Thyroid Function in Pregnancy: Changes and Implications
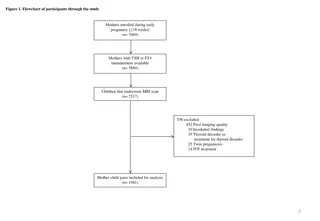
Control of thyroid function, physiological changes in pregnancy, shifts in thyroid hormones, and their impact on maternal and fetal health discussed in detail.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Thyroid and pregnancy Thyroid and pregnancy
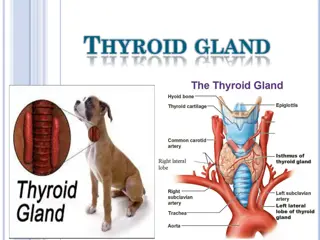
Control of Thyroid Function Hypothalamus releases TRH Act on the pituitary gland to release TSH TSH causes the thyroid gland to release the thyroid hormones (T3 and T4) TRH and TSH concentrations are inversely related to T3 and T4 concentrations. 99% circulating T3 and T4 is bound to TBG. 1% free form Biologically Active
Physiologic Changes in Pregnancy Pregnancy is a state of relative iodine deficiency, because: - Active transport to fetoplacental unit - Increase iodine excretion in urine, 2 fold (increased GFT & decreased renal tubular reabsorption) - Thyroid gland increases its uptake from the blood
TBG - Increase (hepatic synthesis is increased) TT4 & TT3 - Increase to compensate for this rise FT4 & FT3 (crosses the placenta in the 1st half of pregnancy) - Decrease. FT4 are altered less by pregnancy, but do fall little in the 2nd & 3rd trimesters. TSH (does not cross placenta) - decreases in 1st trimester, between 8 to 14 wks HCG, HCG has thyrotropin-like activity - Increase in 2nd & 3rd trimester (Increased TBG)
Thyroid hormones in pregnancy Maternal Thyroid volume increases by 10 20% with increased vascularity and a rise in thyroglobulin during pregnancy. Hepatic synthesis of thyroid-binding globulin (TBG) is increased with increase in total T4 and T3 concentrations Levels of free T4 and free T3 may rise in the first trimester, due to a hCG thyrotropic effect, but then remain in the normal range TSH is usually within normal limits in pregnancy but can be suppressed particularly in the first trimester because there is a negative correlation that exists between TSH and hCG levels in the first half of pregnancy TSH receptor antibodies may cross the placenta when present in high concentrations but the titre decreases with the progression of pregnancy.
Fetal TRH & TSH synthesis by 8 10 weeks Thyroid hormone synthesis by 10 12 weeks TSH, TBG, free T4 and T3 increase throughout gestation Maternal TSH does not cross the placenta Maternal T4 and T3 does cross the placenta in small quantities for early fetal growth.
Hyperthyroidism Hyperthyroidism Causes of maternal hyperthyroidism: Graves disease (90% of cases) toxic nodule toxic multinodular goitre hydatiform mole hyperemesis gravidarum.
Maternal & fetal outcomes are worse in cases of uncontrolled hyperthyroidism, with higher rates of: pre-eclampsia thyroid storm and thyrotoxic heart failure fetal growth restriction prematurity stillbirths fetal or neonatal thyrotoxicosis neonatal hypothyroidism
Treatment Medications: carbimazole (CBZ), methiamazole (MMI) or propylthiouracil (PTU), cross the placenta, but PTU less so than CBZ and MMI. Surgery is rarely performed in pregnancy, possibly if drug resistance or serious side effects with antithyroid drugs, e.g. agranulocytosis. Radioactive iodine treatment is contraindicated during pregnancy and should be avoided for at least 6 months after treatment.
Hypothyroidism Hypothyroidism
Clinical / Subclinical Hypothyroidism Serum TSH level > 3.0 mIU/l Subclinical hypothyroidism elevated TSH with normal FT4, FT3. Clinical Hypothyroidism Subclinical Hypothyroidism TSH High (>10) High (>3 - <10) Free T4 Low Normal Free T3 Normal or low Normal
Epidermiology Overt hypothyroidism complicates up to 3 of 1,000 pregnancies Subclinical hypothyroidism is estimated to be 2-5 % (Canaris GH, 2000)
Symptoms of Hypothyroidism Slowing of metabolic processes: Lethargy/fatigue weight gain cognitive dysfunction cold intolerance constipation bradycardia delayed relaxation of tendon reflexes slow movement and slow speech Deposition of matrix substances: Dry skin hoarseness edema puffy face and eyebrow loss peri-orbital edema enlargement of the tongue Others Decreased hearing myalgia and paresthesia depression menorrhagia arthralgia pubertal delay galactorrhea
Overlapping Complaints Symptoms Hypothyroidism Pregnancy Fatigue Constipation Hair Loss Dry Skin Brittle Nail Weight Gain Fluid Retention Bradycardia Carpel Tunnel Syndrome
Subclinical Hypothyroidism Elevated TSH (> 3.0 mIU/l) with normal FT4, FT3. 31 % with anti-TPO antibody More common on women with autoimmune diseases 50 % hypothyroidism in 8 years May cause childhood IQ decrease Increase in preterm 4% vs 2.5% in euthyroid mother (Casey BM, 2007)
Types of Hypothyroidism Primary hypothyroidism Secondary/tertiary hypothyroidism Iatrogenic Environmental
Primary Hypothyroidism Developed Countries Hashimoto s thyroiditis Chronic thyroiditis prone to develop postpartum thyroiditis Worldwide Iodine deficiency Other Causes: Subacute thyroiditis Thyroidectomy, radioactive iodine treatment
Hashimotos Thyroiditis An inflammatory disorder of thyroid gland More common on those with other autoimmune diseases Almost 100% associated with anti-TPO antibody. (Fitzpatrick & Russell) May cause transient hyperthyroidism PE: Goiter, rubbery consistency, moderate in size, mostly bilateral, painless.
