Anticoagulants in Coagulation Disorders
Explore the mechanisms and classifications of anticoagulants used in the treatment of coagulation disorders. Learn about heparin, low-molecular-weight heparin, and fondaparinux, their mechanisms of action, monitoring, and effects. Discover how these medications provide anticoagulation and their importance in managing blood clotting disorders.
Uploaded on | 1 Views
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Drugs Used in Coagulation Disorders Presented by Dr. Sasan Zaeri PharmD, PhD
ANTICOAGULANTS Classification Three major types of anticoagulants: Heparin and related products must be used parenterally Direct thrombin inhibitors used parenterally Orally active coumarin derivatives (e.g. warfarin) 6
ANTICOAGULANTS Heparin A large sulfated polysaccharide polymer obtained from animal sources Highly acidic and can be neutralized by basic molecules Protamine sulfate (heparin antidote) Given IV or SC to avoid the risk of hematoma associated with IM injection 7
ANTICOAGULANTS Heparin Low-molecular-weight (LMW) heparin Enoxaparin, Dalteparin, Tinzaparin Greater bioavailability (SC) Longer durations of action Administered once or twice a day Fondaparinux A small synthetic drug that contains the biologically active pentasaccharide Administered SC once daily 8
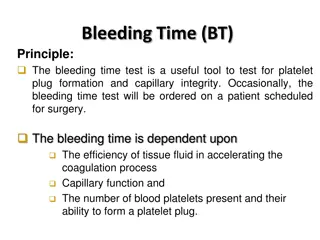
Heparin Mechanism and effects Heparin binds to antithrombin III (ATIII): irreversible inactivation of thrombin and factor Xa 1000-fold faster than ATIII alone Heparin provides anticoagulation immediately after administration Heparin monitoring Activated partial thromboplastin time (aPTT) 9
Mechanism and effects LMW heparins and fondaparinux bind ATIII same inhibitory effect on factor Xa as heparin ATIII they fail to affect thrombin a more selective action aPTT not required potential problem in renal failure due to decreased clearance 11
Clinical uses When anticoagulation is needed immediately e.g. when starting therapy Common uses: DVT Pulmonary embolism acute myocardial infarction in combination with thrombolytics for revascularization in combination with glycoprotein IIb/IIIa inhibitors during angioplasty and placement of coronary stents The drug of choice in pregnancy 12
Toxicity Increased bleeding (most common) may result in hemorrhagic stroke Protamine as antidote Not effective for LMW heparins and fondaparinux Heparin-induced thrombocytopenia (HIT) Due to antibody against complex of heparin and platelet factor 4 May yield venous thrombosis less likely with LMW heparins and fondaparinux Osteoporosis Due to prolonged use of unfractionated heparin 13
Direct Thrombin Inhibitors Lepirudin Recombinant form hirudin (Hirudo medicinalis) Desirudin and Bivalirudin Modified forms of hirudin Argatroban A small molecule with a short half-life Dabigatran Orally active 14
Mechanism and effects These drugs inhibit both soluble thrombin and the thrombin enmeshed within developing clots Bivalirudin also inhibits platelet activation 15
Clinical uses Alternatives to heparin primarily in patients with HIT Coronary angioplasty Bivalirudin in combination with aspirin Monitoring using aPTT requiured 16
Toxicity Bleeding No reversal agents exist Anaphylactic reactions Prolonged infusion of lepirudin induces antibodies that form a complex with lepirudin and prolong its action 17
Warfarin Small lipid-soluble molecule readily absorbed after oral administration Highly bound to plasma proteins (>99%) Its elimination depends on metabolism by cytochrome P450 enzymes 18
Mechanism of action Warfarin inhibits vitamin K epoxide reductase (VKOR) in liver reduced form of vitamin K factors II, VII, IX, X, protein C and S 19
Anticoagulant effect is observed within 8-12 h The action of warfarin can be reversed by: Vitamin K1 (slowly within 6-24 h) Transfusion with fresh or frozen plasma (more rapid reversal) Warfarin monitoring: Prothrombin time (PT) expressed by INR INR: 2-3 20
Clinical uses Chronic anticoagulation in all of the clinical situations described for heparin Exception: anticoagulation in pregnant women In DVT 1. Heparin + warfarin (5-7 days) 2. Warfarin (3-6 months) 21
Warfarin toxicity Bleeding (most common) Hypercoagulability early in therapy dermal vascular necrosis due to deficiency of protein C Bone defects and hemorrhage in fetus Contraindicated in pregnancy 22
Warfarin toxicity Drug interactions Cytochrome P450 inducers carbamazepine, phenytoin, rifampin, barbiturates Cytochrome P450 inhibitors amiodarone, selective serotonin reuptake inhibitors, cimetidine 23
THROMBOLYTIC AGENTS Streptokinase synthesized by streptococci Alteplase, Tenecteplase and Reteplase Recombinant forms of t-PA 25
Mechanism of Action Conversion of plasminogen to plasmin 26
Clinical Uses Alternative to coronary angioplasty Best result in ST-elevated MI and bundle branch block Prompt recanalization if used within 6 h Ischemic stroke Better clinical outcome if used within 3 h Cerebral hemorrhage must be ruled out before such use Severe pulmonary embolism 27
Toxicity Bleeding Same frequency with all thrombolytics Cerebral hemorrhage (most serious manifestation) Allergic reactions (streptokinase) Even at first dose (streptococcal infection history) Loss of drug efficacy Not observed with recombinant forms of t-PA BUT, t-PA is more expensive and not much more effective 28
ANTIPLATELET DRUGS Aspirin acts on COX irreversibly several-day effect Other NSAIDs not used as antiplatelet drug May interfere with aspirin antiplatelet effect Abciximab (monoclonal antibody), eptifibatide and tirofiban reversibly inhibit glycoprotein IIb/IIIa Clopidogrel, ticlopidine irreversibly inhibit the platelet ADP receptor 30
ANTIPLATELET DRUGS Dipyridamole and cilostazol Inhibit phosphodiesterase enzymes cAMP Inhibit uptake of adenosine by endothelial cells and RBCs Adenosine acts through platelet adenosine A2 receptors to increase platelet cAMP 31
Clinical Uses Aspirin To prevent first or further MI To prevent transient ischemic attacks, ischemic stroke, and other thrombotic events 32
Clinical Uses Glycoprotein IIb/IIIa inhibitors To prevent restenosis after coronary angioplasty In acute coronary syndromes (unstable angina and non-Q- wave acute MI) Clopidogrel and ticlopidine To prevent transient ischemic attacks and ischemic strokes especially in patients who cannot tolerate aspirin To prevent thrombosis in patients with coronary artery stent (clopidogrel) 33
Clinical Use Dipyridamole To prevent thrombosis in those with cardiac valve replacement (adjunct to warfarin) To treat intermittent claudication (a manifestation of peripheral arterial disease) 34