Acute Inflammation Process
Inflammation is a protective response to cell injury, aiming to eliminate the cause and initiate repair. Acute inflammation is a short-term process triggered by various stimuli like infection, trauma, and tissue death. It involves cardinal signs such as redness, pain, heat, swelling, and loss of function. Vascular changes lead to increased blood flow and leukocyte accumulation, while cellular events activate leukocytes to combat infections and remove damaged tissue.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
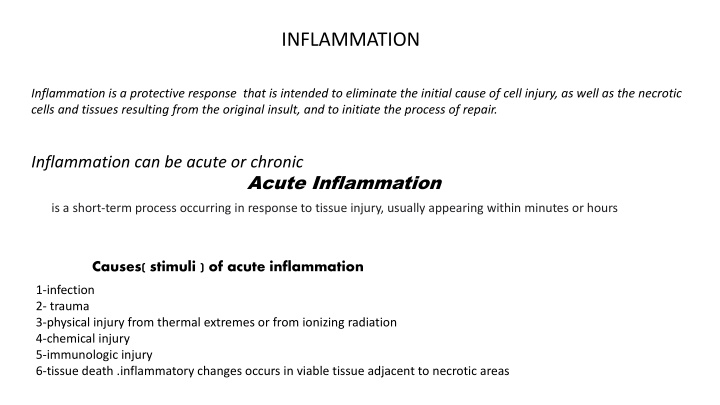
INFLAMMATION Inflammation is a protective response that is intended to eliminate the initial cause of cell injury, as well as the necrotic cells and tissues resulting from the original insult, and to initiate the process of repair. Inflammation can be acute or chronic Acute Inflammation is a short-term process occurring in response to tissue injury, usually appearing within minutes or hours Causes( stimuli ) of acute inflammation 1-infection 2- trauma 3-physical injury from thermal extremes or from ionizing radiation 4-chemical injury 5-immunologic injury 6-tissue death .inflammatory changes occurs in viable tissue adjacent to necrotic areas
Cardinals sign 1-rubor ( redness caused by dilation of vessels) 2-dolor (pain due to increased pressure exerted by the accumulation of interstitial fluid and to mediators such as bradykinin) 3-calor (heat caused by increased blood flow) 4-tumor ( swelling due to an extravascular accumulation of fluid 5-functiolaesa(loss of function)
Component of inflammation: 1- vascular changes 2- cellular events 1- vascular changes: blood vessels changes are initiated rapidly A- After transient vasoconstriction (lasting only for seconds), arteriolar vasodilation occurs, resulting in locally increased blood flow and engorgement of the down-stream capillary beds B- The microvasculature becomes more permeable, and protein-rich fluid moves into the extravascular tissues. C- This causes the red cells in the flowing blood to become more concentrated, Lead to stasis develops, leukocytes (principally neutrophils) begin to accumulate
Cellular event: an important function of the inflammatory response is to deliver leukocytes to the site of injury and to activate them. Leukocytes ingest offending agents, kill bacteria and other microbes, and eliminate necrotic tissue and foreign substances. A- Leukocyte Recruitment 1) margination and rolling along the vessel wall; (2) firm adhesion to the endothelium; (3) transmigration between endothelial cells; and (4) migration in interstitial tissues toward a chemotactic stimulus B- Chemotaxis. After extravasating from the blood, leukocytes move toward sites of infection or injury along a chemical gradient by a process called chemotaxis. Both exogenous and endogenous substances can be chemotactic for leukocytes, including the following: Bacterial products, particularly peptides with N-formyl methionine termini Cytokines, especially those of the chemokine family Components of the complement system, particularly C5 Products of the lipoxygenase pathway of arachidonic acid (AA) metabolism, particularly leukotriene B4 (LTB4)
C-Leukocyte Activation Once leukocytes have been recruited to the site of infection or tissue necrosis, they must be activated to perform their functions. Stimuli for activation include microbes, products of necrotic cells, and several mediators D- phagocytosis : Phagocytosis consists of three steps (1) recognition and attachment of the particle to the ingesting leukocyte; (2) engulfment, with subsequent formation of a phagocytic vacuole; and (3) killing and degradation of the ingested material E- intracellular microbial killing : Is mediated within phagocytic cells by oxygen dependent ( superoxide ,hydrogen peroxide ,hydroxyl radical and and oxygen independent mechanism (lysozyme ,lactoferrin ) The type of emigrating leukocyte varies with the age of the inflammatory response and with the type of stimulus. In most forms of acute inflammation, neutrophils predominate in the inflammatory infiltrate during the first 6 to 24 hours and are replaced by monocytes in 24 to 48 hours:
