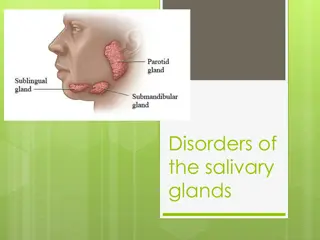
Disorders of the salivary glands
The content covers anatomy, inflammatory disorders including viral, bacterial, and HIV-associated sialadenitis in the parotid gland. It includes causes, clinical presentation, management, and complications associated with these conditions.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Disorders of the salivary glands Dr. Ali Jaffer Alghazzawi DAdvSurg (GI) CABS MBChB
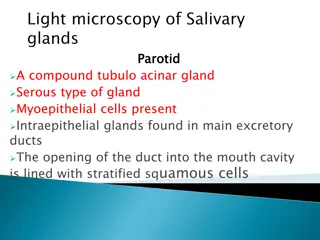
THE PAROTID GLAND- Anatomy Bounded by : the ramus of the mandible the base of the skull the mastoid process Posterior relation : the carotid sheath CNs XI&XII Structures run through the gland Facial nerve that divides into five branches The terminal branch of the external carotid artery (maxillary & superficial temporal a.) Retromandibular vein Intraparotid LN The facial nerve divides the gland into two lobes: superficial 80% deep 20% accessory (ant. To the superficial lobe) 1. 2. 3. 4.
THE PAROTID GLAND- inflammatory disorders Viral infections Mumps is the most common cause of acute painful swelling Predominantly affects children Spread: airborne infected saliva Prodromal period of 1-2 days (fever&headache) Clinically: pain exacerbated by eating and drinking , swelling Provides lifelong immunity Rx: paracetamol& adequate oral fluid Cx: orchitis, oophoritis, pancreatitis, sensorineural deafness & meningoencephalitis Recurrent parotitis of childhood It may be caused by an incompetent punctum that leads to soiling of the parotid ducts with contaminated oral fluids. Children 3-6 years ,rapid swelling of one or both glands, fever& malaise last 3-7 days. The symptoms worsen by chewing and eating. Sialography: punctate sialectasis (snowstorm) Rx: endoscopic washouts& antibiotics
THE PAROTID GLAND- inflammatory disorders Bacterial infections ( acute ascending bacterial siladentis) Previously described in dehydrated elderly patients following major surgery. Reduced salivary flow secondary to dehydration results in ascending infection via the parotid duct into the parotid paranchyma. Currently , it is commonly associated with a salivary calculus. Tender, painful swelling, generalised malaise, pyrexia and cervical lymphadenopathy Symptoms exacerbated by eating or drinking Intraoral exam; pus exuding form the parotid gland papilla Staphylococcus aureus or streptococcous virdans Rx; appropriate antibiotics absecss aspiration with large pore needle or formal drainage under anaesthesia (the skin incision should made low to avoid damage to the lower branch of the facial nerve) Sialography is contraindicated during acute infection.
THE PAROTID GLAND- inflammatory disorders HIV- associated sialadenitis May present as chronic parotitis in children. May present as classical Sjogren syndrome in adults clinically and histologically but there is lack autoantibody. May present with multiple parotid cysts which cause gross parotid swelling and facial disfigurement. CT&MRI; characteristic Swiss cheese appearance of multiple large cystic lesions. The swollen glands usually painless and may regress on the institution of antiviral therapy. Cysts may be aspirated
THE PAROTID GLAND- obstructive parotitis Stone formation (sialolithiasis) and strictures Parotid sialolithiasis 20% The stones are usually radiolucent. Locations; confluence of the collecting ducts, at the point the courses over the masseter muscle or in the distal aspect of the parotid duct adjacent to the parotid papilla. Presentation: intermittent swelling particularly in the mealtimes. Ix : US Rx: Small stones (less 4mm) retrieved by basket up to 8mm broken with lithotripsy larger than 8 mm removed by endoscopic assisted surgery Strictures of the parotid duct 20% Stricture lead to stagnation and mucus plug obstriction Clinically; meal time syndrome starting at the breakfast as swelling which persists. Massage release the plug with a gush of salty saliva. Rx dilatation and endoscopic washouts with steroid solutions Papillary obstruction trauma to the parotid results in inflammatory oedema and obstruction of salivary flow. May result dilation of the duct (mega-duct) which visible coursing the patient cheek Rx progressive dilation of the punctum& stent insertion. Papillotomy should be avoided as it cause stricture.
