Understanding Thyroid Gland Disorders and Functions
Explore the anatomy, physiology, and disorders of the thyroid gland, including hyperthyroidism and hypothyroidism. Learn about the role of the thyroid gland in hormone production and the hypothalamic-pituitary-thyroid axis. Discover the definitions, symptoms, causes, diagnosis, and treatment options for thyrotoxicosis. Dive deep into the complexities of thyroid health with Dr. Mousa Tuwati Alfakhri.
Download Presentation

Please find below an Image/Link to download the presentation.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author. If you encounter any issues during the download, it is possible that the publisher has removed the file from their server.
You are allowed to download the files provided on this website for personal or commercial use, subject to the condition that they are used lawfully. All files are the property of their respective owners.
The content on the website is provided AS IS for your information and personal use only. It may not be sold, licensed, or shared on other websites without obtaining consent from the author.
E N D
Presentation Transcript
Thyroid gland disorders Dr Mousa Tuwati Alfakhri
Objectives Thyroid gland,anatomy and physiology Thyroid function tests Hyperthyroidism hypothyroidism
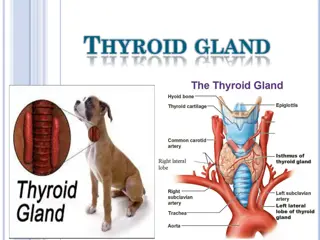
Anatomy Thyroid gland consists of two lateral lobes connected by isthmus. closely attached to thyroid cartilage and to upper end of trachea, and thus moves on swallowing. The gland has rich blood supply from superior and inferior thyroid arteries. thyroid gland consists of follicles lined by cuboidal epithelioid cells. Inside is colloid (the iodinated glycoprotein thyroglobulin) which is synthesized by follicular cells.
In the Thyroid Gland There the following 5 steps in the hormonogenesis 1. Trapping of inorganic Iodine from dietary Iodides 2. Activation of inorganic Iodine to active iodide I2 Incorporation of I2into Tyrosine of Thyroid Globulin to form MIT and DIT 3. 4. Coupling of formed MIT and DIT to form T4& T3 Proteolysis of Thyroglobulin to release T4& T3 5. 5
Thyroid gland secret mainly T4 (prohormone) 90% and only few T3 . In plasma more than 99% of all T4 and T3 is bound to hormone-binding proteins (thyroxine-binding globulin, TBG). Only free hormone is available for action in target tissues In peripheral tissue T4 is deiodinated and converted into T3 which is the active form
hypothalamic-pituitary-thyroid axis HYPOTHALAMUS - TRH ANT. PITUITARY - TSH TSH -R THYROID T4 and T3 PLASMA T4 + FT4 PLASMA T3 + FT3 TISSUES FT4 to FT3 7
Objectives Definitions Symptoms Signs Causes diagnosis Treatment
Definitions Thyrotoxicosis:Hypermetabolic state caused by thyroid hormone excess at the tissue level. Hyperthyroidism:Increased thyroid hormones synthesis and secretion. All patients with hyperthyroidism have thyreotoxicosis Not all patients with thyreotoxicosis are hyperthyroid
Symptoms of thyrotoxicosis Common symptoms Weight loss despite normal or increased appetite Heat intolerance sweating Palpitations tremor Dyspnoea fatigue Irritability emotional lability Less common symptoms Osteoporosis Diarrhoea Angina Anxiety, psychosis Muscle weakness Pruritus, alopecia Amenorrhoea/oligomenorrhoea Infertility, spontaneous abortion Loss of libido, impotence Excessive lacrimation
Signs of thyrotoxicosis common Signs Weight loss Tremor Palmar erythema Sinus tachycardia Lid retraction, lid lag Less common signs Goitre with bruit(graves disease) Atrial fibrillation Systolic hypertension increased pulse pressure Cardiac failure Hyper-reflexia Ill-sustained clonus Proximal myopathy Rare signs Gynaecomastia Spider naevi Onycholysis Pigmentation
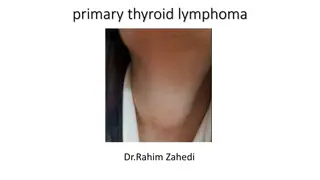
Causes of thyrotoxicosis Extrathyroidal source of thyroid hormone 0.02% Factitious thyrotoxicosis Struma ovarii(Ovarian teratoma containing thyroid tissue) Graves disease 80% Multinodular goitre 15% Solitary thyroid adenoma 5% TSH-induced 0.2% TSH-secreting pituitary adenoma. Choriocarcinoma and hydatidiform mole (Human chorionic gonadotrophin has thyroid-stimulating activity) Thyroiditis 3% autimmune Subacute (de Quervain s) Post-partum Iodide-induced 1% Drugs (amiodarone) Radiographic contrast media
Graves disease The most common cause of thyrotoxicosis (60-80%). Organ specific auto-immune disease The most important autoantibody is Thyroid Stimulating Immunoglobulin (TSI) acts as TSH and stimulates T4and T3 Other antibodies: Anti thyro peroxidase (anti-TPO) antibodies Anti thyro globulin (anti-TG) Associated with other Autoimmune diseases - Pernicious Anemia, T1DM RA, Myasthenia Gravis, Vitiligo, Adrenal insufficiency.
