The UK 100,000 Genomes Project: Views and Experiences of Patients
"The UK 100,000 Genomes Project explores the expectations and experiences of patients recruited, aiming to enable scientific discovery and insights for rare diseases. The project involves whole-genome sequencing of NHS patients and family members, with a focus on ethical considerations and decision-making processes around additional findings."
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
The UK 100,000 genomes project: views, expectations, and experiences of the first patients recruited Dr Sandi Dheensa, A. Lucassen, A. Fenwick, G. Crawford Clinical Ethics and Law, Faculty of Medicine University of Southampton, Southampton, United Kingdom. Clinical ethics and law Southampton: www.soton.ac.uk/cels
100,000 genomes project WGS of National Health Service patients with rare diseases + two family members (trios) Organised and delivered by Genomics England (company set up by UK Dept of Health) Aims to enable new scientific discovery and medical insights kick-start UK genomics industry set up genomic medicine service for NHS Research-practice hybrid 2 Clinical ethics and law Southampton: www.soton.ac.uk/cels
Before giving their blood sample Phone-call from co- ordinator 2-hour consent discussion Referral from own Dr Information sheets 3 Clinical ethics and law Southampton: www.soton.ac.uk/cels
100,000 genomes project My team: Practical Ethics GeCIP What are the ethical and social implications? Investigation of why people participate and their experiences and expectations of the project as a whole Decision-making around additional findings 4 Clinical ethics and law Southampton: www.soton.ac.uk/cels
Method Survey with 95 participants (patients/parents) Longitudinal semi-structured interviews 14 interviews n=9 with mothers of patient n=3 with parents of patient n=2 with adult patients Observations of consent sessions Focus groups with healthcare professionals involved in consent 5 Clinical ethics and law Southampton: www.soton.ac.uk/cels
Overview of findings Trust Reciprocity? Altruism Participation Hope 6 Clinical ethics and law Southampton: www.soton.ac.uk/cels
'Consent' is not informed Overwhelmingly positive experiences but Poor understanding of genetics/genomics and WGS processes: P3: I asked all the questions I needed to at the time, but it s pretty vague ..they took blood. The only thing I don t remember them taking is my DNA (M, aged 61+, undiagnosed muscle disease) Written information was unclear and difficult to understand: P8: I m quite sure that no-one other than medical people had proofread it... (M, aged 61+, undiagnosed muscle disease) 7 Clinical ethics and law Southampton: www.soton.ac.uk/cels
Trust in the health service Mother (P13): There s so much...some of the bits that if I didn t fully understand, it wasn t a case of, 'okay I m going to go off and read this and understand it', it was more like, 'I m trusting, I m handing her over to the experts on this'. (teen daughter, suspected Angelmann) Echoes previous research ( Genetic Alliance: Genome sequencing: What do patients think? 2015) 8 Clinical ethics and law Southampton: www.soton.ac.uk/cels
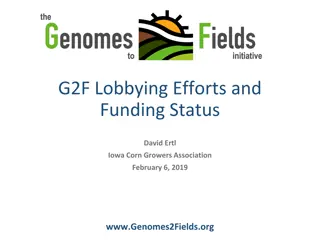
Hope (and to a lesser extent, altruism) Many wanted a clinical diagnosis. Others wanted to contribute to 'greater good ; feelings of solidarity with others Mother (P17): it can be a very lonely place (Undiagnosed 17 y.o) But deeper digging--at the root of this was still a hope that there would (ultimately) be clinical benefit for themselves/their family; I: If it won t help your son, why do you care about helping other children in the future? Mother (P1): It might help my son in the future by understanding his condition better...not a cure but better treatment. So I think it will help my son further down the line [4 y.o son with suspected AHC] 9 Clinical ethics and law Southampton: www.soton.ac.uk/cels
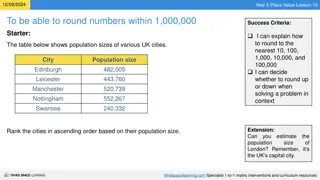
Hope (and to a lesser extent, altruism) Primary reason 80 70 60 50 40 30 20 10 0 Get diagnosis Participate in research Additional findings 10 Clinical ethics and law Southampton: www.soton.ac.uk/cels
Concerns: what next for results? Mother (P11): I feel a bit in the dark. My fear is, we re not going to be forgotten about are we? They would be keen to follow it through would they? We ve had that consent interview, now what? (Daughter with suspected hereditary breast cancer) Worries that diagnosis would not be a happy one (biographical disruption: Bury, 1980) Most knowledgeable should give them results: not necessarily person they had best relationship with. How will this work as genomics is mainstreamed? Reciprocity? 11 Clinical ethics and law Southampton: www.soton.ac.uk/cels
Discussion: summary of findings As per previous research, perception of relationships influenced consent (Kelly et al., 2015 relationships with researchers here relationship with NHS). Consent isn't informed and perhaps not voluntary Is that a 'bad thing'? Should we question decisions to participate? Or is being informed impossible? Should we rethink consent to take into account values such as trust? This trust warrants something in return: reciprocity promotes transparency, fairness, autonomy (Lunshof et al., 2014) Kelly, Susan E., et al. Evaluating the consent preferences of UK research volunteers for genetic and clinical studies."PloS one 10.3 (2015): e0118027; Lunshof, Jeantine E., George M. Church, and Barbara Prainsack. Raw personal data: providing access. Science 343.6169 (2014): 373-374. 12 Clinical ethics and law Southampton: www.soton.ac.uk/cels
Next steps: promoting trust and reciprocity Could an electronic health record help? Others areas of medicine suggest so (e.g. Giardina et al., 2014) NHS first electronic health record ('My Medical Record' ) launched in University Hospitals Southampton What tools can be integrated to improve communication? Interactive apps; patient-HCP messaging; communication plan Giardina, Traber Davis, et al. Patient access to medical records and healthcare outcomes: a systematic review. Journal of the American Medical Informatics Association 21.4 (2014): 737-741. 13 Clinical ethics and law Southampton: www.soton.ac.uk/cels
Acknowledgements Clinical Ethics & Law at Southampton -> ..and other collaborators and colleagues for inspiring discussions University Hospitals Southampton staff for recruitment And all participants. Clinical ethics and law Southampton: www.soton.ac.uk/cels