Acute Renal Failure in Pediatrics
Explore the definition, etio-pathogenesis, lab findings, and diagnostic approaches for acute renal failure in pediatric patients as outlined by Dr. Virendra Kumar Gupta, MD. Learn about the various causes, clinical presentations, and management strategies associated with this condition.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
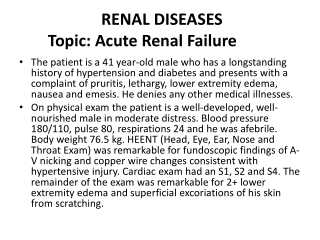
Acute Renal failure Dr. Virendra Kumar Gupta MD Pediatrics Fellowship In pediatric Gastroentero-Hepatology & Liver Transplantation Assistant Professor Department Of pediatrics NIMS Medical College & Hospital , Jaipur
DEFINITION Aclinical syndrome in which a sudden deterioration in renal function results in the inability of the kidneys to maintain fluid and electrolyte homeostasis. Also k/a Acute renalinsufficiency/ Acute Kidney Injury 2-3%of children admitted to pediatrictertiary care centres 8%of infants in neonatal ICU.
Etio-Pathogenesis INTRINSIC RENAL Glomerulonephritis Postinfectious poststreptococcal PRERENAL Dehydration POSTRENAL Posterior urethral valves Ureteropelvic junction obstruction Hemorrhage Lupus erythematosus Henoch-Sch nlein purpura Membranoproliferative Ureterovesicular junction obstruction Ureterocele Tumor Sepsis Hypoalbuminemia Cardiac failure Anti-glomerular basement membrane Urolithiasis Hemorrhagic cystitis Neurogenic bladder Hemolytic-uremic syndrome Acute tubular necrosis Cortical necrosis Renal vein thrombosis Rhabdomyolysis Acute interstitial nephritis Tumor infiltration
LAB FINDINGS Anemia : Dilutional or hemolytic eg. SLE, renal vein thrombosis, HUS Leukopenia : SLE, sepsis Thrombocytopenia :SLE, renal vein thrombosis, sepsis, HUS Hyponatremia : dilutional Metabolic acidosis Elevated BUN, creatinine, uric acid, potassium, and phosphate (diminished renal function); and (hyperphosphatemia). hypocalcemia
Decreased serum C3 level : -Postinfectious glomerulonephritis, SLE, MPGN Antibodies : Streptococcal : PSGN Nuclear : SLE Neutrophil cytoplasmic : Wegener granulomatosis, microscopic polyarteritis GBM :Goodpasture disease - - - -
CXR : Cardiomegaly, overload) or pleural effusions. congestion (fluid pulmonary Renal USG : Hydronephrosis /hydroureter, renal disease. Nephromegaly- s/o intrinsic Renal biopsy : who do not have clearly defined prerenal or postrenal ARF
Other biomarkers: -changes in plasma neutrophil associated lipocalin (NGAL) and cystatin C levels gelatinase- -urinary changes in NGAL, interleukin- 18 (IL-18), and kidney injury molecule-1 (KIM-1).
Management Catheterization - in newborn with suspected posterior ureteral valves & nonambulatory older children. Fluid Bolus : If there is no evidence of volume overload or cardiac failure, intravenous administration of isotonic saline, 20 mL/kg over 30 min hypovolemic patients generally void within 2 hr after bolus; failure points to intrinsic or postrenal ARF. Hypotension due to sepsis - vigorous fluid resuscitation f/b continuous infusion of norepinephrine.
Diuretic therapy : only after the adequate hydration. Mannitol (0.5 g/kg) and furosemide (2-4 mg/kg) - as a single IV dose Bumetanide (0.1 mg/kg)- an alternative to furosemide. If urine output is not improved - continuous diuretic infusion may be considered. Consider Dopamine (2-3 g/kg/min) in conjunction with diuretic therapy. There is little evidence that diuretics or dopamine can prevent ARF or hasten recovery.
