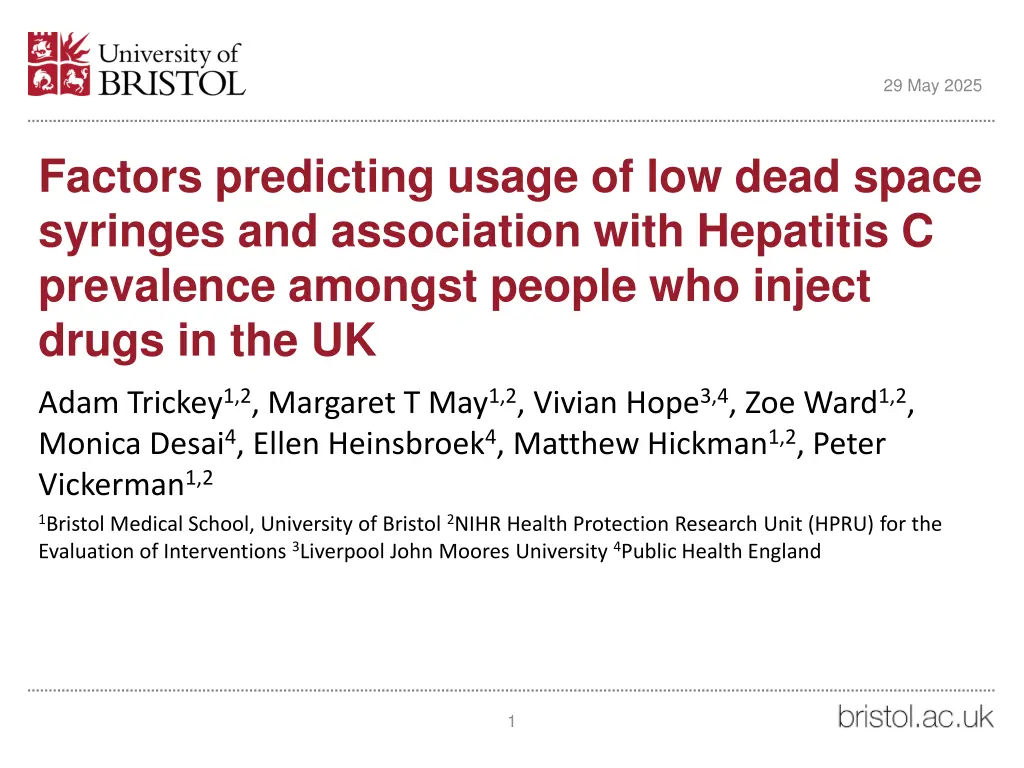
Factors Predicting Usage of Low Dead Space Syringes and Hepatitis C Prevalence Among People Who Inject Drugs in the UK
This study explores the factors influencing the use of low dead space syringes among people who inject drugs in the UK and its association with the prevalence of Hepatitis C. It discusses the risks of blood-borne viral infections, the benefits of low dead space syringes, and the recommendations for preventing the transmission of viruses through injecting equipment.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
29 May 2025 Factors predicting usage of low dead space syringes and association with Hepatitis C prevalence amongst people who inject drugs in the UK Adam Trickey1,2, Margaret T May1,2, Vivian Hope3,4, Zoe Ward1,2, Monica Desai4, Ellen Heinsbroek4, Matthew Hickman1,2, Peter Vickerman1,2 1Bristol Medical School, University of Bristol 2NIHR Health Protection Research Unit (HPRU) for the Evaluation of Interventions 3Liverpool John Moores University 4Public Health England 1
29 May 2025 People who inject drugs (PWID) and hepatitis C virus (HCV) People who inject drugs (PWID) are at risk of blood borne viral infections through the sharing of needles, syringes, and other injecting equipment1 There is high prevalence of these infections, such as hepatitis C virus (HCV), amongst PWID1 Needle and syringe programmes and opiate substitution therapy can decrease the risk of getting HCV2 However, modelling suggests they are not enough to reduce HCV to low levels2 So other prevention or treatment strategies are required 1: Degenhardt, 2017. 2: Platt, 2017 2
29 May 2025 Low dead space syringes (LDSS) Syringes with attached needles, typically have a lower dead space and retain far less blood following an injection, than syringes with detachable needles1 Fixed needle (1ml) Detachable needle Low dead space syringes (LDSS) High dead space syringes (HDSS) Standard syringe with standard needle Average dead space (99 ) Low dead space Standard syringe with low dead space needle Average dead space (13 l) Low dead space syringe with fixed needle Average dead space (3 l) Standard syringe with standard needle Average dead space (99 ) Low dead space syringe with standard needle Average dead space (45 ) Standard syringe with low dead space needle Average dead space (13 l) Low dead space syringe with fixed needle Average dead space (3 l) 1: Zule, 2013 syringe with standard needle Average dead space (45 ) 3
29 May 2025 Low dead space syringes (LDSS) For PWID that share injecting equipment, using low dead space syringes (LDSS) instead of high dead space syringes (HDSS) may lead to a reduced risk of acquiring blood borne infections1 The volume of blood held in a syringe predicts: The amount of viral load transmitted2 Virus survival outside of the body2 The World Health Organization (WHO) recommends that LDSS are supplied to prevent the transmission of blood borne viruses However, evidence for a prevention benefit is limited3 1: Vickerman, 2013, 2: Gaughwin, 1991. 3: Jacka, 2013 4
29 May 2025 Research into which subgroups of PWID use LDSS has been limited Some research indicates HDSS with longer needles are required for injecting into veins around the groin1 HDSS allow replacement of needles during an injection episode1 Injecting practices differ depending on the drug2 Some older PWID inject into their groin after veins in the limbs are worn out3 Previous research indicates that groin injectors are more likely to have high risk behaviours3 1: Zule, 2013, 2: Lankenau, 2004, 3: Hope, 2015 5
