Hemodynamic Disorders and Embolism
Learn about hemodynamic disorders and embolism, including pulmonary thromboembolism and systemic thromboembolism. Discover the causes, consequences, and complications of embolism in different parts of the body. Explore the risks and outcomes associated with various types of emboli, such as thromboembolism and fat embolism. Gain insights into the diagnosis and treatment of these conditions to improve patient care and outcomes.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Hemodynamic disorder: Hemodynamic disorder: Embolism DR SITI ZALEHA S.ABDULLAH, DR TIN TIN THEIN, DR AYE AYE WYNN, DR LIA NATASHA AMIT
Embolism An embolus is a detached intravascular solid, liquid, or gaseous mass that is carried by the blood to a distant site, where it causes tissue dysfunction or infarction. The primary consequence of systemic embolization is ischemic necrosis (infarction) of downstream tissues. Whereas embolization in the pulmonary circulation leads to hypoxia, hypotension, and right- sided heart failure. Thromboembolism; The vast majority of emboli derive from a dislodged thrombus
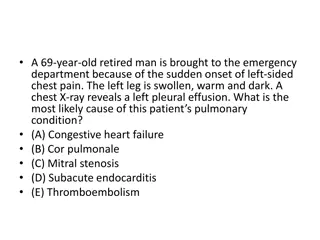
Pulmonary Thromboembolism >95% of cases, venous emboli originate from deep venous thromboses. The incidence 2 to 4 per 1000 hospitalized patients. Most pulmonary emboli (60% 80%) are small and clinically silent. A large embolus that blocks a major pulmonary artery can cause sudden death. Embolic obstruction of medium-sized arteries and subsequent rupture of downstream capillaries rendered anoxic can cause pulmonary hemorrhage. Embolism to small end-arteriolar pulmonary branches usually causes infarction. Multiple emboli occurring through time can cause pulmonary hypertension and right ventricular failure (cor-pulmonale).
Systemic Thromboembolism 80% arise from intracardiac mural thrombi. Two-thirds of these are associated with left ventricular infarcts . 25% with dilated left atria (ie; secondary to mitral valve disease). The remainder originate from aortic aneurysms, thrombi overlying ulcerated atherosclerotic plaques, fragmented valvular vegetations or the venous system (paradoxical emboli). 10% to 15% of systemic emboli are of unknown origin. Arterial emboli can travel virtually anywhere; their final resting place understandably depends on their point of origin and the relative flow rates of blood to the downstream tissues.
Systemic Thromboembolism Common arteriolar embolization sites include the lower extremities (75%) and central nervous system (10%). Intestines, kidneys, and spleen are less common targets. The consequences of embolization depend on the caliber of the occluded vessel, the collateral supply, and the affected tissue s vulnerability to anoxia. Arterial emboli often lodge in end arteries and cause infarction.
Soft tissue crush injury / rupture of marrow vascular sinusoid release fat globules into the circulation. 90% of individual with skeletal injuries. Pathogenesis involves mechanical obstruction and biochemical injury. Fat embolism Amniotic fluid embolism Uncommon, grave complication of labor and immediate postpartum period (1 in 40 000 deliveries). 80% mortality rate. Due to entry of amniotic fluid into circulation via tears in the placental membranes and / or uterine vein rupture. Gas bubbles within the circulation can coalesce and cause obstruction leading to distal ischaemic injury. A particular form of gas embolism, called decompression sickness, occurs when individuals experience sudden decreases in atmospheric pressure (Scuba and deep sea divers). When air is breathed at high pressure (e.g., during a deep sea dive), increased amounts of gas (particularly nitrogen) are dissolved in the blood and tissues. If the diver then ascends (depressurizes) too rapidly, the nitrogen comes out of solution in the tissues and the blood. Air embolism