity to provide complex diagnostic and treatment Efficient working practices interventions Cost effective workforce redesign Increase in overall workforce to meet demand but at appropriate skill mix levels Improved Trust cancer performance Timely outpatient appointments available to appropriate patients i.e. new and Outpatient appointment complex patients reduction Increase in outpatient capacity Fewer overbooked clinics and reduction in associated costs of waiting list initiative clinics Joining the dots across health and care
Options Appraisal Option 1: Do Nothing Option 2: Gold Standard Service Benefits Benefits Realisation Risks Benefits Effective and efficient Benefits Realisation Patient needs are identified early and acted Risks Significant financial investment which exceeds the amount identified by Benefits currently Patients are not provided with holistic support Requires no upon in timely manner resulting in fewer outpatient cost release delivery of offered by the CSW role during their cancer treatment new or treatment effects personalised care will be maintained until additional Source of financial investment is unknown interventions to all There is no early identification of adverse their fixed term investment Enables self-management and facilitates patients diagnosed treatment effects Outpatient appointment release does not yield cashable savings contracts end reduction in follow-up with cancer at XXX Increasing future costs associated with Current block system for NHS funding Trust Improved patient health outcomes increasing prevalence of cancer, high numbers Requires system-wide discussion in order to fully realise benefits of patients over 65 with cancer and adverse Reduced morbidity effects that result from cancer and its treatment Training and HR requirements to provide appropriate support to CSWs Reduced carer burden Improved patient satisfaction/ experience Reduced appointment burden in acute and primary care Clinician and clinical nurse specialist time is released to provide complex interventions Improved Trust cancer performance Improved patient care across primary and secondary care due to improved communication and links to social prescribing link workers Joining the dots across health and care
Option 3: Preferred Approach Secure existing CSW resource from reduction in outpatient appointments, and invest in some additional posts to ensure roll out of PSFU to identified cancer sites. CSW resource to be networked wherever possible to provide cross-cover and ensure maximum reach. This would provide the platform for having a dedicated CSW resource in secondary care, and then allow further development in cross boundary support roles to meet the Wessex Cancer Alliance LTP ambitions. This option provides all the identified benefits of the CSW role to be offered to significant numbers of people with cancer, and is cost-effective when balanced against the outpatient appointment release. Joining the dots across health and care
Option 3: Preferred Approach Benefits Benefits Realisation Risks Patient needs are identified early and acted upon in timely Significant financial investment required. Source of financial Delivery of manner resulting in fewer treatment effects investment is unknown. personalised care interventions to the Enables self-management and facilitates reduction in Current block system for NHS funding majority of patients follow-up Requires system-wide discussion in order to fully realise benefits diagnosed with cancer Improved patient health outcomes at XXX Trust Training and HR requirements to provide appropriate support to Reduced morbidity CSWs Reduced carer burden Improved patient satisfaction/ experience Reduced appointment burden in acute and primary care Clinician and clinical nurse specialist time is released to provide complex interventions Improved Trust cancer performance Improved patient care across primary and secondary care due to improved communication and links to social prescribing link workers Joining the dots across health and care
Resource Requirement Provider Recurrent Costs Fixed Term Costs 2.8 WTE CSW: 83,306 1 WTE B7 PM: 51,205 Hampshire Hospitals NHS FT 3 WTE CSW: 89,256 N/A Portsmouth Hospitals University NHS Trust 5.8 WTE CSW: 172,562 N/A University Hospitals Dorset NHS FT 0.4 WTE B8A PM: 23,366 Equipment Costs: 8,865 Total: 36,831 4.2 WTE CSW: 124,958 University Hospitals Southampton NHS FT No resource requirement identified by the Trust Dorset County Hospital NHS FT No information submitted by the Trust Isle of Wight NHS Trust Joining the dots across health and care
Outpatient Release Finance Data Calculation of potential total number of Breast, Colorectal and Prostate appointments released was made using the National Cancer Programme Outpatient Appointment Estimator (OPA) tool Calculation of potential Provider cost reduction was based on national 2017/18 reference costs in the absence of Provider specific tariffs The OPA reduction data including provider costs for each of the 4 Trusts who submitted data in the Cost Investment section is detailed below: Provider Potential Year 1 reduction Potential Year 0 7 reduction Hampshire Hospitals NHS FT 1,029 113,533 14,808 1,633,816 Portsmouth Hospitals University NHS Trust 845 93,232 7,048 777,629 University Hospitals Dorset NHS FT 1,218 134,386 16,008 1,766,216 University Hospitals Southampton NHS FT 981 108,237 7,383 814,591 Joining the dots across health and care
Summary Costs Provider Investment required Outpatient Provider Cost Reduction (Y 1) Outpatient Provider Cost Reduction (Y 0-7) 134,511 113,533 1,633,816 Hampshire Hospitals NHS FT Portsmouth Hospitals University NHS Trust 89,256 93,232 777,629 University Hospitals Dorset NHS FT 172,562 134,386 1,766,216 University Hospitals Southampton NHS FT 161,789 108,237 814,591 Joining the dots across health and care
Key Points and Suggested Next Steps If business cases are to be submitted to commissioners, important to consider the following: Commissioners commission services and not new roles Important to involve commissioners at the earliest possible stage to align with commissioning priorities New development of ICSs will alter commissioning landscape significantly Next Steps: Providers to use and adapt the contents of the report to populate individual business cases Each provider will have a different approach to business cases, therefore a local approach is important The WCA Business Case Guide produced by SCW is available as a supporting resource Joining the dots across health and care
contact@scwcsu.nhs.uk | scwcsu.nhs.uk | @NHSscw Joining the dots across health and care