Benign and Malignant Thyroid Disease Surgery Overview
This content provides insights into thyroid anatomy, benign conditions like goitre and nodules, malignant risks, and surgical considerations by Prof. S.J. Kirk, MD, FRCS. Explore the learning objectives, clinical relevance, and indications for surgery.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Benign and Malignant Thyroid Disease-Surgery. PROF S.J. Kirk MD FRCS Consultant Surgeon SJK 1
Learning Objectives 1. Physiology and Anatomy of thyroid 2. Control of Metabolism 3. Clinical Relevance & Clinical Symptoms 4. Investigations of Thyroid Pathology 5. Indications for surgery 6. Surgical Procedures 7. Practical considerations Complications and what do I need to know Prof S.J. Kirk Hyperparathyroidism 2
In General the Anatomy of the Thyroid gland is not related to function. For Example: Thyroid function tests have limited value in the diagnosis of benign or malignant anatomical changes
Benign Thyroid Disease Goitre a generic term for swelling of the Thyroid Gland A thyroid nodule may be a lump in an otherwise normal thyroid gland. However, goitres may consist of many nodules (multinodular goitre) and solitary nodules may exist within a goitre. Benign Nontoxic Conditions Diffuse and Nodular (Multifocal, Unifocal) Goiter Benign Toxic Conditions Toxic Multinodular Goiter Graves Disease Inflammatory Conditions Chronic autoimmune (Hashimoto s) Thyroiditis (small shrunken thyroid)
Thyroid Nodules Between 4-7% of population have thyroid nodules, More common in women, Increase in frequency with age Fewer than 10% of solitary nodules are malignant. The risk of malignancy in a thyroid nodule is higher under the age of 20 and over the age of 70[3]. 3 Risk of carcinoma in a single nodule: 5-17% Papillary (80%) Follicular 15% Rates of carcinoma in multi nodular patients: 5-13% 6-28% have papillary carcinoma at autopsy 6 deaths per million (10 per yr in NI) SJK 8
Thyroid Nodules Nodules may be cystic, colloid, hyperplastic, adenomatous or cancerous. Iodine deficiency is the most common cause of goitre worldwide, but not common in the UK. Where salt is added to diet, autoimmune conditions (Hashimoto's thyroiditis and Graves' disease) are more common causes. Smoking increases the risk of nodular goitre. Family history. Thyroid nodules and cancers are more common after exposure to radiation. . Medication (such as lithium and amiodarone) may cause thyroid enlargement. It may also occur in pregnancy and menopause SJK 9
The Problem Thyroid nodules are very common Thyroid malignancy relatively rare Prognosis usually very good provided they are treated early The Issue to be addressed therefore is Is there a nodule in the thyroid gland, Is it an isolated nodule Does it represent sinister pathology
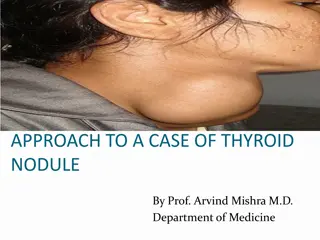
How Does Thyroid Swelling Present Thyroid lumps are often asymptomatic and are noticed by family members or seen in the mirror. They may sometimes cause pain and rarely present with features of compression of the trachea. Increasingly detected on investigations for other pathology
Who needs Referred Immediate referral Stridor associated with a thyroid mass Urgent (two-week rule) referral Child with a thyroid nodule. Unexplained hoarseness with goitre. Painless thyroid mass with rapid enlargement Other potential red flags in patients with Goitre Family history of thyroid cancer History of previous irradiation Non-urgent referral Thyroid nodules with abnormal TFTs. Sudden onset of pain within a thyroid lump.
