Cytomegalovirus (CMV) Infection: Risks, Impact, and Prevention
Explore the comprehensive guide on CMV infection, including its origin, transmission, pathogenesis, epidemiology, significance, and implications in pregnancy and newborns. Understand the risks associated with CMV in different populations like immunocompromised individuals and solid organ transplant recipients. Discover preventive measures and the impact of congenital CMV infection on newborns.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
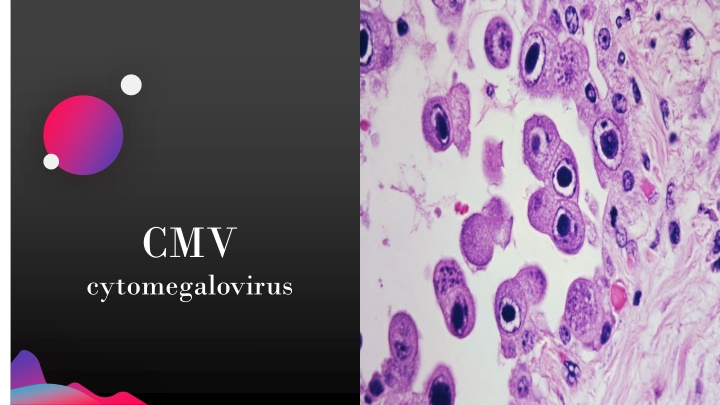
CMV cytomegalovirus
Jens Martensson cytomegalovirus Cyto: cell Mega: large 2
What is CMV? First isolated in 1956 from 2 dying infants CMV is a common virus within the herpes virus family Not readily spread by causal contact but requires repeated or prolonged intimate exposure Through body fluids, such as blood, saliva, urine, semen, and breast milk Also through solid organ transplantation & hematopoietic stem cell transplantation Jens Martensson CMV rarely causes problems in healthy individuals 4
Pathogenesis Once infected the virus remains in the person for life and may be reactivated from time to time especially in immunocompromised individuals Jens Martensson 5
Epidemiology of CMV Jens Martensson 6
Jens Martensson By the age of 5 approximately 1/3rd of children in the United States are infected 7
Significance of CMV Groups at high risk for serious complications: Infants infected in utero (congenital CMV infection) People with compromised immune systems Jens Martensson CMV infection can be fatal in people with weakened immune systems CMV is most common complication of solid organ transplant patients Effects of CMV in immunocompromised patients: Retinitis Colitis Esophagitis Encephalitis Pneumonia 8
CMV in pregnancy & newborns Women who develop an active CMV infection during pregnancy can pass the virus to their babies 90% of babies born with congenital CMV never develop symptoms or disabilities 10% of babies born with CMV can have brain, liver, spleen, lung, and growth problems. Most common health problem is hearing loss Jens Martensson 9
CMV Infection Risk in SOT Recipients Risk Category Donor (D) or Recipient (R) Seropositivity (+/-) D+/R- D+/R+, D-/R+ D-/R- Jens Martensson High Intermediate Low D+/R+ generally higher risk then D-/R+ 10
Prevention Prophylaxis entails antiviral medications to patients within 10 days of transplant and continued for 3-6 months Valganciclovir most commonly used Jens Martensson Preemptive Therapy: monitoring for CMV via blood tests at regular intervals Initiate antivirals after positive assays 11
Treatment Ganciclovir & Valganciclovir 1st line Ganciclovir used more for severe disease Boxed warning: myelosuppression Valganciclovir = prodrug of Ganciclovir Hazardous agents Females should use contraception during treatment and 30 days after Males for 90 days Side effects: Fever, thrombocytopenia, neutropenia N/V/D & anorexia Retinal detachment (Valganciclovir) Jens Martensson 12
Treatment Letermovir Cidofovir CMV specific antiviral compound that targets viral terminase complex encoded by UL56 FDA approved for CMV prevention in allogeneic hematopoietic cell transplant recipients Foscarnet May be given in cases where ganciclovir and foscarnet resistance is documented Relatively contraindicated in kidney transplant recipient's due to nephrotoxicity Often resistant to UL54 mutations Requires aggressive hydration & treatment with probenecid 2nd line Used for drug resistant or refractory CMV disease Recommended if UL97 and Ul54 mutations Highly nephrotoxic & requires close lab monitoring and hydration Jens Martensson 13
Patient Case #1 SP 65 y.o. male received heart transplant DR +/- January 2021 admitted July 2021 for CMV viremia. Jens Martensson Reports fatigue for weeks, nausea and vomiting more current. PMH: hypothyroidism, GERD, HTN, HLD, and depression. Medications: levothyroxine, Lisinopril, magnesium oxide, mycophenolate mofetil, rosuvastatin, tacrolimus 14
Patient Case Jens Martensson Stopped Valganciclovir prophylaxis Admitted 7/2021 for CMV viremia Discharged on Ganciclovir for 3 weeks Ganciclovir started 15
Patient Case #2 MM 38 y.o. male received kidney transplant in November 2019 with CMV D+/R+. Jens Martensson 1st noted to have CMV Viremia in November 2019, and has been treated for CMV on and off since Admitted to hospital June 2020 for persistent CMV Patient reports no symptoms except loose stools for past 2-3 days 16
Patient Case #2 PMH includes ESRD, T2DM, seizure disorder, non-obstructive CAD, depression, OSA, CVID, HFrEF, and previous kidney transplant in 2000. Jens Martensson Medications include: Gengraf, immune globulin, Novolog, levetiracetam, prednisone, metoprolol succinate, losartan, rosuvastatin, venlafaxine, aspirin 81mg 17
Patient Case 2 UL97 mutation found in June 2020 treated with IV ganciclovir CMV viremia detected 11/2019 & treated with Valganciclovir Viremia returned started Foscarnet 7/2021 Jens Martensson Viremia persists treated with Foscarnet Transitioned to PO Letermovir in 10/2020 Letermovir stopped 6/2021 18
Questions? Jens Martensson 19
Thank You Kaitlin Merriam Kaitlin.merriam@optioncare.com