THE PAROTID GLAND- tumours The most common site of salivary tumours Most tumors arise from the superficial lobe. Slow-growing , painless swelling below ,in front of the ear or in the upper aspect of the neck Less commonly arise from accessory loble Rarely arise from deep lobe and present as paraphryngeal mass. Symptoms include difficulty in swallowing and snoring. Clinically there is diffuse firm swelling in the soft palate and tonsils 80- 90 % are benign Most common benign tumor is benign pleomorphic adenoma Most common malignant tumor is mucoepidermoid carcinoma, followed by adenocystic carcinoma which is notorious for its proclivity for perineural invasion and metastatic potential.
THE PAROTID GLAND- tumours Type Subgroup Common examples I Adenoma Pleomorphic Monomorphic Pleomorphic adenoma Adenolymphoma (Warthin s tumour) II Carcinoma Low grade Acinic cell carcinoma Adenoid cystic carcinoma Low-grade mucoepidermoid carcinoma High grade Adenocarcinoma Squamous cell carcinoma High-grade mucoepidermoid carcinoma III Non-epithelial tumours Haemangioma, lymphangioma IV Lymphomas Primary lymphomas Secondary lymphomas Non-Hodgkin s lymphomas Lymphomas in Sj gren s syndrome V Secondary tumours Local Distant Tumours of the head and neck especially Skin and bronchus VI Unclassified tumours VII Tumour-like lesions Solid lesions Benign lymphoepithelial lesion Adenomatoid hyperplasia Cystic lesions Salivary gland cysts
THE PAROTID GLAND- tumours Investigations US: confirm the lump intrinsic to the gland or not. facilitates the sampling of the lesion by FNAC. CT & MRI Open biopsy is contraindicated unless in gross malignancy and preoperative histological diagnosis is required as a preclude to radical parotidectomy
THE PAROTID GLAND- tumours Parotidectomy A. Superficial parotidectomy: the part of the gland superficial to the facial nerve is removed - Benign, low grade and low stage malignant tumours - Partial superficial parotidectomy for small tumours - Extracapsular dissection: benign parotid gland tumours B. Radical parotidectomy: is performed when there is clear histological evidence of high grade malignant tumors eg squamous cell carcinoma with invasion of the facial nerve. it involves removal of all parotid tissue and division of the facial trunk through the main trunk with removal of the ipsilateral masseter muscle and may require neck dissection particularly when there is clinical, radioliogical and cytological evidence o f lymph nodes metastasis. COMPLICATIONS OF PAROTID GLAND SURGERY haematoma formation; infection; deformity: unsightly scar and retromandibular hollowing; temporary facial nerve weakness; transection of the facial nerve and permanent facial weakness; sialocele; facial numbness; permanent numbness of the ear lobe associated with great auricular nerve transection; Frey s syndrome.
THE PAROTID GLAND- tumours Frey s syndrome (gustatory sweating) is considered an inevitable consequence of parotidectomy unless preventive measures are taken . It results from damage to the autonomic innervation of the salivary gland with inappropriate regeneration of the postganglionic parasympathetic nerve fibres of the auriculotemporal nerve that aberrantly stimulate the sweat glands of the overlying skin. Clinically; sweating and erythema (flushing) over the region of surgical excision of the parotid gland Diagnosis ;starch iodine test. This involves painting the affected area with iodine, which is allowed to dry before applying dry starch, which turns blue on exposure to iodine in the presence of sweat. Sweating is stimulated by salivary stimulation. PREVENTION sternomastoid muscle flap; temporalis fascial flap; insertion of artificial membranes between the skin and theparotid bed. All these methods replace the barrier between the skin and the parotid bed to minimise inappropriate regeneration of autonomic nerve fibres. MANAGEMENT OF ESTABLISHED FREY S SYNDROME antiperspirants, containing aluminium chloride; denervation by tympanic neurectomy; the injection of botulinum toxin into the affected skin. ( most effective and can be performed as an out-patient).