29 May 2025 Aims To investigate the predictors of LDSS use amongst PWID to gain information about how to intervene To examine whether the type of syringe used is associated with reduced risk of HCV in the UK 6
29 May 2025 Dataset 2014 and 2015 Unlinked Anonymous Monitoring Survey (UAM) Annual sero-behavioural survey of PWID Recruited from centres providing drug treatment, needle and syringe programmes and outreach work Data from across England, Wales, and Northern Ireland (not Scotland) Participants answer questionnaire about their drug use behaviours and demographic information Participants provide a dried blood spot sample that was tested for HCV antibodies. 7
29 May 2025 LDSS data We calculated the percentage of syringes used in the past month that were LDSS or HDSS Used two questions based on self-report: How many individual needles (including ones attached to syringes) did you get from Needle Exchanges during the last month (28 days)? How many of these needles were already attached to syringes (barrels)? We excluded participants without information on LDSS use. We used multiple imputation to account for missing data in covariates. 8
29 May 2025 Methods To investigate which subgroups of PWID used LDSS all the time, we used: Logistic regression to estimate unadjusted odds ratios (OR) with 95% confidence intervals (CI) of 100% LDSS usage, vs 0-99% use, with demographic and injecting variables. Multivariable logistic regression with backwards selection of predictors. To investigate the relationship between LDSS use and HCV infection risk: We estimated associations of LDSS usage with HCV with and without adjusting for groin injecting due to the correlation between HDSS use and groin injecting Using multivariable logistic regression We repeated this with an interaction term between LDSS use and groin injecting We repeated this analysis including an interaction term between LDSS use and whether a PWID recently started injecting (less than 3 years ago) as many prevalent HCV infections will have occurred many years ago 9
29 May 2025 Results Demographics and characteristics 3,083 had injected in the previous month -> 909 (28%) excluded due to missing information on LDSS use -> 2,174 included in the analyses -> 55% always used LDSS -> 17% used both LDSS and HDSS -> 27% always used HDSS. Women anti-HCV positive Ever been in prison Homeless in last year Shared equipment last month Injected into groin last month Injected heroin last month Injected crack last month Injected cocaine last month Injected speed last month Variable Number Age (years) - Mean Days injecting last month Mean Injecting duration (years) - Mean Total 2,174 37 17 15 24% 55% 70% 19% 37% 40% 90% 43% 8% 21% 10
29 May 2025 Predictors of LDSS usage Those injecting into the groin were very unlikely to use LDSS compared to those not injecting into the groin, aOR 0.14 (0.11-0.17) Injecting crack was predictive of not using LDSS, aOR 0.79 (0.63-0.98) Heroin injectors were more likely to use LDSS than non-heroin injectors, aOR 1.47 (1.04-2.08) 11
29 May 2025 Regional variation Highest: West Midlands (68%) Second: London (66%) Lowest: East Midlands (45%) 12
29 May 2025 LDSS usage and HCV 13