Thyroid Assessment Triple Assessment What to do when a patient presents with a swelling of the Thyroid Gland Clinical: History and Examination Radiology: Ultrasound, CT. Pathology: FNA (solitary / dominant nodule in MNG)
History WHAT IS IMPORTANT IN THE HISTORY ? Age (50% malignant in children < 14 yrs) Sex (> risk in men) Growth rate / Pain Previous irradiation (20-50% malignant) Family history Voice changes / Pressure symptoms Symptoms of hypo / hyperthyroidism
Examination WHAT IS IMPORTANT ON EXAMINATION Size, Solitary or dominant nodule in MNG Ask the patient to drink some water and note the thyroid move as she/he swallows. Stand behind a seated patient examine the gland as she/he swallows again. Record character of lumps, asymmetry, size and tenderness. Consistency, Lymphadenopathy Signs of hypo / hyperthyroidism
Diferential Diagnosis for Thyroid Lumps/Swellings Non-toxic (simple) goitre - non-functioning nodules. TFTs are normal. Toxic multinodular goitre - functioning nodules. TFTs are abnormal. Retrosternal goitre (usually multinodular). Colloid nodule. Thyroid follicular adenoma. Thyroid cyst. Thyroid Cancer Graves Disease- diffusely enlarged overactive thyroid gland. Hashimotos Thyroiditis- autoimmune destruction of the gland may cause diffuse enlargement.
Ultrasound Assessment US reports thyroid size and appearance, 3D description of specific nodules, presence of paratracheal nodes, and evidence of invasive qualities. Doppler Flow important Useful in individuals undergoing FNA and have difficult lesions to palpate. Also beneficial in complex cysts, and nodules with questionable multinodularity SJK 18
FNA evaluation of solitary nodule FNA (fine needle aspiration) 4 Possible interpretations Insufficient for diagnosis Benign Thy2, Thy3A, Thy3F Malignant Thy4, Thy 5 Suspicious for follicular or Hurthle cell tumor SJK 19
Who Should have thyroid Surgery Large thyroid or multi-nodular goitre (a goitre is an enlarged thyroid gland) causing obstructive symptoms of breathing or swallowing difficulties Solitary nodule thyroid adenoma Thy3 Thyroid cancer Graves disease (hyperthyroidism or thyrotoxicosis, with eye signs or unresponsive) Where diagnosis remains uncertain
Thyroid Surgery Consistent techniques of thyroid surgery date back approximately 100 years Theodor Kocher of Bern, Switzerland made major contibutions to the understanding of thyroid disease and thyroid surgery 1872 - Performed his first thyroidectomy 1901 - had performed 2,000 thyroid procedure overall operative mortality had decreased from 50% to 4.5% 1909 - won the Nobel prize for his work SJK 22
Options Available Extent of Thyroidectomy Lumpectomy Partial thyroidectomy Subtotal thyroidectomy Lobectomy / hemithyroidectomy Near-total thyroidectomy Total thyroidectomy SJK 23
Thyroid Carcinoma 1.5% of all newly diagnosed cancers Number increasing over last 25 years; Previously 5 cases per 100,000 now rising to 12 per 1000 Female predominance (11.7 female to 4.2 male cases/100,000 No one increasing Female cancer in the world Death rate 0.5 cases per 100,000 world SJK 24
Papillary Carcinoma Commonest thyroid cancer (75%), most common between 40-50 years and in women. Tendancy to be multifocal multiple lesions spreads via the lymphatics. Follicular Carcinoma 40-60 years and in women, 15% of thyroid malignancy. Focal encapsulated lesions (multifocal disease is rare), Spread via haematogenous spread to bones and lungs. *Hurthle cell tumours variant of Follicular tumours Medullary Carcinoma 3% of thyroid cancers arise in the parafollicular cells (C-cells, derived from the neural crest cells). Produce raised calcitonin levels are associated (20% of cases) with MEN 2 syndrome (both 2a and 2b). Spreads by lymphatic channels nodal disease is associated with a very poor prognosis.
