Safety and Efficacy of ABT-450/r/Ombitasvir, Dasabuvir, and Ribavirin
Coinfection with HCV and HIV poses significant health risks, and effective treatment is crucial. The study evaluates the safety and efficacy of ABT-450/r, ombitasvir, dasabuvir, and ribavirin in co-infected patients. Results indicate improved SVR rates and a favorable safety profile compared to traditional therapies. IFN-free regimens show promise in treating HCV/HIV coinfection.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
TURQUOISE-I: SAFETY AND EFFICACY OF ABT-450/R/OMBITASVIR, DASABUVIR, AND RIBAVIRIN IN PATIENTS CO-INFECTED WITH HEPATITIS C AND HIV-1 Mark S. Sulkowski, Joseph J. Eron, David Wyles, Roger Trinh, Jay Lalezari, Jihad Slim, Joseph Gathe, Peter J. Ruane, Chia Wang, Richard Elion, Fritz Bredeek, Robert Brennan, Gary Blick, Amit Khatri, Krystal Gibbons, Yiran B. Hu, Linda Fredrick, Tami Pilot-Matias, Barbara Da Silva-Tillmann, Barbara McGovern, Andrew L. Campbell, Thomas Podsadecki 20th International AIDS Conference Melbourne, Australia 21 July 2014
Disclosures MS Sulkowski: Consultant/Advisory Board: AbbVie, BMS, Gilead, Idenix Pharmaceuticals, Janssen, Merck, Tobira Therapeutics; Data Safety Monitoring Board: Gilead (funds paid to Johns Hopkins University); Study Steering Committee: Pfizer; Grant/Research support: AbbVie, Boehringer Ingelheim, BMS, Gilead, Merck, Janssen, Vertex Pharmaceuticals (funds paid to Johns Hopkins University). JJ Eron: Grant/Research support: AbbVie, Merck, BMS, GSK/ViiV; Consultant; AbbVie, Gilead, BMS, GSK/ViiV, Merck, Janssen. D Wyles: Grant/Research support: AbbVie, BMS, Gilead, Merck, Vertex Pharmaceuticals; Consultant/Advisor: AbbVie, BMS, Gilead, Janssen. J Lalezari: Research support: AbbVie. J Slim: Speaker Bureau: AbbVie, BMS, Gilead, Merck, Janssen, Genentech. J Gathe: Grant/Research support: AbbVie, Tobira, Boehringer Ingelheim, BMS, GSK, Parexel, Gilead, Huesped. PJ Ruane: Grant/Research support: AbbVie, BMS, Gilead, Merck, Idenix, ViiV, Janssen; Consultant/Advisor: AbbVie, Merck, Gilead: Speaker: Gilead, ViiV, Merck. C Wang: Nothing to disclose. R Elion: Grant/Research support: AbbVie, Merck, BMS, GSK/ViiV, Gilead; Consultant: Gilead, BMS, GSK, ViiV; Speakers bureau: BMS, Merck, ViiV, Gilead, Janssen. F Bredeek: Grant/Research support: AbbVie, BMS, Gilead, Merck, Sumagen, ViiV; Consultant/Advisor: AbbVie, Merck, ViiV. R Brennan: Grant/Research support: AbbVie, Pfizer, Cubist Pharmaceuticals Inc, Achillion, Sanofi Pasteur, ViiV, GSK. G Blick: Grant/Research support: AbbVie, Gilead Sciences, Pfizer, Sangamo Biosciences, ViiV; Consultant/Advisor: BMS, Merck, Serono, ViiV; Speaker: AbbVie, Auxilium, BMS, Merck, Serono, ViiV. R Trinh, A Khatri, K Gibbons, YB Hu, L Fredrick, T Pilot-Matias, B Da Silva-Tillmann, B McGovern, AL Campbell, and T Podsadecki: Employees of AbbVie and may hold stock or options. The design, study conduct, analysis, and financial support of the clinical trials were provided by AbbVie. AbbVie participated in the interpretation of data, review, and approval of the presentation. All authors had access to all relevant data. This presentation contains information on the investigational products ABT-450/r, ombitasvir (ABT-267), and dasabuvir (ABT-333) and investigational use of ribavirin. 2 TURQUOISE-I: Safety and Efficacy of ABT-450/r/Ombitasvir, Dasabuvir, and Ribavirin in Patients Co-Infected with Hepatitis C and HIV-1 | AIDS 2014 | 21 July 2014