Epidemiology of Graves Disease Prevalence: 0.6% of population Incidence: 0.5/1000/year Female/male ratio: 5 10/1 Peak incidence: 30 60 years of age
Graves disease - pathogenesis Genetic and environmental factors Production of IgG antibodies (thyroid-stimulating immunoglobulins TSI or TSH-receptor antibodies TRAb) Stimulation thyroid hormone production and goitre formation
Precipitating And Predisposing Factors Genetic Susceptibility(15% of pts with Graves have a close relative with the same disorder) Stress :patients with Graves'hyperthyroidism give history of psychologic stress(loss of a spouse or road traffic accident) before onset of hyperthyroidism Gender( F:M 7:1) Smoking(relative risk approximately 2.0) and an even stronger risk factor for Graves' opthalmopathy Pregnancy (30% of women give history of pregnancy in 12 months before onset of G D ) Drugs(amiodarone, Interferon alpha,iodine)
Components of Graves disease Prevalence Feature Hyperthyroidism and goiter 95% Thyroid eye disease 50% Pretibial myxoedema 5% acropathy 1% Thyroid eye disease without hyperthyroidism [ Euthyroid Graves disease ] 5%
Goiter Symmetrically enlarged,with bruit on auscultation Neck uss :diffuse goiter with hypervascularity
Thyroid scintigraphy In graves disease diffuse Increase uptake of radioactive iodine
Thyroid Dermopathy Pretibial region Raised, light colored or yellow-reddish lesion with orange peel apperance .Sometimes pruritus
Thyroid Acropathy Clubbing and Osteoarthropathy
Thyroid Ophthalmopathy Proptosis Lid lag
Ophthalmopathy in Graves Periorbital edema and chemosis
Toxic Multinodular Goiter (TMG) TMG is the next most common hyperthyroidism - 20% More common in elderly individuals long standing goiter Milder manifestations (apathetic hyperthyroidism) Mild elevation of FT4and FT3 Progresses slowly over time Clinically multiple firm thyroid nodules Scintigraphy shows - hot and normal areas
Thyroid scintigraphy inTMG Alternate increase uptake(hot) and normal uptake areas
Sub Acute Thyroiditis (SAT) is the next most common hyperthyroidism 15% T4 and T3are extremely elevated in this condition Immune destruction of thyroid due to viral infection Destructive release of preformed thyroid hormone Thyroid gland is painful and tender on palpation Nuclear Scintigraphy scan - no RIU in the gland Leucocytosis and high ESR Treatment is NSAIDs and Corticosteroids
Toxic Single Adenoma (TSA) TSA is a single hyper functioning follicular thyroid adenoma. It is the cause in 5% of patients who are thyrotoxic Nuclear Scintigraphy scan shows only a single hot nodule TSH is suppressed by excess of thyroxines So the rest of the thyroid gland is suppressed
Thyroid Scintigraphy inToxic Single Adenoma single hot nodule
Diagnosis of thyrotoxicosis Investigation to confirm diagnosis of thyrotoxicosis Invetstigation to diagnose underlying cause
Investigation to confirm diagnosis of thyrotoxicosis In primary hyperthyroidism TSH is high T4 and T3 are high in about 5-10% of thyrotoxicosis T4 is normal and T3 is hight(T3 toxicosis) In TSH dependent causes(secondary thyrotoxicosis) of thyrtoxicosis such asTSH- secreting pituitary adenoma and Choriocarcinoma and hydatidiform mole TSH is high and free T3 and T4 are high
Subclinical thyrotoxicosis Serum TSH is undetectable, and serum T3 and T4 areat the upper end of the reference range. This combinationis most often found in older patients with multinodulargoitre. These patients are at increased risk of atrial fibrillation and osteoporosis annualis follow up, as the conversion rate to overt thyrotoxicosis is 5% each year.