29 May 2025 Odds ratios (OR) of being anti-HCV positive (against negative) N=2,174. Fully adjusted without groin injecting Variable Unadjusted Fully adjusted 0-99% LDSS use 1 1 1 0.64 (0.54, 0.76) 0.77 (0.64, 0.93) 0.95 (0.77, 1.18) 100% LDSS use Injections (every 10) per month 1.11 (0.92, 1.33) 1.10 (0.90, 1.35) 1.07 (0.87, 1.31) Shared equipment last month 1.22 (1.01, 1.46) 1.27 (1.04, 1.55) 1.30 (1.06, 1.59) Injecting duration 1.08 (1.07, 1.09) 1.07 (1.06, 1.08) 1.07 (1.06, 1.08) Injecting crack 2.58 (2.15, 3.09) 2.23 (1.83, 2.71) 2.17 (1.78, 2.65) Injecting heroin 1.67 (1.24, 2.24) 1.20 (0.86, 1.68) 1.15 (0.82, 1.61) Injecting other drug 0.77 (0.54, 1.11) 0.78 (0.52, 1.17) 0.81 (0.54, 1.21) 1.67 (1.35, 2.08) Injecting into groin 2.35 (1.96, 2.81) NA Ever been in prison 2.83 (2.34, 3.42) 2.10 (1.71, 2.58) 2.04 (1.66, 2.51) Homeless in last year Also: The aOR of HCV infection for exclusive LDSS use (versus any HDSS use) amongst non-groin injectors was 0.86 (0.65, 1.13). 1.18 (0.95, 1.47) 1.23 (0.96, 1.57) 1.20 (0.94, 1.53) 14
29 May 2025 LDSS usage and HCV amongst PWID that had recently started injecting Fully adjusted without groin injecting 1 0.53 (0.30, 0.95) Variable 0-99% LDSS use & recent starter 100% LDSS use & recent starter Unadjusted 1 0.46 (0.26, 0.80) Fully adjusted 1 0.60 (0.34, 1.08) Injections (every 10) per month Shared equipment last month Injecting duration Injecting crack Injecting heroin Injecting other drug Injecting into groin Ever been in prison Homeless in last year 1.11 (0.92, 1.33) 1.22 (1.01, 1.46) 1.08 (1.07, 1.09) 2.58 (2.15, 3.09) 1.67 (1.24, 2.24) 0.77 (0.54, 1.11) 2.35 (1.96, 2.81) 2.83 (2.34, 3.42) 1.18 (0.95, 1.47) 1.10 (0.90, 1.35) 1.29 (1.05, 1.57) 1.06 (1.05, 1.08) 2.26 (1.85, 2.76) 1.18 (0.84, 1.65) 0.78 (0.52, 1.17) NA 2.06 (1.68, 2.53) 1.23 (0.97, 1.58) 1.07 (0.87, 1.31) 1.31 (1.07, 1.61) 1.06 (1.05, 1.07) 2.20 (1.81, 2.69) 1.13 (0.81, 1.58) 0.81 (0.54, 1.22) 1.66 (1.34, 2.06) 2.00 (1.63, 2.47) 1.21 (0.94, 1.54) 15
29 May 2025 Limitations Hard to separate out effects of LDSS use and groin injecting 98% responded to the groin injecting question, but only 72% to the LDSS questions We could only examine injecting practices in the past month We were unable to determine how current injecting practices related to practice over time Do not know when participants had been infected with HCV, could have been many years ago Recall bias and social desirability considerations Some detachable needles are now low dead space, but this availability was unlikely during the study period 16
29 May 2025 Main results Around 2/3 of our sample used LDSS every time they injected in the past month. 1/4 were not using LDSS. Geographic differences in LDSS use across the UK, possibly due to variation in provision of LDSS, and variation in the types of drugs injected Our study found an unadjusted association between LDSS use and HCV infection. Association maintained following adjustment for drug type and injecting duration These associations weakened following adjustment for injecting into the groin, which was highly correlated with HDSS use 17
29 May 2025 Implications To determine whether LDSS use reduces HCV infection risk it is crucial to understand the relationship with groin injecting We know more about who uses LDSS in the UK Groin injectors are a distinct subset of PWID who use HDSS with longer needles to enable injection into deep lying veins For WHO guidelines to work needles are required that meet the needs of all PWID and minimise dead space Detachable syringes with lower dead space are being developed but they still have greater dead space than LDSS The association amongst recent initiates suggests LDSS may reduce HCV infection risk but more evidence is needed to confirm this 18
29 May 2025 Acknowledgements No conflicts of interest. 19