Thrombosis and Embolism in General Surgery
Thromboembolic events involving the coagulation system can lead to tissue damage through the formation of blood clots and migration to distant sites, causing ischemia and infarction. Understanding the mechanisms of normal hemostasis and the pathophysiology of arterial vasoconstriction, primary and secondary hemostasis is crucial in managing conditions like myocardial infarction, stroke, and pulmonary embolism. Explore the complexities of clot formation, platelet activation, and counter-regulatory mechanisms to better comprehend the impact on morbidity and mortality.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Odessa National Medical University, Department Of General Surgery N 1 Thrombosis and Embolism 2nd Year Pathology 2010
Thromboembolic events Activation of coagulation system Solid mass of blood constituents formed within the vasculature Thrombosis formation of blood clot at site of coagulation system activation Embolism migration through the vasculature to a distant site Cause tissue damage by occlusion of blood vessels Result in ischaemia and infarction 2nd Year Pathology 2010
Thromboembolic events ischaemia lack of oxygen due to impaired blood supply results in reversible cell injury or irreversible injury and necrosis (infarction) depends on duration & tissue s metabolic needs infarction tissue necrosis due to ischaemia Major causes of morbidity & mortality 2nd Year Pathology 2010 myocardial infarction, stroke, pulmonary embolism
Normal Haemostasis Maintains blood in fluid state in normal vessels Induces rapid, localized plug at site of vascular injury Complex set of activators & inhibitors (procoagulant & anticoagulant influences) 3 components endothelium and vascular wall a) platelets b) proteins of coagulation and fibrinolytic cascades c) 2nd Year Pathology 2010
Normal Haemostasis Arteriolar vasoconstriction Primary haemostasis temporary platelet plug a) Platelet adhesion b) Platelet activation (shape change & granule release) c) Platelet aggregation Secondary haemostasis solid permanent plug a) Activation of coagulation cascade b) Conversion of fibrinogen to insoluble fibrin c) Aggregates of polymerized fibrin & platelets Counter-regulatory mechanisms restrict plug to site of injury 1. 2. 3. 4. 2nd Year Pathology 2010
Haemostatic Mechanisms - 1 Arteriolar vasoconstriction Exposure of subendothelial nerve fibres reflex Endothelial damage endothelin secretion Primary haemostasis Von Willebrand factor binds to exposed collagen Platelets bind to vWF Platelets activated on contact & release granule contents, including ADP and thromboxane (TXA2) d) Platelet aggregation stimulated by ADP and TXA2 e) Autocatalytic cascade of plt adhesion, activation and aggregation (ADP and TXA2) 1. a) b) 2. a) b) c) 2nd Year Pathology 2010
Platelets Glycoprotein receptors (integrins) on surface GpIb: binds vWF important in plt adhesion GpIIb-IIIa: binds fibrinogen important in secondary haemostasis GpIb deficiency Bernard-Soulier syndrome vWF deficiency von Willebrand s disease GpIIb-IIIa deficiency Glanzmann s Thombasthenia Alpha granules Adhesion molecules (P-selectin, vWF) Coagulation factors (fibrinogen, fibronectin, factor V and vWF) Growth factors (PDGF, TGF-beta) Dense bodies ADP, ATP, calcium Vasoactive molecules (histamine, serotonin, adrenalin) Other enzymes Thromboxane synthetase TXA2 1. a) b) Bleeding disorders 2. a) b) c) 3. a) b) 4. a) 2nd Year Pathology 2010
Haemostatic Mechanisms - 2 Secondary haemostasis Tissue factor released from damaged endothelium 3. a) Tissue factor and secreted plt factors activate coagulation cascade Activation of thrombin b) c) Conversion of fibrinogen to insoluble fibrin fibrin deposition Autocatalytic activation of coagulation cascade Binding to plt surface receptors further plt aggregation and activation 2nd Year Pathology 2010 Fibrin deposition stabilizes and anchors aggregated plts