Background Coinfection with HCV occurs in 20 40% of persons living with HIV HCV/HIV coinfection is associated with more rapid liver disease progression2 Liver-related disease is a leading cause of morbidity and mortality in HCV/HIV coinfected patients in the era of ART1 The addition of direct-acting antivirals to pegIFN/ribavirin (RBV) has improved sustained virologic response (SVR) rates, but these regimens are associated with the well-known treatment-limiting toxicities of IFN- based therapy3-5 IFN-free regimens have shown promise with higher SVR rates and an improved safety profile 1Kitahata MM, et al. N Engl J Med. 2009;360:1815-26. 3Sulkowski MS, et al. Lancet Infect Dis. 2013;13:597-605. 4Sulkowski MS, et al. Ann Intern Med. 2013;159:86-96. 5Rodriguez-TorresM, et al. IDWeek 2013. 2Martin-Carbonero L, et al. Clin Infect Dis. 2004;38:128-33. 3 TURQUOISE-I: Safety and Efficacy of ABT-450/r/Ombitasvir, Dasabuvir, and Ribavirin in Patients Co-Infected with Hepatitis C and HIV-1 | AIDS 2014 | 21 July 2014
3 Direct-Acting Antiviral Regimen (3D) The multi-targeted 3D regimen includes: ABT-450, a potent NS3/4A protease inhibitor (identified by AbbVie and Enanta) co-dosed with low-dose ritonavir* (ABT-450/r) to increase the peak, trough, and overall drug exposures of ABT-450, enabling once daily dosing6 Ombitasvir (ABT-267), a potent NS5A inhibitor Dasabuvir (ABT-333), a non-nucleoside NS5B RNA polymerase inhibitor ABT-450, ritonavir, and ombitasvir are co-formulated as a single tablet Extensive phase 1 drug-drug interaction studies in healthy volunteers with tenofovir, emtricitabine, atazanavir, and raltegravir indicated no clinically meaningful alterations in HCV or HIV drug exposures *Ritonavir does not have antiviral activity against HCV. 6Menon R, et al. HepDART 2009. 4 TURQUOISE-I: Safety and Efficacy of ABT-450/r/Ombitasvir, Dasabuvir, and Ribavirin in Patients Co-Infected with Hepatitis C and HIV-1 | AIDS 2014 | 21 July 2014
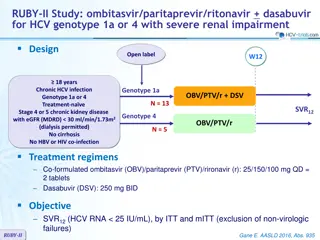
3 Direct-Acting Antiviral Regimen (3D) The 3D regimen, with and without RBV, has been studied in >2700 patients to date High SVR12 rates were achieved with 3D + RBV in genotype (GT) 1- infected patients within a phase 3 program 96% SVR12 in treatment-na ve and -experienced patients after 12 weeks of treatment7-10 92 96% SVR12 in treatment-na ve and -experienced patients with cirrhosis treated for 12 or 24 weeks11 TURQUOISE-I is a 2-part, multicenter, phase 2/3 study assessing the safety and efficacy of 3D + RBV in HCV GT1/HIV-1 coinfected patients, including those with cirrhosis 7Feld JJ, et al. N Engl J Med. 2014;370:1594-603. 9Zeuzem S, et al. N Engl J Med. 2014;370:1604-1614. 11Poordad F, et al. N Engl J Med. 014;370:1973-82. 8Ferenci P, Bernstein D, et al. N Engl J Med. 2014;370:1983-92. 10Andreone P, et al. Gastroenterology. 2014;doi:10.1053/j.gastro.2014.04.045. 5 TURQUOISE-I: Safety and Efficacy of ABT-450/r/Ombitasvir, Dasabuvir, and Ribavirin in Patients Co-Infected with Hepatitis C and HIV-1 | AIDS 2014 | 21 July 2014
TURQUOISE-I: Part 1 Study Design (N = 63) All patients will be followed for 48 weeks after HCV treatment end Open-label Treatment SVR12 3D + RBV (N = 31) SVR4 3D + RBV (N = 32) Week 24 Week 36 Day 1 Week 12 3D: coformulated ABT-450/r/ombitasvir, 150 mg/100 mg/25 mg QD; dasabuvir, 250 mg BID RBV: 1000 or 1200 mg daily according to body weight in 2 divided doses (<75 kg and 75 kg, respectively) 6 TURQUOISE-I: Safety and Efficacy of ABT-450/r/Ombitasvir, Dasabuvir, and Ribavirin in Patients Co-Infected with Hepatitis C and HIV-1 | AIDS 2014 | 21 July 2014