Invetstigation to diagnose underlying cause Thyroid scintigraphy A thyroid scan, which can be done at the same time as the RAIU, helps to distinguish among high RAIU disorders Graves disease shows diffuse isotope uptake toxic multinodular goiter shows patchy uptake a toxic adenoma shows uptake only in a single nodule
Differential Diagnosis (with radioiodine uptake ) Low Silent thyroiditis Postpartum thyroiditis Subacute thyroiditis Iodine-induced hyperthyroidism Amiodarone-induced hyperthyroidism Iatrogenic hyperthyroidism Struma ovarii High or Normal Graves disease Toxic multinodular goiter Toxic adenoma HCG-induced hyperthyroidism TSH-producing pituitary tumor
Other investigations for underlying causes TSH-receptor antibodies (TRAb) (graves disease) thyroid-peroxidase antibodies (TPO) autoimmune thyroid disease(greves disease, Hashimoto thyroiditis ). thyroglobulin,erythrocyte sedimentation rate(subacute thyroiditis) human chorionic gonadotropin(Choriocarcinoma and hydatidiform mole )
Algorithm for Hyperthyroidism Measure TSH and FT4 TSH, FT4 N TSH, FT4 TSH, FT4 Primary (T4) Thyrotoxicosis Pituitary Adenoma Measure FT3 High T3 Toxicosis Features of Grave s Normal Sub-clinical Hyper Yes No RAIU Low RAIU F/u in 6-12 wks Rx. Grave s Sub Acute Thyroiditis, I2, Thyroxine Single Adenoma, MNG www.drsarma.in
GRAVES DISEASE TREATMENT General principles of treatment RADIOIODINE Treatments available for Graves disease SURGICAL MEDICAL
Medical treatment 1. Antithyroid drugs 2. blockers
blockers to decrease the sympathetic excess Propranalol, Atenelol, Metoprolol if blockers contraindicated calcium chanel blockers used
Antithyroid drugs Goal: Permanent remission of hyperthyroidism Limitations: High recurrence rate of hyperthyroidism Possible side effects
Anti Thyroid Drugs (ATD) Imp. considerations Methimazole Propylthiouracil Efficacy Very potent Potent Duration of action Long acting BID/OD Short acting QID/TID In pregnancy Contraindicated Safely can be given Mechanism of action Iodination, Coupling Iodination, Coupling Conversion of T4to T3 No action Inhibits conversion Rashes, Neutropenia Adverse reactions Rashes, Neutropenia Dosage 20 to 40 mg/ OD PO 100 to 150mg qid PO
Adverse effects of Antithyroid drugs Mild leukopenia (12 25%) Agranulocytosis (0.1 0.5%) Aplastic anemia Thrombocytopenia Cholestasis Hepatocellular necrosis Lupus-like syndrome Nephrotic syndrome
Radio Active Iodine (RAI Rx) Destruction of thyrocytes by -radiation The effect is less rapid than ATD or Thyroidectomy It is effective, safe, and does not require hospitalization. Very few adverse effects as no other tissue absorbs RAI Goal is to make the patient hypothyroid Never given for children and pregnant/ lactating women Not recommended with patients of severe Ophthalmopathy
Indications for radioiodine therapy Patient preference Poor-compliance with antithyroid drugs Recurrence after thyroidectomy Severe uncontrolled disease
Complcations Radioiodine Therapy Permanent hypothyroidism Transient hypothyroidism Thyroiditis Thyrotoxic crisis Possible exacerbation of ophtalmopathy (preventable by glucocorticoids)
Surgical treatment Total thyroidectomy is now considered the operation of choice because of the risk of relapse with partial thyroidectomy
Thyroid crisis or thyroid storm is Acute life threatening exacerbation of thyrotoxicosis rare condition, with a mortality of 10%, hyperpyrexia, severe tachycardia, extreme restlessness, cardiac failure and liver dysfunction. usually precipitated by stress, infection or surgery in an unprepared patient, or radioiodine therapy. Treatment is urgent Propranolol in full doses is started immediately together with potassium iodide, antithyroid drugs, corticosteroids