Haemostatic Mechanisms - 3 Counter-regulatory mechanisms Fibrinolytic pathway (Plasminogen activation formation of plasmin) Coagulation cascade Circulating urokinase-like plasminogen activator (u-PA) Release of tissue-type plasminogen activator (t-PA) from endothelium Anticoagulant pathways Heparin-like molecules on endothelial surface antithrombin III activation Endothelial synthesis of Protein S Thrombin thrombomodulin activation Protein C activation 4. a) a) Fibrin and fibrinogen degradation b) c) b) a) Inhibition of coagulation b) c) 2nd Year Pathology 2010
Extrinsic pathway Intrinsic pathway Inhibitors Tissue factor pathway inhibitor Tissue Factor XII XI IX Collagen VII VIIa XIIa XIa IXa + VIIIa Protein C + Protein S X Xa Positive Feedback Va V Antithrombin III Prothrombin Thrombin Fibrinogen Fibrin XIII 2nd Year Pathology 2010 Fibrinolytic cascade Cross-linked fibrin
Thrombosis Inappropriate activation of haemostatic mechanisms E.g. uninjured vessel or very minor injury Definition: formation of solid mass of blood constituents within vascular system in life Virchow s triad: changes in the vessel wall changes in blood flow changes in the blood constituents 1. 2. 3. 2nd Year Pathology 2010
Changes in the vessel wall Primarily damage to intimal surface (endothelium) Causes of endothelial cell injury: ulcerated atherosclerotic plaques scarred valves in endocarditis / prosthetic valves radiation, cigarette smoke, cholesterol/lipids Results of endothelial cell injury: exposed subendothelial extracellular matrix platelet activation activation of coagulation cascade depletion of antiplatelet, anticoagulant and fibrinolytic functions endothelial activation activationof procoagulant functions 2nd Year Pathology 2010
Endothelium Antithrombotic functions Antiplatelet Adenosine diphosphatase ( ADP) Prostacyclin and nitric oxide (also vasodilation) Anticoagulant Heparin-like molecules (activate antithrombin III) Thrombomodulin (activates protein C) Protein S synthesis Fibrinolytic t-PA Procoagulant functions Production of vWF Production of tissue factor Binding of factors IXa and Xa 2nd Year Pathology 2010
Changes in blood flow Normal flow is laminar cells in centre of blood stream clear zone of plasma adjacent to endothelium Disrupted flow is static or turbulent Stasis Platelets in contact with endothelium Prevent dilution of clotting factors Retard inflow of clotting factor inhibitors e.g. myocardial infarct, aneurysm, atrial fibrillation, hyperviscosity syndromes Turbulence Eddy currents with local pockets of stasis Promote endothelial cell injury e.g. ulcerated atherosclerotic plaque 2nd Year Pathology 2010
Changes in blood constituents Hypercoagulability Leads to recurrent venous thrombosis, arterial thrombosis, recurrent abortion and stillbirths Inherited (see table overleaf) or Acquired (below) oral contraceptive use pregnancy / hyperoestrogenic states malignancy - elaboration of a procoagulant factor, leading to arterial and venous thrombosis (Trousseau s syndrome) tissue damage surgery, trauma, burns Hyperviscosity predisposes to stasis in small vessels polycythaemia) / deformed RBC s (sickle cell anaemia) Presence of endothelial cell toxins toxins in cigarette smoke, high levels of lipid or cholesterol predispose to endothelial cell injury 2nd Year Pathology 2010
Anti-phospholipid syndrome autoantibodies bind plasma proteins with affinity for phospholipid surfaces, including coagulation factors associated with SLE most common inherited form of hypercoagulability present in 5% of Caucasians mutant factor V resistant to protein C inactivation as common as factor V Leiden mutation genetic and environmental factors including OCP use autosomal dominantly inherited deficiencies of anticoagulant factors Factor V Leiden mutation Elevated factor VIII Protein C, Protein S, antithrombin III deficiencies Homocystinemia elevated plasma homocysteine levels also increased rick of atherosclerosis increases the level and activity of prothrombin Prothrombin mutation Plasminogen abnormalities Plasminogen or tissue plasminogen activator deficiency, plasminogen activator inhibitor excess features resemble protein C or S deficiency autosomal dominant disorder, precipitated by stress Sticky platelet syndrome 2nd Year Pathology 2010