TURQUOISE-I: Study Analyses Efficacy analyses Rapid virologic response (RVR; week 4 of treatment) End-of-treatment response (EOTR; week 12 or 24 of treatment) Sustained virologic response (SVR4 and SVR12; post-treatment week 4 and 12, respectively) On-treatment HCV virologic failure Post-treatment HCV viral relapse Safety analyses Maintenance of plasma HIV-1 RNA suppression Treatment-emergent adverse events On-treatment lab abnormalities Virologic response is defined as HCV RNA <LLOQ (25 IU/mL) 7 TURQUOISE-I: Safety and Efficacy of ABT-450/r/Ombitasvir, Dasabuvir, and Ribavirin in Patients Co-Infected with Hepatitis C and HIV-1 | AIDS 2014 | 21 July 2014
TURQUOISE-I: Key Eligibility Criteria 18 to 70 years of age BMI 18 and <38 kg/m2 HCV GT1 infection (plasma HCV RNA >10,000 IU/mL) HCV treatment-na ve or pegIFN/RBV-experienced For pegIFN/RBV-experienced, prior: Relapse*, Partial response , or Null response Child-Pugh A Cirrhosis HIV-1 infected Plasma HIV-1 RNA <40 copies/mL CD4+ count 200 cells/mm3 or CD4+% 14% Stable atazanavir or raltegravir-inclusive ART regimen *Relapse: HCV RNA undetectable at or after the end of treatment, but with a detectable level within 52 weeks thereafter Partial response: >2 log10 IU/mL HCV RNA reduction at treatment week 12 but detectable at end of treatment Null response: <2 log10 IU/mL or <1 log10IU/mL HCV RNA reduction at treatment week 12 or 4, respectively 8 TURQUOISE-I: Safety and Efficacy of ABT-450/r/Ombitasvir, Dasabuvir, and Ribavirin in Patients Co-Infected with Hepatitis C and HIV-1 | AIDS 2014 | 21 July 2014
TURQUOISE-I: Baseline Demographics and Disease Characteristics 12-Week Arm (N = 31) 29 (94) 7 (23) 50.9 6.0 6 (19) 26 (84) 27 (87) 6.54 0.57 24-Week Arm (N = 32) 29 (91) 8 (25) 50.9 8.3 6 (19) 25 (78) 29 (91) 6.60 0.78 Male, n (%) Black, n (%) Age, mean SD Cirrhosis, n (%) IL28B non-CC genotype, n (%) HCV genotype 1a, n (%) HCV RNA (log10 IU/mL), mean SD Prior pegIFN/RBV experience, n (%) Na ve Relapse Partial response Null response CD4+ T-cell count/mm3, mean SD Atazanavir HIV-1 ART regimen Raltegravir HIV-1 ART regimen 20 (65) 1 (3) 5 (16) 5 (16) 633 236 16 (52) 15 (49) 22 (69) 3 (9) 2 (6) 5 (16) 625 296 12 (38) 20 (63) 9 TURQUOISE-I: Safety and Efficacy of ABT-450/r/Ombitasvir, Dasabuvir, and Ribavirin in Patients Co-Infected with Hepatitis C and HIV-1 | AIDS 2014 | 21 July 2014
3D + RBV Regimen TURQUOISE-I Results: ITT Virologic Response Rates 12-Week Arm 24-Week Arm 100 100 96.8 96.9 93.5 96.9 93.5 100 80 % Patients 60 40 20 30 31 31 31 32 32 31 32 0 RVR (Week 4) EOTR SVR4 SVR12 (Week 12 or 24) 10 TURQUOISE-I: Safety and Efficacy of ABT-450/r/Ombitasvir, Dasabuvir, and Ribavirin in Patients Co-Infected with Hepatitis C and HIV-1 | AIDS 2014 | 21 July 2014
3D + RBV Regimen TURQUOISE-I Results: ITT Virologic Response Rates 12-Week Arm 24-Week Arm 100 100 96.8 96.9 93.5 96.9 93.5 100 80 % Patients 60 40 20 30 31 29 31 31 32 29 31 31 31 32 32 31 32 0 RVR (Week 4) EOTR SVR4 SVR12 (Week 12 or 24) 11 TURQUOISE-I: Safety and Efficacy of ABT-450/r/Ombitasvir, Dasabuvir, and Ribavirin in Patients Co-Infected with Hepatitis C and HIV-1 | AIDS 2014 | 21 July 2014
TURQUOISE-I: Reasons for Non-Response Virologic failure occurred in 2 patients; both were prior null responders with HCV genotype 1a infection and had compensated cirrhosis Each had resistance-associated variants in at least 2 targets at the time of virologic failure not present at baseline HCV GT 1a IL 28B GT T/T Regimen Duration 12 wks Type of Variants at Time of Failure Patient 1 Virologic Failure Relapse at PT Week 2 Breakthrough at Week 16 NS3 D168V NS5A M28T NS5B S556G 2 1a T/T 24 wks None Q30R S556G 1 patient (12-week Arm) withdrew consent but had an undetectable HCV RNA at last study visit (week 10) No patient discontinued due to adverse events 12 TURQUOISE-I: Safety and Efficacy of ABT-450/r/Ombitasvir, Dasabuvir, and Ribavirin in Patients Co-Infected with Hepatitis C and HIV-1 | AIDS 2014 | 21 July 2014
