Anal Cancer Screening: What Now?
In this presentation by Dr. Susan Cu-Uvin, explore the relationship between HIV and anal cancer, screening recommendations, and treatment options. Case studies highlight key considerations for individuals with HIV. Stay informed on the latest insights in anal cancer prevention and care.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Anal Cancer Screening: What Now? Susan Cu-Uvin, MD Professor of Obstetrics, Gynecology, and Medicine Brown University Providence, Rhode Island
Financial Relationships With Ineligible Companies (Formerly Described as Commercial Interests by the ACCME) Within the Last 2 Years: Dr Cu-Uvin has no relationships with ineligible companies to disclose. (12/05/22) $$$Please confirm that your financial relationships are still current or update as necessary$$$ Slide 2 of 18
Learning Objectives After attending this presentation, learners will be able to: Describe the impact of the HIV epidemic on the incidence rates and progression to anal cancer and the risk factors among people with HIV (PWH) in the United States List the recommendations for anal cancer screening and their limitations among PWH Describe the recommended treatment for anal high grade squamous epithelial lesions to prevent anal cancer Slide 3 of 18
Case 1: 45 y.o. PWH and identifies as MSM CD4 count of 200 PVL undetectable on cART No diagnosis of sexually transmitted infection in the past 2 years He says he always uses a condom with sexual activity Slide 4 of 18
Case 1: ARS Question 1 His risk of developing anal cancer compared to the general population is: A. Decreased because he is on cART with an undetectable PVL B. Increased despite being on cART with an undetectable PVL C. Similar to the general population Slide 5 of 18
Case 1: The incidence of anal cancer among MSM with HIV is estimated to be 89 per 100,000 person-years. Among women with HIV, the incidence ranges from 18.6 to 35.6 per 100,000 person years. In comparison, the incidence of anal cancer in the general population is 1.6 per 100,000 person-years. In a meta-analysis, the risk of progression from anal HSIL to cancer was estimated to be 265 per 100,000 person-years among MSM with HIV. Danish data show a 5-year incidence of progression to cancer of 14.1% among persons with HIV with anal intraepithelial neoplasia. Slide 6 of 18
Case 2: 35 y.o. transgender female with HIV who is asymptomatic CD4 count of 150 PVL undetectable on cART She wants to know if she should be screened for anal cancer Slide 7 of 18
Case 2: ARS Question 2 What screening would you recommend? A. Anal Pap test with HPV co-testing B. High resolution anoscopy and biopsy C. HPV testing only since HPV 16/18 are the most frequent cause of anal neoplasia/cancer Slide 8 of 18
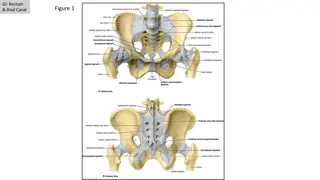
Recommendations for Anal Cancer Screening: For MSM and transgender women age 35 and older; Women with HIV (WWH) and all other PWH age 45 and older: Anal Cytology Testing Only If screening with anal cytology only, PWH in whom screening has been initiated should have an anal cytology testing every 12 months (BIII). If the results of three consecutive anal cytology tests are normal, follow-up anal cytology tests should be every 3 years (BIII). Persons with any abnormal cytology (>ASC-US) should be referred for HRA (BIII). Slide 9 of 18
Recommendations for Anal Cancer Screening: Normal Anal Cytology with HPV Co-Testing If co-testing with anal cytology and anal high-risk HPV testing is performed, then persons who co- test negative (i.e., a normal anal cytology and negative HPV test) can have their next anal cancer screening in 3 years (BIII). If the initial anal high risk HPV testing results identify HPV16 or HPV16/18, referral to HRA is recommended (regardless of cytology result) (BIII). If anal cytology is normal and the high-risk HPV testing is positive, but the genotype-specific testing for HPV16 or HPV16/18 is negative, then repeat co-testing in one year is recommended. If either of the co-tests at one year is abnormal (i.e., abnormal anal cytology or positive high-risk HPV), referral to HRA is recommended (BIII). If the initial high-risk HPV test is positive but that test does not specifically identify HPV 16 or 18 genotypes, then repeat cytology and HPV co-testing is recommended in 6 months. Referral for HRA is recommended if either test is positive at 6 months (BIII). Slide 10 of 18
Recommendations for Anal Cancer Screening: Abnormal Anal Cytology and HPV Co-testing If ASC-US on anal cytology, and high-risk HPV testing is negative, then repeat co-testing (cytology and high-risk HPV testing) in 1 year is recommended. If either of the co-tests at one year is abnormal (i.e., abnormal anal cytology or positive high-risk HPV test) referral to HRA is recommended (BIII). If ASC-US on cytology and high-risk HPV testing is positive, then referral for HRA is recommended. For LSIL, ASC-H or HSIL on anal cytology, referral to HRA is recommended (regardless of high- risk HPV test result) (BIII). Within the above guidelines, if the number of people who need HRA is exceeding HRA capacity, providers may consider prioritizing for referral to HRA: older PWH; those known to be living with HIV for the longest period of time; those with higher grade of cytologic abnormality; those with HPV 16 or 18 on HPV testing; and current smokers. All other PWH meeting the criteria specified above should be referred for HRA as soon as feasible (BIII). Slide 11 of 18
Case 3: 50 y.o. MSM with HIV, diagnosed with anal high grade squamous epithelial lesion by HRA and biopsy. Slide 12 of 18
Case 3: ARS Question 3 What treatment would you recommend? A. Observation only, repeat HRA every 6 months B. Surgery C. Radiation D. Hyfrecation (office-based electrocautery/ablation) Slide 13 of 18
Anchor Study Slide 14 of 18
ANCHOR Study Slide 15 of 18
Changes Formatted title, financial disclosure, and learning objectives slides. Slide 2: Removed UpToDate as this is not an ineligible company Slide 6: Standardized font color usage (eg, inclusion of per 100,000 in red). Slide 13: Changed office based to office-based . Slides 5, 8, 13: Formatted ARS Questions Slide 17 of 18
Queries Slide 2: Please confirm that your financial relationships are still current and update as necessary. Slides 9-11: Please add citations to the slides Are 15 slides enough content for 30 minutes? Slide 18 of 18