Thrombus Formation Atherosclerotic plaque 1. initial fatty streak 2. plaque enlarges (smoking/hyperlipidaemia) 3. turbulence (due to protrusion into lumen) 4. loss of endothelium & exposure of collagen 5. platelet adherence & activation 6. fibrin meshwork deposition with RBC entrapment 7. more turbulence, more platelet adherence, more fibrin deposition 8. thrombus of alternating layers of platelets, fibrin and red blood cells 2nd Year Pathology 2010
Arterial Thrombi Large vessels (aorta, heart) - nonocclusive / mural Smaller vessels (coronary arteries, leg arteries) - often occlusive Classically have alternating white and red layers called lines of Zahn alternating layers of pale platelets and darker RBC s e.g. aneurysmal sacs, infarcted left ventricle, damaged heart valves, atherosclerotic plaques Consequences: Ischaemia in tissues distal to thrombus with possible necrosis (infarction) May embolize due to rapid flow 2nd Year Pathology 2010
Arterial Thrombi 2nd Year Pathology 2010 Non-occlusive thrombi in wall of atherosclerotic aorta
Arterial Thrombi 2nd Year Pathology 2010 Occlusive thrombus in wall of atherosclerotic coronary artery
Arterial Thrombi a b 2nd Year Pathology 2010 Alternating layers of a) platelets and fibrin and b) red blood cells
Venous Thrombi Sites of stasis, commonly veins of lower extremity Red - More enmeshed erythrocytes, less platelets Occlusive Predisposing factors Bed rest, immobilization, heart failure, surgery, trauma, pregnancy, hypercoagulable states Consequences: Rarely cause ischaemia if affect arterial supply More commonly embolize 2nd Year Pathology 2010
Fate of Thrombi Dissolution by fibrinolysis Propagation along length of vessel complete vessel occlusion Embolization Recanalization capillaries invade thrombus to re-establish blood flow Organization Inflammation and fibrosis replacement by scar, may obliterate vessel lumen 1. 2. 3. 4. 5. Recent thrombi may be completely dissolved Older thrombi more resistent to fibrinolysis (extensive fibrin polymerization) 2nd Year Pathology 2010
Consequences of Thrombosis Arterial Thrombosis Obstruction: Myocardial infarction due to coronary artery thrombosis Cerebral infarction (Stroke) due to carotid artery thrombosis Acute lower limb ischaemia & infarction due to femoral/popliteal artery thrombosis Embolization: Cardiac/aortic mural thrombi emboli to brain, kidneys, spleen Venous Thrombosis e.g. deep leg veins Obstruction: Local congestion, swelling, pain, tenderness Oedema and impaired venous drainage Infection & varicose ulcers Embolization Thrombi at or above knee pulmonary emboli 2nd Year Pathology 2010
Consequences of Thrombosis 2nd Year Pathology 2010 Acute myocardial infarct secondary to coronary artery thrombosis
Embolism Any intravascular mass (solid, liquid or gas) carried by blood to site distant from point of origin Most derived from thrombi (thromboembolism) Lodge in vessels too small to permit further passage partial / complete vascular occlusion distal tissue ischaemia & infarction 2nd Year Pathology 2010
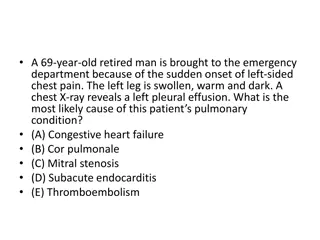
Pulmonary Thromboembolism Arise from thrombi in systemic venous circulation leg veins (95%) pelvic veins intracranial venous sinuses Risk factors as for venous thrombosis Effects are two-fold: Possible infarction of lung tissue supplied by infarct Interruption of oxygenation of blood within this area Interruption of right ventricular outflow Effects depend on size 2nd Year Pathology 2010