Hyperkalemia : Sr K >6 mEq/L cardiac arrhythmia, cardiac arrest, and death Earliest ECG change - peaked T waves f/b widening of the QRS intervals, ST segment depression, ventricular arrhythmias, and cardiac arrest. Exogenous sources of K : dietary, intravenous fluids, total parenteral nutrition) should be eliminated. Sodium polystyrene sulfonate resin (Kayexalate) : (1 g/kg) - orally or by retention enema when Sr K>6 mEq/L - exchanges sodium for potassium - can take several hours to take effect. A single dose of 1 g/kg can lower the sr K level by about 1 mEq/L. - Resin therapy may be repeated every 2 hr, the frequency being limited primarily by the risk of sodium overload.
If Sr K >7 mEq/L : emergency measures in addition to Kayexalate Calcium gluconate 10% solution : 1.0 mL/kg IV, over 3-5 min Sodium bicarbonate :1-2 mEq/kg IV, over 5-10 min Regular insulin : 0.1 U/kg, with glucose 50% solution, 1 mL/kg, over 1 hr
Metabolic acidosis: Mild is common in ARF - rarely requires treatment. Severe (arterial pH < 7.15; serum bicarbonate < 8 mEq/L) or contributes to hyperkalemia it should be corrected.
Hypocalcemia : -Primarily treated by lowering the serum phosphorus level -Calcium should not be given IV except in cases of tetany, to avoid deposition of calcium salts into tissues. -Follow a low-phosphorus diet,
- Hyponatremia : - Most commonly a dilutional - Must be corrected by fluid restriction. - Hypertonic (3%) saline - limited to symptomatic hyponatremia (seizures, lethargy) or those with a serum sodium level <120 mEq/L.
GI bleeding : Because of uremic platelet dysfunction, increased stress, and heparin exposure in hemodialysis. Oral or intravenous H2 blocker- Ranitidine.
Hypertension : Common in ARF patients with acute HUS. glomerulonephritis or Salt and water restriction Diuretics Isradipine (0.05-0.15 mg/kg/dose) amlodipine, 0.1-0.6 mg/kg/24 hr qd or divided bid propranolol, 0.5-8 mg/kg/24 hr divided bid or tid labetalol, 4-40 mg/kg/24 hr divided bid or tid severe symptomatic hypertension - continuous sodium nitroprusside or esmolol infusions of
Neurologic symptoms : and confusion Headache, (encephalopathy). seizures, lethargy, Potential etiologic factors - hyponatremia, hypocalcemia, hypertension, cerebral hemorrhage, cerebral vasculitis, and the uremic state. Diazepam - most effective in controlling seizures Treat the underlying cause.
Anemia of ARF : Generally mild Packed red blood cells if Hb < 7 g/dl Slow (4-6 hr) transfusion with packed red diminishes the risk of hypervolemia. blood cells (10 ml/kg)
Nutrition : In most cases, sodium, potassium, and phosphorus should be restricted. Protein restricted & caloric intake maximised to minimize the accumulation of nitrogenous wastes. Critically ill patients with ARF - parenteral essential amino acids given
Protein : enough protein for growth - limiting high protein intake. Protein needs increase on dialysis. Foods with protein include Eggs Milk cheese Chicken Fish Red meats beans yogurt Cottage cheese
Sodium : Depend on stage of their kidney disease,their age, and sometimes other factors. Foods high in sodium include Canned foods Some frozen foods Most processed foods Some snack foods, such as chips
Potassium. Low-potassium High-potassium - apples cranberries strawberries blueberries raspberries pineapple cabbage boiled cauliflower mustard greens - oranges melons apricots bananas potatoes tomatoes sweet potatoes cooked spinach
Health care team Pediatrician Nephrologist Dialysis nurse Transplant coordinator Transplant surgeon Social worker Financial counselor Dietitian
DIALYSIS : Indications Volume overload with evidence of hypertension and/or pulmonary edema refractory to diuretic therapy Persistent hyperkalemia Severe metabolic acidosis unresponsive to medical management Neurologic symptoms (altered mental status, seizures) Blood urea nitrogen >100-150 mg/dL (or lower if rapidly rising) Calcium:phosphorus imbalance, with hypocalcemic tetany