Type of inflammatory cells : 1- neutrophil : are the most prominent inflammatory cells in foci of acute inflammation during the first 24-hours.important cause of neutrophilia bacterial infection and infarction After 2-3 days neutrophil are replaced mainly by 2- monocytes-macrophages :are capable of engulfing larger particle ,long lived and capable of dividing and proliferating within the inflamed tissue Important cause of monocytosis .TB, Typhus ,brucellosis 3- lymphocyte : most prominent in many viral infection 4- eosinophils: are prominent in allergic reaction and parasitic infection 5- mast cells and basophils :
Outcome of acute inflammation 1- Resolution: Regeneration and repair. When the injury is limited 2- tissue destruction and persistent acute inflammation Abscess; this is a cavity filled with pus( neutrophils ,monocytes and liquefied cellular debris),Its often walled off by fibrous tissue and is relatively inaccessible to the circulation),Its usually caused by bacterial infections ,often by staphylococci Ulcer :this is loss of surface epithelium ,this can be caused by acute inflammation of epithelial surface ( e.g peptic ulcer and ulcer of the skin ) Fistula: this is an abnormal communication between two organ or between an organ and a surface
3- Chronic inflammation may follow acute inflammation if the offending agent is not removed, or it may be present from the onset of injury (e.g., in viral infections or immune responses to self-antigens). This is marked by the replacement of neutrophils and monocyte with lymphocyte plasma cells and macrophage Tts often includes proliferation of fibroblast and new vessels with resultant scarring and distortion of architecture 4-Scar: this is the final result of tissue destruction with resultant distortion of structure and in some cases altered function
CHRONIC INFLAMMATION Chronic inflammation is inflammation of prolonged duration (weeks to years) in which continuing inflammation, tissue injury, and healing, often by fibrosis, proceed simultaneously. chronic inflammation is characterized by a different set of reactions : Infiltration with mononuclear cells, including macrophages, lymphocytes, and plasma cells Tissue destruction, largely induced by the products of the inflammatory cells Repair, involving new vessel proliferation (angiogenesis) and fibrosis Chronic inflammation may arise in the following 1- Persistent infections by microbes that are difficult to eradicate. These include Mycobacterium tuberculosis, Treponema pallidum (the causative organism of syphilis), and certain viruses and fungi, 2-Immune-mediated inflammatory diseases (hypersensitivity diseases). 3-Prolonged exposure to potentially toxic agents. Examples are non degradable exogenous materials such as inhaled particulate silica,
Granulomatous Inflammation: Granulomatous inflammation is a distinctive pattern ofchronic inflammation characterized by aggregates of activated macrophages with scattered lymphocytes. . Tuberculosis is the prototype of a granulomatous disease , T .pallidum and fungi is another cause of granulomatous disease they develop in response to relatively inert foreign bodies (e.g., suture or splinter), forming so-called foreign body granulomas. granuloma formation does not always lead to eradication of the causal agent, which is frequently resistant to killing or degradation, and granulomatous inflammation with subsequent fibrosis may even be the major cause of organ dysfunction in some diseases, such as tuberculosis.
SYSTEMIC EFFECTS OFINFLAMMATION 1- fever 2-leukocytosis The leukocyte count usually climbs to 15,000 to 20,000 cells/mL, 3-Other manifestations of the acute-phase response include increased heart rate and blood pressure; decreased sweating, mainly as a result of redirection of blood flow from cutaneous to deep vascular beds, to minimize heat loss through the skin; and rigors (shivering), chills (perception of being cold as the hypothalamus resets the body temperature), anorexia, and malaise, probably secondary to the actions of cytokineson brain cells.
Q- talk briefly about the following 1- definition of inflammation and important cause of acute inflammation 2- out come of acute inflammation 3- defined abscess 4- took briefly disease associated with arise of chronic inflammation 5- took briefly systemic effect of inflammation