Pulmonary Thromboembolism 2nd Year Pathology 2010 Embolus migrates from deep leg veins through venous system to pulmonary circulation
Pulmonary Thromboembolism 2nd Year Pathology 2010 Saddle embolus in branching main pulmonary artery
Pulmonary Thromboembolism 2nd Year Pathology 2010 Small pulmonary embolus in branch of pulmonary artery
Pulmonary Thromboembolism Small: silent due to collateral bronchial artery flow organization with cumulative damage (idiopathic pulmonary hypertension) Medium: pulmonary infarct with acute respiratory and cardiac symptoms Large: right heart failure & collapse (>60% pulm circ) Massive: sudden death e.g. saddle embolus 2nd Year Pathology 2010
Systemic Thromboembolism Arise in arterial system (heart/large arteries) Atheromatous plaque with thrombus Valve vegetation Atrial thrombus (Atrial Fibrillation) Old myocardial infarct (adynamic) Recent myocardial infarct (loss of endothelium) Rarely paradoxical embolus from venous system (through septal defect in heart) 2nd Year Pathology 2010
Systemic Thromboembolism Travel in systemic circulation Cause arterial occlusion, distal ischaemia & infarction brain - stroke, neurological deficit / death renal/splenic infarcts may be asymptomatic, seen as ischaemic scars at autopsy intestine - mesenteric emboli cause intestinal infarction, can be lethal limbs - ischaemic foot (dry gangrene) 2nd Year Pathology 2010
Systemic Thromboembolism 2nd Year Pathology 2010 Renal infarct secondary to systemic thromboembolism
Other Forms of Embolism Fat embolism Next most common after thromoemboli Fracture of long bones / Burns / Trauma Can cause severe pulmonary insufficiency Air embolism Gas bubbles obstructing vascular flow Surgical /obstetric procedures / Chest wall injury Decompression sickness Gases dissolve in blood at high pressure Come out as bubbles during rapid decompression N2 bubbles remain - muscle, jts, lungs, brain, heart 2nd Year Pathology 2010
Other Forms of Embolism 2nd Year Pathology 2010 Fat emboli in the lung
Other Forms of Embolism Atheromatous plaque embolism Platelet emboli Infective emboli (infective endocarditis) Tumour emboli Foreign material (talc in IVDU) Amniotic fluid embolism amniotic fluid forced into uterine veins @ delivery, causing respiratory distress 2nd Year Pathology 2010
Other Forms of Embolism 2nd Year Pathology 2010 Kidney showing cholesterol embolism from an atherosclerotic plaque
Disseminated Intravascular Coagulation Thrombotic disorder Sudden / insidious onset of widespread fibrin thrombi in microcirculation Diffuse circulatory insufficiency Brain, lungs, heart, kidneys Consumption of platelets and coagulation factors Activation of fibrinolytic pathways Severe bleeding disorder Complication of any widespread activation of thrombin Sepsis, Burns, Trauma, Extensive Surgery, Amniotic fluid embolism, Carcinoma, Intravascular haemolysis 2nd Year Pathology 2010
Non-thromboembolic Vascular Insufficiency Atheroma M.I., hypertension due to renal artery stenosis Spasm angina, Raynaud s phenomenon External Compression surgery, torsion, tumour Steal syndrome Blood diverted to one organ or tissue due to increased demands, compromising the supply of another Hyperviscosity Sickle cell disease splenic infarcts 2nd Year Pathology 2010
Consequences of Vascular Insufficiency Number of determining factors Size of vessel and size of vascular territory Partial / total vascular occlusion Duration of ischaemia Metabolic needs of tissue involved Presence or absence of alternative (collateral) circulation Most important consequence = Infarction Commonest cause of death in western world 2nd Year Pathology 2010
Summary Thrombosis Normal haemostatic mechanisms Pathogenesis: Virchow s triad Arterial vs Venous Thrombi Fate of Thrombi Embolism Types of embolus Systemic vs Pulmonary Embolism Other Causes of Vascular Insufficiency Consequences of Vascular Insufficiency 2nd Year Pathology 2010