TURQUOISE-I: Treatment-Emergent Adverse Events 10% 12-Week Arm (N = 31) 28 (90.3) 0 18 (58.1) 5 (16.1) 5 (16.1) 6 (19.4) 4 (12.9) 6 (19.4) 2 (6.5) 5 (16.1) 1 (3.2) 24-Week Arm (N = 32) 28 (87.5) 0 12 (37.5) 7 (21.9) 6 (18.8) 4 (12.5) 5 (15.6) 2 (6.3) 5 (15.6) 1 (3.1) 4 (12.5) Event, n (%) Any AE Serious AE Fatigue Insomnia Nausea Headache Upper respiratory tract infection Pruritus Cough Ocular icterus Diarrhea The majority of adverse events were mild or moderate in severity 5 severe adverse events were reported: insomnia, hypophosphatemia, disseminated herpes zoster, tooth abscess, and vertigo No treatment-emergent serious adverse events were reported 13 TURQUOISE-I: Safety and Efficacy of ABT-450/r/Ombitasvir, Dasabuvir, and Ribavirin in Patients Co-Infected with Hepatitis C and HIV-1 | AIDS 2014 | 21 July 2014
TURQUOISE-I: On-Treatment Laboratory Abnormalities 12-Week Arm (N = 31) 4 (12.9) 0 11 (35.5) 0 0 24-Week Arm (N = 32) 3 (9.4) 0 6 (18.8) 0 1 (3.1) Parameter, n (%) Hemoglobin <10 g/dL Hemoglobin <8 g/dL Total bilirubin >3X ULN ALT >5X ULN AST >5X ULN 6 patients reduced RBV dose due to hemoglobin declines; all achieved SVR Indirect hyperbilirubinemia was the most common laboratory abnormality 15/17 (88.2%) patients experiencing grade 3 total bilirubin elevations were receiving atazanavir-inclusive ART 5 patients (2 in the 12-week Arm, and 3 in the 24-week Arm) had a confirmed HIV-1 RNA 40 copies/mL (but <200 copies/mL) during the treatment period All 5 patients achieved plasma HIV-1 RNA re-suppression while maintaining the same HIV-1 ART regimen without 3D + RBV interruption 14 TURQUOISE-I: Safety and Efficacy of ABT-450/r/Ombitasvir, Dasabuvir, and Ribavirin in Patients Co-Infected with Hepatitis C and HIV-1 | AIDS 2014 | 21 July 2014
TURQUOISE-I: Summary This study evaluated the IFN-free 3D + RBV regimen in HCV treatment- na ve and experienced patients coinfected with HIV-1, including those with cirrhosis: SVR12 rate of 93.5% was achieved with 12 weeks of 3D + RBV SVR4 rate of 96.9% was achieved with 24 weeks of 3D + RBV 3D + RBV coadministered with atazanavir or raltegravir ART was well-tolerated with no treatment-emergent serious adverse events and no patient discontinuations due to adverse events These results are consistent with those in HCV GT1-monoinfected populations receiving the 3D + RBV regimen 15 TURQUOISE-I: Safety and Efficacy of ABT-450/r/Ombitasvir, Dasabuvir, and Ribavirin in Patients Co-Infected with Hepatitis C and HIV-1 | AIDS 2014 | 21 July 2014
TURQUOISE-I: Next Steps A cohort of patients on a stable darunavir-inclusive ART regimen who will receive treatment with the 3D + RBV regimen for 12 weeks (Part 1b) will be evaluated TURQUOISE-I, Part 2 will be conducted globally and will initiate later this year 16 TURQUOISE-I: Safety and Efficacy of ABT-450/r/Ombitasvir, Dasabuvir, and Ribavirin in Patients Co-Infected with Hepatitis C and HIV-1 | AIDS 2014 | 21 July 2014
Acknowledgements The authors would like to express their gratitude to the patients and their families, investigators, and coordinators who made these studies possible. The authors thank AbbVie employees Christine Collins, Sandra Lovell, Rakesh Tripathi, Martin King, Karmin Robinson-Morgan, Gretja Schnell, Jill Beyer, and Thomas Reisch for contributions to the study. Medical writing support was provided by Douglas E. Dylla, an employee of AbbVie. 17 TURQUOISE-I: Safety and Efficacy of ABT-450/r/Ombitasvir, Dasabuvir, and Ribavirin in Patients Co-Infected with Hepatitis C and HIV-1 | AIDS 2014 | 21 July 2014