Hashimotos Thyroiditis T cells recognize the patient s own thyroid antigens as foreign cytotoxic to thyroid epithelial cells stimulate B cells to make anti-thyroid antibodies, anti-peroxidase antibody, anti- thyroglobulin antibody, and anti-TSH-receptor antibody block the action of TSH, leading to hypothyroidism!!
Hashimotos Thyroiditis Lymphoid infiltrate, often with germinal centers
Iodine Deficiency Affect 38% of worldwide population (Pearce EN, 2008) Sources: Iodized salt and seafood. Others: cow milk, egg, beans Perinatal mortality Congenital cretinism (growth failure, mental retardation, other neuropsychological deficits) ACOG
Subacute Thyroiditis Subacute granulomatous thyroiditis - Painful - Fever, myalgia - Viral infection Subacute lymphocytic thyroiditis - includes postpartum thyroiditis (Prevalent: 5% ) - Painless Symptomatic Tx for initial hyperthyroidism
Secondary and Tertiary Hypothyroidism <1% hypothyroidism cases Low or normal serum TSH concentrations + low serum T4 and T3 2nd (TSH deficiency) hypothyroidism: - pituitary tumor - postpartum pituitary necrosis (Sheehan's syndrome) - trauma, infiltrative diseases. 3rd (TRH deficiency) hypothyroidism can be caused by - Damages the hypothalamus or - Interferes with hypothalamic-pituitary portal blood flow
Medication Cause Ferrous Sulfate GIT Absorption of thyroid hormone. Sucralfate Inhibit Cholestyramine Separated by 4 hours Aluminium Hydroxide
Overt hypothyroidism in pregnancy is rare In continuing pregnancies hypothyroidism is associated with increased risk of: Pre-eclampsia Placenta Abruption increased c-section rates Fetal death (especially if increased TSH occurs in 2nd trimester) Motherisk April 2007
More for the Baby!! Maternal thyroid hormones are important in embryogenesis No production until 12 weeks, therefore needs mom s T4 for fetal brain development Maternal hypothyroidism can cause negative effect on fetal intellectual development. Higher incidence of LBW (due to medically indicated preterm delivery, pre- eclampsia, abruption) Iodine deficient hypothyroidism -> congenital cretinism (growth failure, mental retardation, other neuropsychological deficits) Motherisk April 2007, CMAJ Apr 2007 176(8) Treatment before 10 weeks gestation adverse effect Treatment before 10 weeks gestation adverse effect No No
Indications for Screening universal screening is not recommended (ACOG) Family Hx of autoimmune thyroid disease Women on thyroid therapy Presence of goiter or thyroid nodules Hx of thyroid surgery Infertility Unexplained anemia or hyponatremia or high cholesterol level Previous Hx of - neck radiation - postpartum thyroid dysfunction - previous birth of infant with thyroid problem Other autoimmune chronic conditions: Type 1 DM
Laboratory Workup Overt hypothyroidism: symptomatic patient elevated TSH level low levels of FT4 and FT3 Subclinical hypothyroidism: asymptomatic patient elevated TSH normal FT4 and FT3
Treatment Replacement with external thyroid hormone -- levothyroxine (Levothyroid, Levoxyl, Synthroid, and Unithroid). Levothyroxine (Synthroid) pregnancy category A A sterioisomer of physiologic thyroxine 1.6 mcg/kg, usually about 50 to 100 mcg/day for women 30-60 minutes before eating breakfast.
Treatment and Goals The American Association of Clinical Endocrinologists recommends keeping the thyroid-stimulating hormone (TSH) level between 0.3 and 3.0 mIU/L. After readjustment of levothyroxine, observe 6-8 weeks Check TSH every trimester
Side Effects of L-Thyroxine : Rapid or irregular heartbeat Chest pain or shortness of breath Muscle weakness Nervousness Irritability Sleeplessness Tremors Change in appetite Weight loss
Pearls Safe in pregnancy and lactation Very little thyroxin crosses the placenta NO risk of thyrotoxicosis of fetus Patients who were on thyroxine therapy before pregnancy should increase the dose by 30% once pregnancy is confirmed (Bombrys et al, 2008) Keep TSH level between 0.3 and 3.0 mU/L. TSH should be monitored every trimester until delivery.
Overt hypothyroidism (OH) OH complicates 2 10 per 1000 pregnancies and is commonly due to: Hashimoto's thyroiditis previous radioiodine therapy/thyroid surgery previous postpartum thyroiditis hypopituitarism iodine deficiency.
Maternal and fetal outcomes are worse with OH higher risks of spontaneous miscarriage, PET,PIH, PPH & low birth weight. There is a risk of a slight reduction in IQ in the fetus but no increased risk of congenital malformations. Pregnancy itself probably has no effect on hypothyroidism although approximately 25% of women will require an increase in their thyroxine dose in pregnancy
Congenital cretinism is a well-documented syndrome of growth restriction, deafness and neuropsychological impairment, resulting from severe iodine deficiency or untreated congenital hypothyroidism. woman should be euthryoid at conception, on a stable dose of thyroxine and the importance of compliance during the first trimester should be emphasised.