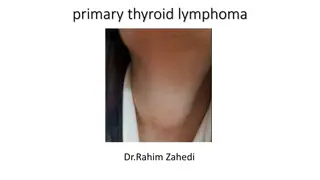
Anaplastic Thyroid Cancer These rare tumours, accounting for 5% of thyroid cancers, usually present in the elderly and are very aggressive. They tend to grow rapidly with early local invasion and often have spread by the time of presentation. Prognosis is poor and treatment is often supportive. Lymphoma Thyroid lymphomas are very rare, making up only 1-2% of all thyroid cancers. They usually present in people over 60 years old. They may grow quite rapidly, with marked compressive symptoms and B-Cell symptoms.
5 year Survival Rates Papillary Cancer Follicular Cancer Stage 1 100% 100% Stage 2 100% 100% Stage 3 95.8% 79.4% Stage 4 45.3% 47.1% SJK 27
Postoperative Management. It is important to know that all disease has been totally removed Thyroglobulin levels in the absence of normal thyroid tissue, is a sensitive and specific marker for the presence of thyroid cancer Ideally this assay should be performed when the thyrotropin (TSH) level is elevated Recombinant human TSH Ongoing clinical surveillance SJK 28
Postoperative treatment Radioactive iodine ablation (dose 30 -100 microcu )decreases the local recurrence and mortality rates in patients with stage 2 and stage 3 well-differentiated thyroid carcinoma Uptake is proportional to tumour differentiation Use of postoperative RAI and thyroid hormone supression has been advocated for patients with tumors > 1.5 cm Small (<1.0cms) tumour confined to thyroid no radioactive iodine Radio active iodine ineffective in lobectomy normal thyroid takes up iodine 100 more than malignant cells SJK 29
Key Points Thyroid lumps are a common presentation however only a small proportion of them are cancerous The main types of thyroid cancer are papillary, follicular, medullary, anaplastic, and lymphoma Red flag signs for any thyroid lump include pain, rapid growth, a cough, hoarse voice, or stridor, lymphadenopathy, or tethering of the lump Diagnosis is made via Ultrasound Scan followed by Fine Needle Aspiration Cytology Management options available range from surgical to medical to palliative
Complications of thyroid Surgery SJK 32
IMMEDIATE COMPLICATIONS HEMORRHAGE INFECTION RECURRENT LARYNGEAL NERVE PALSY THYROID CRISES OR STORM RESPIRATORY OBSTRUCTION PARATHYROID INSUFFICIENCY OR TETANY
LATE COMPLICATIONS THYROID INSUFFIENCY RECURRENT THROTOXICOSIS PROGRESSIVE EXOPHTHALMOS HYPERTROPHIC SCAR OR KELOID.
Question 1 of 5 Which of the following patients has clinical features most suspicious for thyroid cancer? 1. A 33 year old woman with a history of hypothyroidism with a 1 cm mobile nodule on examination 2. A 36 year old woman with a history of hypothyroidism on levothryroxine treatment for the past 8 years with a slightly enlarged boggy feeling thyroid gland on examination without any distinct nodules 3. A 30 year old man with symptoms of excessive sweating, weight loss, and hyperactivity and with exophthlamos and a slightly enlarged thyroid gland on exam without any palpable nodules. 4. A 27 year old asymptomatic male with a hard fixed 2 cm nodule on examination
Which of the following types of thyroid cancer has the worst prognosis? 1. Follicular 2. Medullary 3. Papillary 4. Anaplastic
A patient is experiencing voice hoarseness several days post- operatively after thyroidectomy for follicular thyroid cancer What is the most likely reason for this? 1. Anticipated post-operative local inflammation 2. Radioactive iodine treatment side effect 3. CN XI injury during surgery 4. Recurrent laryngeal nerve damage during sugery
What blood test is used to test for recurrence of medullary thyroid cancer after initial treatment? 1. Serum calcitonin level 2. Serum thyroglobulin level 3. Serum T3 and T4 levels 4. Serum calcium level
Which type of thyroid cancer has a hereditary component and is associated with MEN-2 syndrome? 1. Papillary cancer 2. Medullary cancer 3. Follicular cancer 4. Anaplastic cancer